Cover was created by the transcriber and was placed in the public domain.
The Project Gutenberg EBook of A Text-book of Diseases of Women, by Charles Bingham Penrose This eBook is for the use of anyone anywhere in the United States and most other parts of the world at no cost and with almost no restrictions whatsoever. You may copy it, give it away or re-use it under the terms of the Project Gutenberg License included with this eBook or online at www.gutenberg.org. If you are not located in the United States, you'll have to check the laws of the country where you are located before using this ebook. Title: A Text-book of Diseases of Women Author: Charles Bingham Penrose Release Date: June 26, 2017 [EBook #54982] Language: English Character set encoding: UTF-8 *** START OF THIS PROJECT GUTENBERG EBOOK A TEXT-BOOK OF DISEASES OF WOMEN *** Produced by deaurider, Wayne Hammond and the Online Distributed Proofreading Team at http://www.pgdp.net (This file was produced from images generously made available by The Internet Archive)
1
2
3
Cover was created by the transcriber and was placed in the public domain.
 With 225 Illustrations
With 225 Illustrations
 SIXTH EDITION, REVISED
SIXTH EDITION, REVISED4
Set up, electrotyped, printed, and copyrighted July, 1897. Revised, reprinted,
and recopyrighted May, 1898. Reprinted December, 1899. Revised,
reprinted, and recopyrighted December, 1900. Revised, reprinted,
and recopyrighted July, 1901. Reprinted January, 1902.
Revised, reprinted, and recopyrighted, June, 1904.
Reprinted August, 1905. Revised, reprinted,
and recopyrighted March, 1908.
 Copyright, 1908, by W. B. Saunders Company.
Copyright, 1908, by W. B. Saunders Company.

 PRINTED IN AMERICA
PRINTED IN AMERICA
 PRESS OF
PRESS OF
W. B. SAUNDERS COMPANY
PHILADELPHIA
5
I have carefully revised this book for the sixth edition, and have made those changes and additions that have been rendered necessary by the increase of our knowledge of gynecology.
1720 Spruce Street, Philadelphia.
March, 1908.
6
7
I have written this book for the medical student. I have attempted to present the best teaching of modern gynecology, untrammelled by antiquated theories or methods of treatment. I have, in most instances, recommended but one plan of treatment for each disease, hoping in this way to avoid confusing the student or the physician who consults the book for practical guidance. I have, as a rule, omitted all facts of anatomy, physiology, and pathology which may be found in the general text-books upon these subjects. Such facts have been mentioned in detail only when it seemed important for the elucidation of the subject, or when there were certain points in the pathology that were peculiar to the diseases under consideration. I am indebted to Dr. H. D. Beyea for several pathological drawings, and to Dr. Wm. R. Nicholson for the preparation of the Index.
8
9
15
Gynecology is the study of diseases peculiar to women. As woman possesses organs which man has not, and as the parts—physiological and social—that she plays in life differ from those played by man, we should expect to find her afflicted with a certain number of diseases, peculiar to her, which are dependent upon her anatomy, physiology, and mode of life. Such diseases occur in barbarous as well as in civilized women; and similar diseases, peculiar to the female, occur in the lower animals. Thus, in the cow and the mare we find tumors of the vagina, prolapse of the vagina and uterus, fibroid tumors, sarcoma and cancer of the uterus, and some forms of ovarian cysts. Cysts of the tubes and the ovaries are exceedingly common in old mares; cats and goats are similarly affected.
From a pathological point of view, however, the civilized woman unfortunately differs from her barbarous sister, and from the female of the lower animals, in many important particulars. She is more liable to the pathological conditions which, more or less, all females have in common. These conditions appear in a more severe form, and are followed by more disastrous results, in the civilized than in the barbarous state.
The female among the lower animals and among 16 savages seems to be about equal in proportionate strength and physical endurance to the male, though in size and in gross muscular strength she may be his inferior. Her subordinate position is often due not so much to any difference in strength as to the fact that the male possesses weapons—as the horns of the deer—with which nature has not endowed the female; and though she is liable to more diseases than the male, yet her relative position does not seem to be materially altered by this fact. The bitch is as enduring as the dog. The female grizzly is as ferocious and as dangerous as the male. The mare is as fast as the horse. The squaw among the American Indians can lift and carry burdens which the lazy buck would not attempt.
How different it is with the civilized woman, as we know her in this country! The average healthy woman in this country is very much inferior in physical strength and endurance to the average man, and this inferiority is tremendously increased when she becomes sick from any of the diseases to which her sex is liable.
The increased liability of the civilized woman to disease is in a large measure due to her poor physique. But this is not all.
The causes of many of the diseases with which the gynecologist has to deal cannot be traced so easily.
Fibroid tumors of the uterus, which are so common among the colored women of this country, are said by Tait to be unknown among their African cousins, who are removed by but a few generations.
The most common causes of diseases of women are injuries received during parturition; sepsis; venereal diseases; errors of development; improper mode of life and clothing during the period of development; neglect during menstruation; and celibacy.
The results of the injuries received during parturition are most numerous. They may appear immediately, a short time after labor, or at some remote period. The disabilities attending laceration through the sphincter 17 ani or a recto-vaginal or vesico-vaginal fistula appear before the mother leaves her bed. The suffering from a laceration of the cervix, a subinvolution of the uterus, or a retrodisplacement may not be felt for some weeks or months after labor; while the still more remote result, the development of cancer, may not appear for many years, though it can be positively traced to the lesion in the cervix as the primary cause.
Septic infection of the genital tract kills or makes invalids of many women. The infection occurs at the time of a miscarriage or of a normal labor, or it may be acquired from the dirty instruments or the dirty hands of a physician. It is not a cause of disease among civilized women alone, but occurs among barbarous and semi-barbarous races.
Venereal disease, especially gonorrhea, has been said to be the most common cause of disease among women. The disease extends from the external genitals through the uterus and Fallopian tubes, causing sterility, chronic invalidism, and death from peritonitis.
Errors of development are frequent causes of disease and suffering among women. Atresia of the vagina or of the cervix uteri, by causing retention of the uterine discharges, produces most serious pathological conditions. Arrested development of the whole or of part of the uterus is a common cause of disease.
Improper clothing and an improper mode of life during the period of development are most fertile sources of diseases of women. Clothing which contracts the waist, as well as clothing which, though not unduly tight in the inactive state, yet interferes with abdominal respiration during activity, is most injurious. Such clothing diminishes the capacity of inspiration by restricting abdominal expansion, and thus crowds down the pelvic organs toward the pelvic floor; and the continuous support to the abdominal walls diminishes their natural muscular strength and places the woman in a condition predisposing to the various displacements of the uterus. 18
An improper mode of life, irregular hours for sleeping and eating, insufficient exercise, and lack of fresh air and sun, resulting in poor muscular development, seem to predispose the woman, as the man, to a variety of pathological conditions; but as the reproductive apparatus in woman is more delicately organized, and as, during the period of active life, this is really her chief part, it more especially suffers as a result of any general systemic derangement.
Neglect during menstruation, especially in the young girl, is a frequent cause of subsequent suffering. The effect of menstruation upon the whole system is remarkable. The nervous, vascular, and digestive systems all share in the menstrual function. The usual work of the girl at school or other employment should be altered to suit the altered conditions of her body at the menstrual period. Long school hours and close mental application or active exercise are too often continued at this time.
Celibacy is an unnatural state and a common cause of disease. Certain forms of fibroid tumors of the uterus are more common in single than in married women, and more common in sterile than in childbearing women. And the painful cirrhotic ovaries of the old maid are the result of the unceasing menstrual congestions never relieved by pregnancy and lactation. 19
In order to make a complete gynecological examination, we must examine the abdomen, the external organs of generation, and the pelvic structures.
Examination of the Abdomen.—In order to make a perfectly satisfactory examination of the abdomen, the woman should be in bed, with all clothing removed except the undershirt and the night-dress, which should be drawn well up above the costal margin. Examination made with any constricting clothing about the waist or about the lower thorax is most unsatisfactory.
The abdomen is examined by inspection, palpation, percussion, and auscultation.
The woman should lie flat upon her back, and the abdomen should be thoroughly exposed. We can then determine by inspection the presence of dilated veins or of lineæ albicantes, the general size and form of the abdomen, the occurrence of any abdominal movement, and the presence of any asymmetry in the abdominal contour, such as would be made by the bulge of a tumor or the displacement of an abdominal organ. The shape of the abdomen, even though symmetrical, is often diagnostic of certain intra-abdominal conditions. Thus, an abdominal enlargement that is due merely to fat presents a different contour from the enlargement caused by tympanitic distention of the intestine. The enlargement due to ascites, or free fluid in the peritoneum, differs in contour from that caused by an encysted collection of fluid.
It should be remembered that lineæ albicantes are not always the result of pregnancy, but that they may have 20 been caused by distention of the abdomen from some other cause.
Palpation.—We can determine most by palpation of the abdomen. The examiner should always remember that it is most important to secure the patient’s confidence, and to proceed so gently, slowly, and gradually in performing palpation that no voluntary or reflex contraction of the abdominal muscles may impede his manipulations.
In cases in which there is a sore or tender spot within the abdomen the contraction of the recti muscles may be altogether involuntary, persisting even when the patient is anesthetized. We see this in the rigid right rectus muscle of appendicitis. The hands should be warmed, and palpation should be performed with both hands. A certain amount of gentle stroking or massage of the abdomen will secure the patient’s confidence by making her feel that she will not be hurt by any sudden violent pressure, and will also prevent reflex contraction of the muscles. By proceeding in this way, slowly, the examiner can palpate the whole of the abdominal surface, exploring first the structures lying most anterior, and then, pressing the fingers more deeply, he can examine the more posterior structures.
Fluctuation in an encysted fluid accumulation is generally readily determined. While one hand is placed against one side of the fluid mass and the opposite side is percussed by the fingers of the other hand, the wave of fluctuation is easily felt. Sometimes a thrill or a false wave of fluctuation is observed in the subcutaneous fat of obese women. This disturbing element may, however, be eliminated by an assistant pressing the ulnar edge of his hand in the median line upon the abdominal surface, thus stopping the fat wave of fluctuation.
Special organs in the abdomen sometimes require special methods of examination. It is very often necessary for the gynecologist to examine the kidneys, because many women have movable or floating kidneys, and the 21 nervous, gastric, and abdominal symptoms may be due to this condition. The presence of a floating kidney may often be determined by inspection; the presence of a movable kidney, however, must be determined by palpation. This should be performed with the woman in the sitting, or standing, erect posture; or sitting upon the edge of a chair, with the body inclined somewhat forward and the hands upon the knees; or lying upon a bed, on the side opposite the kidney that is being examined. One hand should be placed over the lumbar muscles; the other hand should be placed upon the anterior abdominal wall immediately below the costal margin, and should be pressed backward. If the kidney lies below its normal position, it may in this way be brought between the two hands, and can be felt to glide upward as the hands are pressed together. In case a movable kidney cannot readily be found, because it may have returned to its normal position, it may often be brought down again if the woman is made to cough.
In a thin woman the vermiform appendix may sometimes be felt through the abdominal wall; and in cases of pain and inflammation in the right iliac region it is sometimes important to determine whether or not the trouble has started in the vermiform appendix or in the Fallopian tube. In order to palpate the vermiform appendix the examiner should stand upon the right side of the woman, who is lying upon her back, and should place the tips of the fingers of the right hand at about the junction of the upper and middle thirds of a line drawn from the middle of Poupart’s ligament to the umbilicus. By pressing backward firmly and gently, pulsations of the right common iliac artery may be felt; and then by drawing the hand directly outward it will pass over the different structures in this region lying between the palpating hand and the posterior abdominal wall. The appendix may often be felt, especially if it is indurated by inflammation.
Percussion of the abdomen should be performed with 22 the woman in the dorsal position; though, if the examiner suspects the presence of free fluid in the peritoneum, or ascites, much may be learned by percussing in different positions and noting the accompanying changes in the percussion-note.
Percussion should then be performed with the woman upon her back, upon the right side, upon the left side, sitting up, and upon the hands and knees. An encysted fluid accumulation will give practically the same result in percussion in all positions, while free fluid will gravitate to the most dependent portion.
Auscultation of the abdomen is best performed with the stethoscope. By it we may hear fetal heart-sounds, uterine souffle, placental bruit, peritoneal friction sounds, and the peristaltic sounds of the intestinal tract. All of these sounds are of importance, and the presence or absence of any of them may have an important bearing upon the diagnosis of the case.
Examination of External Genitals and Pelvic Structures.—To examine the external organs of generation and the pelvic viscera the woman should be placed upon a table. In some cases the physician may be obliged, for want of proper facilities or on account of the physical condition of the patient, to make his examination upon a bed. Such an examination, however, is never so satisfactory or so thorough as the examination made with the woman upon the examining-table. A great number of gynecological tables have been introduced. The one which seems to the writer the best, on account of its simplicity and the perfect relaxation of the abdominal muscles furnished by it, is shown in the accompanying illustration (Fig. 1). It is a plain wooden table, at the foot of which are attached the upright supports for holding the stirrups for the feet, such as have been devised by Dr. Edebohls. By this arrangement the feet and legs are supported without any effort on the part of the woman; when the buttocks are drawn well down to the foot of the table there is a certain amount of flexion 23 of the pelvis upon the trunk, and the most complete attainable relaxation of the abdominal muscles is secured.
When the woman has been placed in this position the examiner should investigate thoroughly, and in order, the following structures: The anus, the perineum, the labia majora, the nymphæ, the fourchette, the orifices of the ducts of the vulvo-vaginal glands, the hymen or its remains, the vestibule and the small glands of the vestibule, the external urinary meatus, and the clitoris.
To determine any pathological condition of these structures it is necessary that the physician should be familiar with the appearance in the normal woman, and to gain such essential knowledge we should avail ourselves of every opportunity offered to make a critical examination of the external genitals of women, going over all the different structures in order.
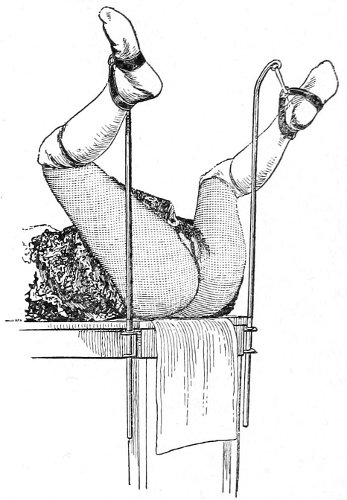
Fig. 1.—Woman in the dorsal position with feet supported in Edebohls’ stirrups.
Vaginal and Bimanual Examination.—Having examined and noted the condition of the external genitals, the physician should next proceed to examine the vagina. The index finger of the right or the left hand should be gently introduced into the vagina. The condition of the vaginal walls, and the direction, consistency, form, etc. of the vaginal cervix, may be determined. The shape and size of the os uteri should be noted. The ulnar edge and the tips of the fingers of the other hand should then be placed upon the abdomen, immediately above the symphysis pubis, and gently pressed backward and downward toward the vaginal finger 24 (Fig. 2). In this way the various pelvic organs, the uterus, Fallopian tubes, ovaries, and ureters, may be palpated between the two hands, and their position, size, shape, and consistency may be determined. Such an examination is, of course, made much more easily in a thin woman than in a fat one. A thin woman a few weeks after labor may be examined most easily, on account of the relaxation of the abdominal and vaginal walls.
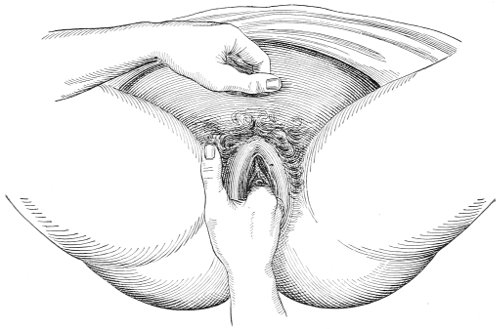
Fig. 2.—Bimanual examination.
This is called the bimanual method of examination, and the student will find that as he acquires practice in this method he will gradually depend less upon examination by the uterine sound and the speculum, and will rely altogether upon his sense of touch, his ability to palpate.
It matters not which hand be used in making the vaginal examination. It will, however, be found that the hand that is used the more frequently will become the more proficient.
In making the bimanual examination the structures 25 should be palpated methodically in order. The vaginal finger notes the condition of the cervix uteri. If the fundus be in the normal position, the uterus can then be taken between the abdominal hand (upon the fundus) and the vaginal finger (upon the cervix) (Fig. 3). The shape, size, mobility, and consistency are noted. The vaginal finger is then passed anteriorly and laterally toward either uterine cornu, while the abdominal fingers pass over to the posterior aspect of the same cornu. The ovarian ligament and the proximal end of the Fallopian tube may thus be felt. Passing farther outward, the whole of the tube and the ovary may be examined. The same procedure is then applied to the opposite side.
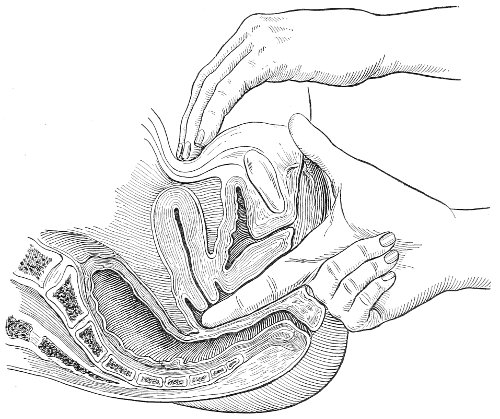
Fig. 3.—Bimanual examination; median sagittal section of the pelvis.
The condition of the ureters may be determined by placing the vaginal finger in either lateral vaginal fornix and drawing it outward and forward, when these structures will pass over the end of the finger. When the 26 ureters are indurated by inflammation they can be plainly felt.
By the method of examination here advised the physician will always make a visual examination before making a digital one. There are several advantages derived from this procedure. In the first place, no examination of a woman is thorough unless a careful visual examination of the external genitals has been made. The discovery of discharges and of lesions of the external genitals may throw much light upon the condition found higher up in the pelvis. Again, the examiner protects himself. A great many unfortunate cases of syphilis have been acquired by physicians from a primary sore upon the examining finger. A preliminary visual examination enables one to guard against this danger. The primary sore occurs upon the end of the examining finger or upon the web between the index and middle fingers—the part of the hand that is pressed against the fourchette.
The hands of the physician should, of course, be surgically clean before making an examination, and the grease or oil which is used as a lubricant should be clean. The hands should always be washed, after separating the parts to make the visual examination, before the finger is thrust into the vessel containing the lubricant. It is best to place a small portion of the lubricant on a plate or a saucer for each individual patient, and thus avoid the danger of contaminating the rest. Carbolized oil, borated vaseline or cosmoline, and a thick sterile solution of soap are good lubricants. Neutral green soap diluted with boiled water to the consistency of thin jelly is a very agreeable lubricant which may easily be washed from the hands and the vagina.
If practicable, the woman should receive a vaginal douche of bichloride-of-mercury solution, 1:4000, and the vulva should be washed, before making a bimanual examination. The examiner should always clean the external genitals of all discharges before introducing the vaginal finger. In this way we avoid the danger of 27 carrying septic material from the external genitals to the upper portion of the genital tract. This preliminary cleansing is not desirable before the external genitals have been examined; for much may be learned from observation of the discharges which bathe or escape from the various structures. If practicable, a cleansing vaginal douche of bichloride-of-mercury solution should be administered after the bimanual examination.
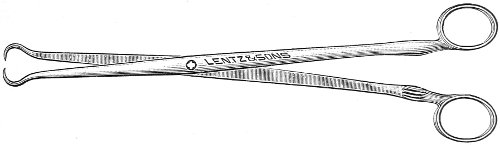
Fig. 4.—Double tenaculum.
The examination of the uterus and other pelvic structures is often facilitated by dragging the uterus downward with a tenaculum while the vaginal or the bimanual examination is being made. Sensation in the cervix is so slight that little or no pain is experienced in this procedure. The anterior or posterior lip of the cervix is caught with the single or the double tenaculum (Fig. 4), guided along the vaginal finger or introduced through the speculum, and the uterus is drawn down by an assistant in case the bimanual examination is being made, or by the external hand of the examiner in case a simple vaginal examination is made. When this is done the utero-sacral ligaments are made tense, and can be felt like two cords extending from the sides of the cervix outward and backward to the pelvic wall. The posterior surface of the uterus can be palpated often as high up as the fundus. The method is especially useful when the examination is made by the rectum, and in this way the whole posterior surface and the fundus of the uterus may be palpated (Fig. 5).
The contraindications to a vaginal examination are 28 virginity, the presence of a hymen, and any acute inflammatory or painful condition of the vulva or vagina. None of these conditions, however, forbid an examination if an exact diagnosis is essential to the proper treatment of the case, and can be made only in this way. It may be that in these cases a rectal examination will be sufficient for diagnosis.
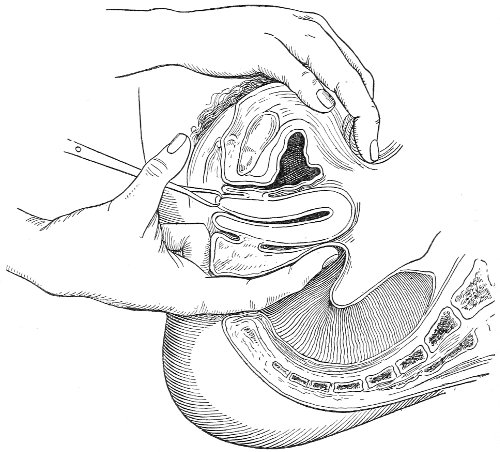
Fig. 5.—Bimanual examination with one finger in the rectum. The uterus is drawn down with the double tenaculum.
Rectal examination of the pelvic structures is made in a way similar to that already described for the vaginal examination. Bimanual examination may be made by palpating the various organs between the rectal finger and the abdominal hand.
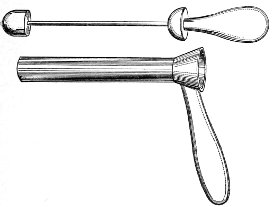
The Vaginal Speculum.—The speculum is an instrument through which a visual examination is made of the vagina, the external os uteri, and the vaginal cervix. A 29 great number of specula have been invented. At the present day the best two instruments of this class are the bivalve speculum, such as Goodell’s (Fig. 6), and the duck-bill speculum (Fig. 7), or perineal retractor, invented by Sims.
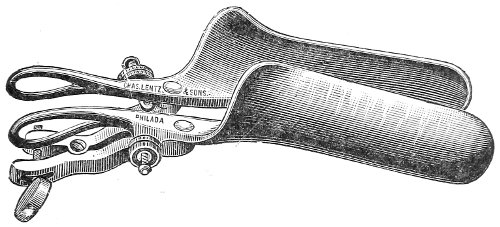
Fig. 6.—Goodell’s speculum.
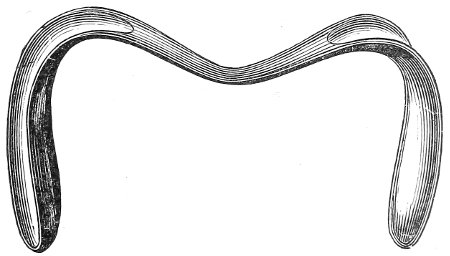
Fig. 7.—Sims’ speculum.

Fig. 8.—Sims’ depressor for the anterior vaginal wall.
The bivalve speculum is introduced with the woman upon her back, in the dorso-sacral position already described. The vulva and the vagina should be cleaned. The speculum should be warmed by placing it in hot water, and should then be lubricated with the soap solution or with vaseline. It should be introduced with the blades closed and the plane of the blades lying not exactly 30 in the median sagittal plane of the body, but inclined at a small acute angle to this plane, one edge of the speculum being directed toward either vaginal sulcus. The instrument is passed into the vagina toward the position in which, by a previous digital examination, the vaginal cervix had been found to lie. The instrument is then turned with the handles toward either thigh, so that the blades become parallel to the anterior and posterior vaginal walls, in order that, when separated, they will open the vaginal slit. The handles are brought together and the blades opened. When the vaginal cervix comes well into view the blades are fixed in place by the screws (Fig. 9).
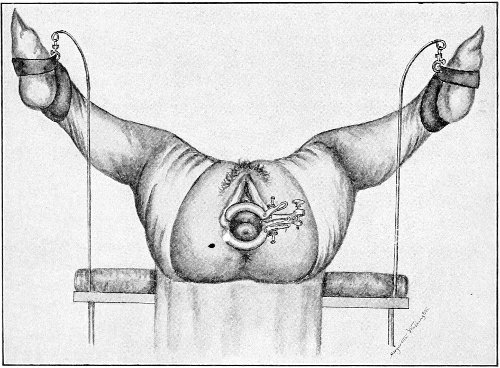
Fig. 9.—Goodell’s speculum in position.
In some cases, where the cervix points well forward or well backward, it may be readily brought into view through the speculum by catching it with a tenaculum.
By means of the bivalve speculum we are able to make a partial inspection of the vaginal walls, an imperfect inspection of the vaginal vault, and a good inspection of the vaginal cervix and the external os. Applications 31 can be made to the cervix, but none of the minor operations of gynecology can be performed through this speculum.
The Sims speculum enables us to make the most thorough inspection of the vagina, the vaginal vault, and the vaginal cervix. The Sims speculum is merely a hook or retractor for the perineum, and may be introduced with the woman in the dorsal position, the Sims position, or the genu-pectoral position. If the Sims speculum is introduced in the dorso-sacral position, it is necessary to hold forward the anterior vaginal wall in order to obtain a view of the cervix.
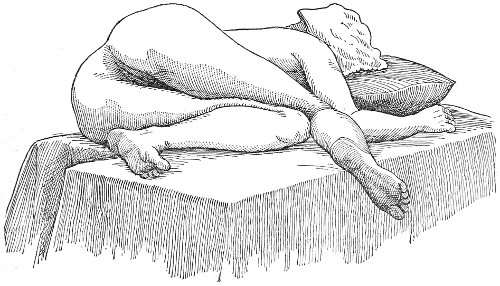
Fig. 10.—The Sims position.
The Sims position, which is also called the latero-abdominal position, is shown in Fig. 10. The woman is placed on the bed or table upon her left side. The side of the face is upon the pillow; the left arm is behind the back, so that the left breast rests upon the table. The thighs are flexed upon the abdomen at an angle of about 90° to the trunk. The right thigh is more flexed than the left, so that the right knee may touch the table above the left knee. The legs are flexed on the thighs. In this position there is a tendency for the intestines, following the force of gravity, to fall from the pelvis, 32 and for the uterus and other pelvic viscera to be drawn up. When the perineum is retracted with the blade of the Sims speculum, air will enter the vagina and the vaginal slit will become distended (Fig. 11). To facilitate inspection of the cervix it is usually necessary also to push forward the anterior abdominal wall by some kind of depressor, such as the one shown in Fig. 8.
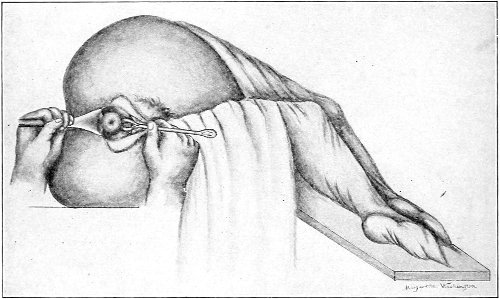
Fig. 11.—The cervix uteri exposed with the Sims speculum.
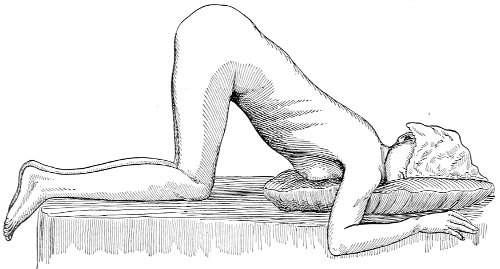
Fig. 12.—The knee-chest position.
The genu-pectoral position or the knee-chest position is shown in Fig. 12. The side of the face is upon the pillow; the breast is upon the table; the thighs are vertical. In 33 this position the intestines fall from the pelvis, and the other pelvic viscera are drawn upward by the force of gravity. If the anus is opened, air rushes in and distends the rectum. If the perineum is retracted, air enters and distends the vagina. If the urethra is opened, the bladder is likewise distended. The position is the most useful one for inspection of the rectum, vagina and vaginal cervix, and the bladder.
The Sims speculum, with the woman in the dorsal, the Sims, or the knee-chest position, is the most useful instrument by which to expose the cervix uteri for any of the minor operations of gynecology. The manipulations of the operator are not hampered by working between metal walls.
Examination of the Rectum.—If the woman is placed in the knee-chest position, a most satisfactory inspection of the whole of the rectum may be made. The woman should be placed in this position with the buttocks before a good light, and the posterior margin of the anus should be retracted by the small blade of a Sims speculum; the rectum will immediately become distended with air and the rectal walls will be well exposed. Or the rectal specula (Figs. 13, 14) may be used. In employing the longer of these instruments it is best to use light reflected from a head-mirror or thrown directly from an electric head-light into the speculum.
 |
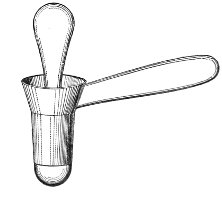 |
Fig. 13.—Rectal speculum, large size. |
Fig. 14.—Rectal speculum, small size. |
The instrument should always be introduced for the 34 first two inches with the obturator in place. The obturator should then be withdrawn and the speculum pushed farther in, the operator watching and guiding its course around the rectal valves or folds of mucous membrane, so as to prevent injury to the walls of the rectum. Anesthesia is not necessary for this procedure.
Examination of the Bladder.—It will readily be understood that all the hollow viscera are much more easily examined when their walls are separated by distention with air than when the walls are collapsed. The bladder is most readily examined in this way. The woman should be placed in the knee-chest position, or in the dorsal position with the hips elevated above the abdomen. In either position the intestines fall from the pelvis, and when the urethra is opened air enters and distends the bladder. This distention is most certainly accomplished in the knee-chest position. In women who are not very fat, however, the extreme dorso-sacral position is equally good. The details of this method of examination are described on a later page.
The uterine sound is an instrument by which the length of the uterine cavity may be determined (Fig. 15). The sound, which is a large surgical probe, somewhat curved to adapt itself to the normal shape of the uterine axis, is made of pliable metal, so that the curvature may be changed readily to suit any case. The sound is graduated, and at a position of 2½ inches from the tip is a small elevation marking the length of the normal uterine cavity.

Fig. 15.—Uterine sound.
The uterine sound was at one time used a great deal to determine the length and direction of the uterus, and 35 perhaps to assist in determining the character of the uterine contents or of the endometrium. With our present methods of examination, however, the sound is of but little if any use. The size and direction of the uterus can in nearly all cases be determined by bimanual examination. The use of the uterine sound is by no means free from danger. Many cases of septic endometritis and salpingitis have been caused by it, and the physician has often unintentionally committed an abortion by passing the sound in a pregnant woman. The uterine sound should never be used in a routine way. It should never be used unless one expects to determine with it something that cannot be determined by simpler methods of examination.
The most thorough aseptic precautions should be observed when the sound is introduced. The vulva, vagina, and cervix should be cleaned and the sound should be sterilized. The sound should never be introduced if there is any suspicion of pregnancy.
ANTISEPSIS—In all examinations the physician should observe every precaution to avoid carrying infection from one patient to another. All instruments used in the examination should be thoroughly cleansed with soap and warm water, and then boiled for five minutes in a 1-per cent. solution of carbonate of soda. 36
Vulvitis.—Vulvitis, or inflammation of the vulva, is not a common disease. The vulva is composed of several parts which are anatomically distinct, and, though all these parts are usually involved in an acute attack of inflammation of the vulva, yet the symptoms of the disease and the pathological appearance depend to a great extent upon the structures which are principally affected. The labia majora, the nymphæ, the vestibule with its mucous crypts or glands, the clitoris, the external urinary meatus, and the ducts of Bartholin’s glands may all be involved in the inflammation. The sebaceous glands of the labia may be especially involved, producing a form of sebaceous acne which has been called follicular vulvitis. Inguinal adenitis may accompany vulvitis.
The appearance of the parts is that characteristic of inflammation of the skin and mucous membrane in any other part of the body. The mucous membrane becomes red and swollen; the labia may become edematous; an abundant purulent discharge covers the parts, and unless cleanliness is practised the irritation from the discharge spreads to the inner aspects of the thighs, the perineum, and the anal region.
The patient suffers with local pain, which is increased by walking and by the passage or contact of urine.
The usual cause of vulvitis is gonorrhea. The condition is sometimes secondary to other diseases. It may be caused by the irritation from the discharges of a vesico-vaginal or recto-vaginal fistula, from a cancer of the cervix or in some forms of endometritis. Girls and 37 women who are unclean may be attacked by vulvitis as a result of irritation from decomposed smegma, sweat, urine, etc. The oxyuris, or thread-worm, may enter the vulva from the rectum and cause, in unclean children, sufficient irritation to produce inflammation. Vulvitis from uncleanliness is most likely to occur in hot weather after prolonged exercise. It not infrequently attacks children, especially those of a strumous diathesis, whose hygienic surroundings are poor. In such cases the suspicions of the parents may demand a medico-legal examination; and it is of importance to remember that vulvitis of this kind is not rare, and is not due to violation or contagion. Vulvitis in little girls may be also due to gonorrhea, independently of violation. This is the cause of epidemics of vulvitis and vaginitis in girls crowded in houses, hospitals, or asylums. The disease is spread by contamination from towels or bed-clothing.
The essential points of treatment to observe in the acute stage of vulvitis are rest in the recumbent posture and perfect cleanliness. The labia should be separated and the parts frequently bathed and cleaned with warm water. Various local washes or applications are of use. A warm solution of boracic acid (ʒj to a pint of water), the dilute solution of the subacetate of lead, or a solution of bichloride of mercury (1:5000) may be used.
If the disease is of gonorrheal origin, the parts should be painted once or twice a day with a 2 per cent. solution of nitrate of silver, applied after the discharges have been gently washed away.
As the disease subsides the inflammation may be found to persist in the crypts of the vestibule, the urinary meatus, and the ducts of Bartholin’s glands. It is very important that all remains of the inflammation, especially if it be of septic or gonorrheal origin, should be eradicated before the woman is discharged from treatment. The presence of any focus of inflammation, even though latent, is a constant source of danger to the woman; for septic organisms or material may be carried from the external 38 genitals to the higher parts of the genital tract, as the uterus and Fallopian tubes, with the most disastrous results.
Sometimes a small drop of pus will be observed escaping from one of the small glands or crypts of the vestibule, about the urinary meatus, after the inflammation has disappeared in other parts of the vulva. In this case the gland should be punctured with a fine cautery-point or a fine wooden probe or point saturated with pure carbolic acid or other caustic.
If the disease persists in the external meatus or urethra, it must be treated by the local applications appropriate for urethritis.
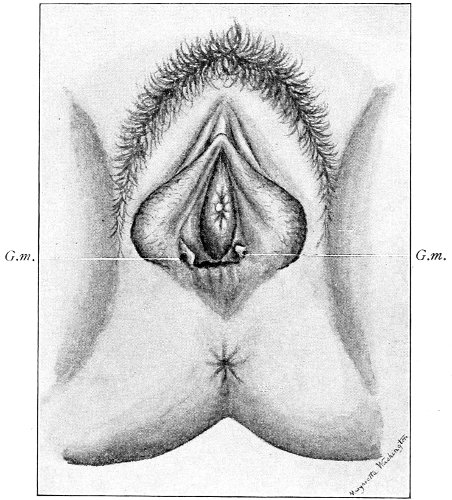
Fig. 16.—Appearance of the external genitals in a woman with gonorrhea: G. m., gonorrheal macula situated at the base of a vaginal caruncle.
Inflammation of the Vulvo-vaginal Glands.—The vulvo-vaginal glands are two in number. They are about the size of a bean, and are situated deeply on the inner aspect of the labia majora, where they may be felt in thin women. The duct of the gland is about one 39 inch in length, and opens immediately in front of the hymen, about the middle of the side of the ostium vaginæ. In cases of vulvitis the duct of the gland usually becomes inflamed, and the inflammation may extend to the gland, producing abscess of the vulvo-vaginal gland.
Inflammation of the duct and the gland may also occur independently of vulvitis, from direct septic or gonorrheal infection.
Suppuration of the duct may be demonstrated by pressing over the course of the duct, when a drop of pus will escape from the opening. In such cases the orifice of the duct is usually surrounded by a red areola, resembling a flea-bite, which has been called the gonorrheal macula (Fig. 16). This macula persists long after all other traces of inflammation about the vulva and vagina have disappeared, and after all frank suppuration in the duct has subsided. Its presence indicates at least the probability of previous gonorrheal infection.
When the duct of the gland alone is the seat of inflammation, it should be laid open with fine scissors or knife, and the tract thoroughly cauterized with the nitrate-of-silver stick, pure carbolic acid, or a solution of chloride of zinc (2 per cent.).
Suppuration of the vulvo-vaginal gland is accompanied by marked swelling and peripheral edema. The swelling may extend to the anus, and is of characteristic shape (Fig. 17). The pain is always severe. Fluctuation is first apparent on the inner surface of the labium majus. If the condition is not treated, one or more fistulous openings appear below the orifice of the duct, and the pus is discharged. The condition then becomes chronic. The fistulous openings persist. Acute inflammation disappears from the gland, leaving it in a condition of hypertrophic induration. A thin, milky or greenish, purulent fluid may be pressed out of the duct or the fistulous openings. Infection from this discharge may be communicated to man, or may ascend the genital 40 tract, producing inflammation of the endometrium or of the Fallopian tubes.
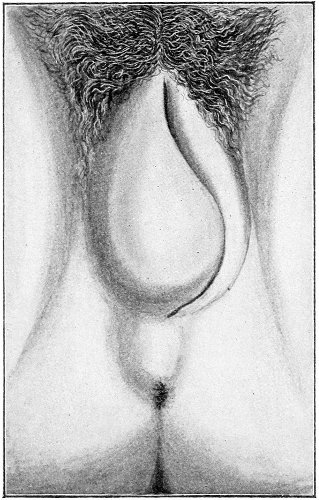
Fig. 17.—Abscess of right vulvo-vaginal gland.
In abscess of the vulvo-vaginal gland a free incision should immediately be made into the labium at the junction of the skin and the mucous membrane. The interior should be wiped out with pure carbolic acid and the cavity packed with gauze. If the disease is first seen in the chronic stage, after the abscess has evacuated itself, the only method of cure is to excise, with curved scissors, the whole of the indurated gland, the duct, and the fistulous tracts. The wound may be left open and packed, or it may be closed immediately with buried catgut sutures.
Cysts of the Vulvo-vaginal Glands.—Cysts may 41 occur in the duct of the vulvo-vaginal gland or in the gland itself. Cysts of the duct are small—about the size of a chestnut. They are situated superficially, lying immediately under the mucous membrane of the vagina at the base of the labium minus.
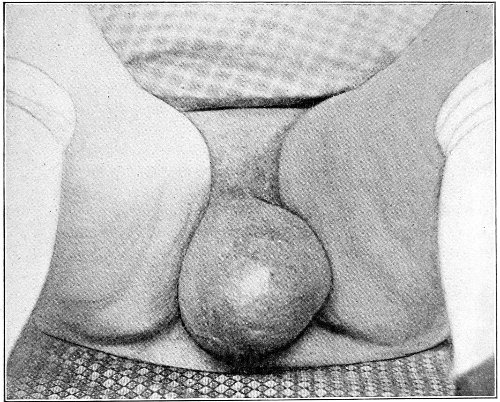
Fig. 18.—Cyst of the right vulvo-vaginal gland (Hirst).
Cysts of the gland may be unilocular if formed at the expense of a single lobule of the gland, or multilocular if several lobules enter into their formation. These cysts may attain the size of the fetal head (Fig. 18).
Cysts of the gland or of the duct are formed by retention of the cyst-contents. The retention is due to occlusion of the duct, usually the result of inflammation. In some cases the duct remains pervious, and the retention is due to the altered character of the secretion of the gland, which becomes too viscous to pass, except under unusual pressure, along the duct.
These cysts contain clear yellow or chocolate-colored 42 fluid. The diagnosis of cyst of the vulvo-vaginal gland is usually not difficult. If we are in doubt in regard to the fluid character of the tumor, this may be determined with the exploring-needle.
Inguinal hernia, hydrocele of the canal of Nuck, cysts of the round ligament, and sacculated cysts of old hernial sacs may be mistaken for cysts of the vulvo-vaginal glands. In such cases, however, the tumor lies more in the upper and outer part of the labium majus, and extends to, and may be connected with, the external inguinal ring.
Cysts of the vulvo-vaginal glands should be treated by free incision and packing, or by extirpation. If the sac is emptied by the aspirator or by a small incision, it will refill. The best method is to extirpate the cyst. In case there has been no inflammatory action binding the cyst to surrounding structures, extirpation without rupture is easy. If rupture occurs, the cyst-wall may be dissected off with the knife or removed with the curved scissors. The wound may be immediately closed with deep and superficial sutures.
Pruritus Vulvæ.—Pruritus vulvæ, or itching of the vulva, may be due to a great variety of causes. Eruptions of the vulva, such as eczema, cause itching. Irritation from the discharge of vaginitis, metritis, cancer of the cervix or body of the uterus, the presence in children of the thread-worm, the irritation from diabetic urine, or trophic lesions of the nerves due to diabetes, may result in pruritus. Some of the pathological conditions of the uterus, tubes, and ovaries may produce reflex irritation of the nerves of the vulva, and cause itching, in a manner similar to that in which vesical calculus causes itching of the glans penis.
The congestion of the external genitals that accompanies pregnancy may also produce pruritus.
There are some cases of pruritus vulvæ, however, in which no physical cause for the intolerable itching can be discovered, and in which minute examination of the affected portions of skin or mucous membrane demonstrates 43 no pathological change. Such cases are called idiopathic.
The itching may be so severe that the woman cannot refrain from scratching and rubbing the parts on all occasions. She becomes debarred from the society of her friends, and seeks relief in anodynes and hypnotics. The continual scratching increases the irritation of the vulva, and an eczematous eruption may result, which produces an irritating discharge that spreads the irritation to other parts of the body with which it may come in contact.
The itching of pruritus may extend into the vagina, to the skin of the abdomen, to the inner aspect of the thighs, and to the anus.
In the treatment of pruritus it is first of importance to discover, if possible, the cause of the itching. Any vaginal or uterine discharge should be investigated. Discharge from the uterus can be eliminated as a cause by placing against the external os a pledget of cotton, frequently renewed, to absorb the discharge before it reaches the vulva, or the parts may be kept clean by frequent douches. In children the stools should be examined for the thread-worm. The urine should always be examined. Diabetes is a frequent cause of pruritus vulvæ in old women. Any pathological condition of the uterus, Fallopian tubes, and ovaries should be treated before we can eliminate this as a possible cause of pruritus.
In the cases of so-called idiopathic pruritus in which no local lesion can be discovered attention should be directed to the general nutrition of the patient. As in pruritus ani, the gouty diathesis may cause the disease. Alcoholic drinks, rich food, fish and shell-fish, may assist in its production.
Treatment.—A great variety of local applications have been used for the relief of pruritus. In case of diabetes the urine should, as much as possible, be kept from contact with the parts, which should be thoroughly dried after urinating, and dusted with a powder consisting 44 of equal parts of subnitrate of bismuth and prepared chalk.
The following local applications are useful in pruritus:
| Bichloride of mercury, | gr. ½; | ||
| Emulsion of bitter almonds, | ℥j, | ||
| applied twice a day. | |||
A powder of 1 grain of morphine to 2 grains of prepared chalk, applied twice a day.
| ℞. | Tinct. opii, | ||
| Tinct. iodi, | |||
| Tinct. aconit., | āā. | ʒv; | |
| Acid, carbolic., | ʒj, | ||
| applied once or twice in the twenty-four hours. | |||
An ethereal solution of iodoform sprayed into the folds of the vulva with an atomizer.
Cauterization with pure carbolic acid.
In pruritus of gouty origin an ointment, composed of 15 grains of calomel to 1 dram of cerate, will often relieve or cure the local condition. A small quantity should be rubbed over the itching area at bed-time. Often one or two applications give immediate relief. If the condition does not quickly improve it is useless to continue this treatment. The danger of salivation from its prolonged use should be remembered.
In cases which have resisted all local applications the affected areas of mucous membrane have been excised. Even this method, however, does not promise certain cure. It should be tried, however, when the pruritus is localized and has resisted the milder forms of treatment.
Kraurosis Vulvæ.—Kraurosis vulvæ is a very rare disease, of chronic inflammatory nature, affecting the vulva. The disease is characterized by cutaneous atrophy, with very marked shrinking and contraction of 45 the vaginal orifice. The lesions may be unilateral or circumscribed, but usually the tissues of the labia majora, the nymphæ, and the area surrounding the clitoris and urinary meatus are more or less involved. The cause of the disease has not as yet been determined. It has been observed at every age after puberty, in the nulliparæ as well as the multiparæ, and in the parturient woman. It must be differentiated from pruritus and the atrophic changes which take place after the physiological and induced menopause.
The first symptoms noticed by the patient are usually those of pruritus—an intense itching and burning about the vulva. In some cases the affected tissue early becomes excessively hyperplastic. The mucous membrane and the skin of the vulva are often discolored, small red spots appearing, which are sensitive to touch. Later a peculiar shrinking of the superficial tissue takes place, and the diseased surfaces become dry and whitened. The nymphæ gradually disappear, fusing with the labia majora; and the mucous membrane and skin become shiny and drawn smoothly over the shrunken clitoris. Cracks or fissures appear on the dry surfaces. A sensation of drawing and shrinking of the vulva is now usually experienced. The vaginal orifice gradually narrows and contracts, until frequently the little finger can scarcely be introduced. When this last condition of atrophy is reached, the pathological process is arrested, the subjective sensations of shrinking pass away, and the symptoms resembling pruritus are no longer experienced. The shrunken and contracted vaginal orifice, however, persists and is never spontaneously restored.
Treatment.—Palliative treatment by local applications may be tried, or a cure may be attempted by operation. The palliative treatment is simply directed toward the relief of the subjective symptoms, which at times are exceedingly painful. Pure carbolic acid or a solution of cocaine applied locally, or pure nitrate of silver applications frequently repeated, afford temporary relief. Cloths 46 wrung out of hot water and placed over the vulva also lessen the suffering. A solution of the neutral acetate of lead in glycerin, on cotton placed between the labia, is recommended. Forced dilatation of the vaginal orifice under ether has been practised with good result. The most satisfactory treatment is complete excision of the diseased tissue. Unless all affected tissue is removed, the disease may return.
Varicose Tumors of the Vulva.—Varicose tumors of the vulva are usually the result of pregnancy. They may, however, accompany any form of pelvic or abdominal tumor, the pressure of which interferes with the venous circulation of the pelvis. The varicose condition usually affects the labia majora. It varies from a mere increase in size of the veins of the vulva to a varicose tumor the size of the fetal head. The condition, being secondary, usually disappears with the removal of the exciting cause. The labia may be supported with a compress and a bandage.
Hematoma of the Vulva.—Hematoma of the vulva is due to the subcutaneous rupture of a vein. Blows, kicks, or falls cause this condition. It is usually produced by rupture of a varicose vein during pregnancy or labor.
The affected labium is purple in color and may reach the size of a fetal head. When the hematoma is small the vagina should be kept as clean and aseptic as possible, and a light compress should be applied. Absorption usually takes place. If the collection of blood is large or if it has become infected, a free incision should be made into the labium, the clots should be turned out, and the cavity thoroughly washed and packed with gauze.
Papilloma.—Papillomata or warts of the vulva are not uncommon. They may occur singly, scattered over the vulva and the neighboring skin, and extending up the vagina as far as the cervix uteri, or they may occur in large cauliflower-like masses. They are pink or purplish in color. They often exude a bloody, offensive discharge, 47 which is capable of exciting a similar condition by contact. Papilloma is usually the result of gonorrhea or syphilis. It may, however, be caused by irritation from filth or by the leucorrhea of pregnancy.
The treatment of papilloma is by excision. The small warts should be picked up with forceps and clipped off with curved scissors. Every one should be removed or the condition may recur. In the case of large papillomatous tumors the wound of excision should be closed with continuous sutures. Pregnancy is no contraindication to excision of papillomata.
The vulva may be the seat of epithelioma, lupus, sarcoma, fibroma, fibromyoma, myxoma, lipoma, or enchondroma. These tumors present the same characteristics and demand the same surgical treatment as in other parts of the body.
Small cysts have been found in the labia majora and minora, the vestibule, the hymen, and the clitoris.
Elephantiasis.—True elephantiasis of the vulva (elephantiasis Arabum), due to the presence of the Filaria sanguinis hominis, is a rare disease in this climate. The disease occurs especially in Barbadoes. It may affect the labia and the clitoris. The hypertrophied labia may attain the size of the adult head.
The treatment of this condition is excision of the affected structures.
There is a syphilitic form of hypertrophy or elephantiasis of the vulva which is not uncommon in this country. The labia minora and majora may be transformed into enormous flap-like folds. Though at first free from ulceration, this may subsequently result from chafing. Warty growths may cover the hypertrophied labia, the perineum, and the buttocks. The disease usually affects both labia, though it may be confined to one.
This manifestation of syphilis does not yield readily to constitutional or local medicinal treatment. Many cases prove to be incurable by medicine. Antisyphilitic treatment 48 should always be tried at first, and if this fails, the hypertrophied structures should be excised with the knife.
If, in such cases, there is any doubt in regard to diagnosis between syphilis and cancer, a small portion of tissue should be excised and submitted to microscopic examination.
Adhesions of the Clitoris.—Adhesions between the glans of the clitoris and the prepuce or hood which covers it are exceedingly common. Usually no trouble whatever is caused by these adhesions, unless an accumulation of smegma takes place, or irritation is produced by the presence of a concretion.
In case of any irritation about the genitals, the prepuce and clitoris should always be carefully examined. In fact, a careful examination of the clitoris should form a routine part of all examinations of the external genitals.
When trouble arises from the presence of adhesions, the prepuce should be drawn back and the adhesions freed with a blunt probe. A 20 per cent. solution of cocaine should be applied to the clitoris for ten minutes previous to the operation. The whole corona and the sulcus back of the corona should be exposed. The raw surface should be covered with vaseline, and the patient should abstain from walking as long as pain is caused by it. The prepuce should be drawn back and vaseline applied every day for two weeks, to prevent the formation of adhesions. 49
Inflammation of the Vagina.—Acute inflammation of the vagina is not a very common affection. Primary inflammation confined to the vagina alone is unusual. The disease in most cases is secondary to vulvitis, urethritis, or endo-cervicitis. The causes of vulvitis (which have already been considered) are also the causes of vaginitis. It is of importance to remember that the disease may occur in children as a result of the same factors which produce vulvitis.
The exanthemata, as measles and scarlet fever, may cause vaginitis as part of the general involvement of the skin and mucous membrane which occurs in these diseases. The most usual cause is gonorrhea.
Several varieties of acute vaginitis may be recognized—the simple, the granular, the senile, and the emphysematous. It is unusual to find the entire surface of the vagina involved. The disease is confined to areas or patches separated by healthy tissue.
In simple vaginitis the inflamed membrane remains smooth.
In granular vaginitis, which is the variety usually seen, the papillæ are infiltrated with small cells, and are much enlarged, so that the inflamed surface has a granular appearance.
Senile vaginitis is due to infection of portions of the vaginal mucous membrane that have lost their epithelium as a result of the atrophic changes of old age. This disease occurs in patches of various size, sometimes presenting the character of ecchymosis; in other cases the 50 patches have altogether lost the epithelium, and permanent adhesions may take place between areas which are brought in contact. This form of vaginitis has also been called adhesive vaginitis. It is said that a similar condition may occur in children.
The emphysematous form of vaginitis occurs in pregnancy. The vaginal walls are swollen and crepitating. The gas is contained in the meshes of the connective tissue.
Acute vaginitis is accompanied by dull pain and a sense of fulness in the pelvis. The discomfort is increased by standing, walking, defecation, and urination. There is a free discharge of serum or pus, which may be tinged with blood. The character of the discharge depends upon the variety and the period of the disease. Inspection, which can best be made through the Sims speculum, with the woman in the Sims or knee-chest position, shows the characteristic lesions of inflammation of the mucous membrane.
Acute vaginitis, if neglected, may pass into the chronic form. It usually lingers in the upper part of the vagina, in the fornices, especially in vaginitis of gonorrheal origin. By careful inspection we find here one or more granular patches of inflammation, which cause a vaginal discharge from which man may be infected, and from which infection of the upper portion of the genital tract, the uterus, and the Fallopian tubes may be derived.
Treatment.—Vaginitis, especially of the gonorrheal form, should be treated vigorously, and treatment should be continued until all traces of inflammation have disappeared. Inflammation of any part of the lower portion of the genital tract may have the most disastrous consequences if it extends to the uterus and the Fallopian tubes.
The woman should be kept as quiet as possible. The bowels should be moved freely with saline purgatives. She should take, three times in twenty-four hours, lying upon her back, a vaginal douche of one gallon of a boracic-acid 51 solution (ʒj to the pint). The temperature of the solution should be about 110° F.
If the disease be of gonorrheal origin, a warm bichloride solution (1:5000) should be used in the same way.
After the acute symptoms have subsided local applications should be made, in addition to the douches. The woman should be placed in the knee-chest position, and the vagina should be thoroughly exposed with the Sims speculum. If necessary, the vaginal surface should be gently cleaned with warm water and cotton. A 4 per cent. solution of cocaine may be applied to the vagina if there is much pain. Then the entire vaginal surface should be painted with a solution of bichloride of mercury (1:1000). These applications should be made daily until the disease is cured. The vaginal douches should be continued at the same time.
In the chronic form of the disease and in senile vaginitis the local patches of inflammation should be painted once a day with a solution of nitrate of silver, 5 to 10 per cent., or stronger if the condition does not yield. The senile form of vaginitis, being dependent upon a general condition, is often impossible to cure. We can sometimes relieve the discomfort by applying boracic-acid ointment (ʒj to ℥j) to the vagina. The application of pure carbolic acid to the inflamed patches sometimes does good.
Urethritis usually accompanies a gonorrheal vaginitis, and demands coincident treatment.
Tumors of the Vagina.—Vaginal Cysts.—Well-defined cysts are sometimes found in the vaginal walls. They occur at all ages from childhood to old age.
Vaginal cysts are usually single. They vary in size from that of a pea to that of a fetal head. The vaginal mucous membrane covers the free surface of the cyst, and may either be movable over it or may be much attenuated and closely incorporated with the cyst-wall. Vaginal cysts may be sessile or more or less pedunculated. The internal surface of the cyst is usually covered with 52 cylindrical epithelium, which is sometimes ciliated. The contents vary in consistency and color. They are often viscid, transparent, and of a pale yellow tint. They may contain pus or altered blood.
The origin of vaginal cysts has been much disputed. It is probable that they arise from the remains of the Wolffian canal—the canal of Gärtner. In the embryo the transverse or longitudinal tubule of the parovarium extends to the side of the uterus and thence down the side of the vagina to the urethral orifice. It persists in this condition in some of the lower animals—the sow and the cow—and may also persist as a closed tube in woman. In such cases it may become distended and form the vaginal cyst.
The treatment of vaginal cyst is removal. If the tumor be situated near the vulva, it may be extirpated by careful dissection. If this operation be deemed impracticable, partial excision of the cyst should be practised. The tumor should be seized with a tenaculum, opened by the scissors, and part of the wall, with the overlying mucous membrane, should be excised. The interior of the cyst should then be packed with gauze.
Fibroid Tumors of the Vagina.—Fibroid tumors sometimes occur in the vagina. They are usually found in the upper part of the anterior wall. They are sometimes adherent to the urethra. They are usually of small size, but may attain a diameter of six inches. The treatment of such tumors is removal.
Cancer and sarcoma may attack the vagina, though these diseases as primary conditions are very rare. When possible, complete removal should be done.
Atresia of the Vagina.—Severe puerperal infection or mechanical injury, followed by extensive destruction of the tissues of the vagina, may result in a cicatricial narrowing or complete closure or atresia of the vaginal canal.
The symptoms of this condition are due to retention of the uterine discharges. There is no discharge of 53 menstrual blood from the vagina. Attacks of pain occur periodically at the menstrual periods. A cystic tumor, which may be felt by rectal examination, is present. The tumor consists of the distended portion of the vaginal canal (hematocolpos), and sometimes of the distended cervical canal and body of the uterus. The contents of the hematocolpos are usually sterile, although they may become purulent (pyocolpos).
The diagnosis is readily made by vaginal and rectal examination.
Treatment consists in incision and excision of the vaginal septum and the suture of the vaginal mucous membrane above to that below the obstruction. In very severe cases it is difficult to maintain the patulous condition of the vaginal canal on account of subsequent cicatricial contraction. In such cases the repeated passage of vaginal bougies or the transplantation of mucous membrane has been resorted to.
Vaginismus.—The term “vaginismus” has been applied to a condition characterized by a spasmodic contraction of the muscles which close the vaginal orifice. The muscular spasm occurs reflexly when penetration of the vagina is attempted, as at coitus or a digital examination. The condition is due to dread of pain, and is usually the result of some painful local lesion, such as a urethral caruncle, fissures or sores of the vulva or anus, etc.; or it may be due to some painful condition of the tubes and ovaries. Similar contraction is observed in the sphincters of the anus when there is present a painful anal lesion.
Vaginismus has been said to occur in neurotic and hysteric women in whom there was no discoverable local lesion.
Treatment consists in the removal of any local cause of pain or irritation.
If the reflex spasm of the muscles persists when coitus is attempted, notwithstanding the removal or the absence 54 of any discoverable local cause, operative measures have been advised.
Under anesthesia the vaginal entrance has been stretched by means of large dilators or the fingers, or the fibers of the sphincter vaginæ have been cut on each side of the fourchette and a glass or vulcanite tube of suitable size has then been placed in the vagina and retained for two or three weeks by a perineal pad and T-bandage.
Vaginismus is a very rare condition. Operative treatment, except that which may be required for the removal of some local cause of irritation, is rarely, if ever, necessary.
Coccygodynia.—Coccygodynia is a rare affection characterized by pain in the coccyx and surrounding structures. The pain is caused by pressure, as in sitting, or by any movement involving the muscles attached to the coccyx. The disease is usually caused by traumatism, and in most cases is due to injuries to the coccyx in labor, as a result of which the bone is fractured or dislocated, and becomes fixed in an abnormal position. Sometimes osteitis or necrosis develops. In the unusual cases, in which no structural changes are detected, the condition may be due to rheumatism. Coccygodynia is very rarely found in men.
The diagnosis may be made by introducing the index finger in the rectum and palpating the anterior and lateral surfaces of the coccyx, and by moving the bone between the finger in the rectum and the thumb placed in the crease of the nates. The mobility, deformity, and tenderness may be readily determined. If a local lesion is found, and the symptoms have not yielded within a reasonable time to expectant treatment, removal of the coccyx by operation is indicated. The coccyx is exposed by a median incision, the bone is separated from its muscular and tendinous attachments, and is removed at the sacrococcygeal articulation with scalpel or scissors. If 55 the articulation is ankylosed, it may be necessary to use the chain-saw. The wound is drained with a few strands of silkworm-gut and closed with interrupted sutures.
Operation should not be advised hastily. The painful symptoms are not always relieved by it. Operation should not be performed unless bony deformity or other distinct lesion is found. 56
An accurate knowledge of the anatomy and mechanism of the female perineum is essential to an understanding of the nature and treatment of injuries to this structure. The anatomical structures lying between the anus behind and the symphysis pubis in front are those that most directly interest the gynecologist. Proceeding from 57 below upward, we find the following structures lying in superimposed planes: the skin, the superficial fascia, the deep layer of the superficial fascia, the transversus perinæi and the sphincter vaginæ muscles, the anterior layer of the triangular ligament, the posterior layer of the triangular ligament, the levator ani muscle (Fig. 19).
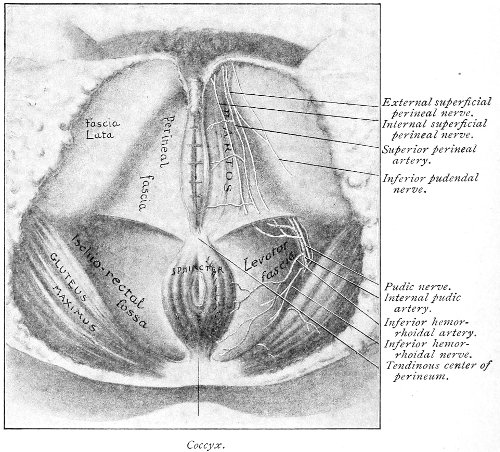
Fig. 18, A.—Superficial structures of the female perineum (Weisse).
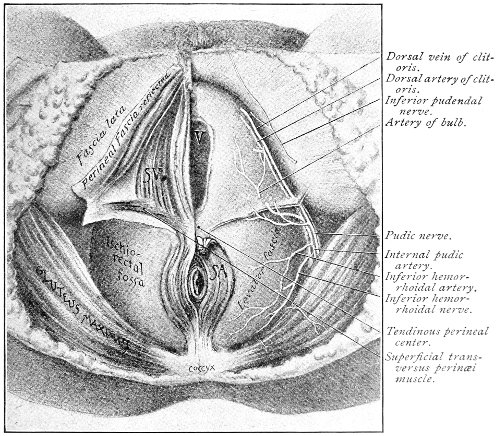
Fig. 19.—Dissection of female perineum: on the left side the perineal muscles are exposed by the reflection of the perineal fascia; on the right side the muscles and the superficial layer of the triangular ligament have been removed, thereby exposing the deep layer of the ligament. S. V., Sphincter vaginæ muscle.
The vagina passes through these structures. They surround and support the ostium vaginæ as the fascia and muscles surround and support the opening of the rectum or the anus. The muscles and fasciæ are attached in the median line between the anus and the vagina, and therefore this part of the body, which is called the perineum, is supported or maintained in its 58 proper position by these various structures. The transversus perinæi arises from the ramus of the ischium and is inserted in the perineum. The bulbo-cavernosus, or sphincter vaginæ, arises in the perineum and is inserted in and about the clitoris. The inner fibers of the levator ani arise from the symphysis pubis and are inserted in the perineum and the lower part of the vagina (Fig. 20). When these muscles contract, their action, therefore, is to draw the perineum upward and forward. At the same time the anus is drawn upward and forward, and so also is the posterior margin of the ostium vaginæ and the lower portion of the posterior vaginal wall.
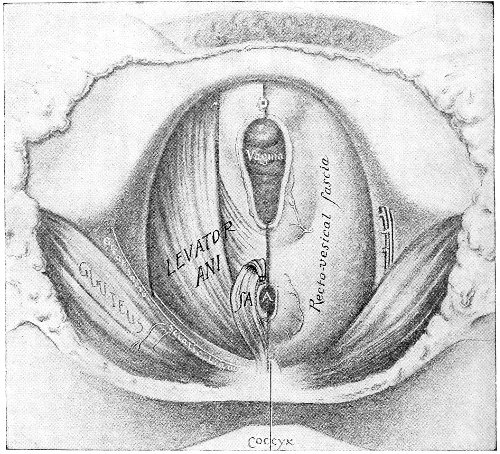
Fig. 20.—Dissection of female perineum, showing the deeper structures after removal of the levator and sphincter ani muscles.
The vagina has no circular sphincter like the anus, but 59 the vaginal month is kept closed by the action of the transversus perinæi, sphincter vaginæ, and levator ani muscles, which draw the perineum forward, and thus keep the posterior vaginal wall in apposition with the anterior wall.
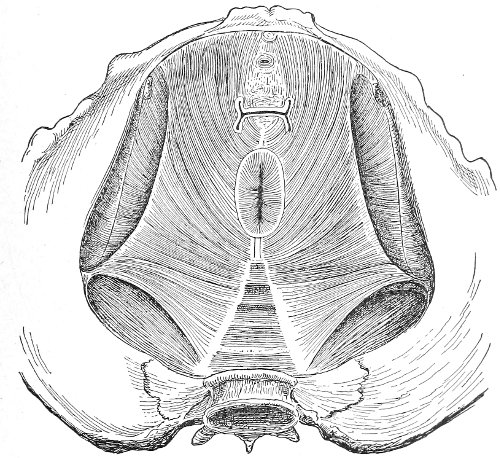
Fig. 21.—Muscular floor of the pelvis seen from above.
This sling of muscles and fascia, which surrounds and supports the opening of the vagina, may readily be felt in the nulliparous woman by introducing the finger in the vagina and pressing backward and outward toward the ischio-rectal fossa. We then feel plainly, immediately within the ostium vaginæ, a firm resisting band of tissue, apparently about half an inch broad, embracing the posterior portion of the lower vagina. This band is formed by the inner edges of the various muscles and planes of fascia that have been described.
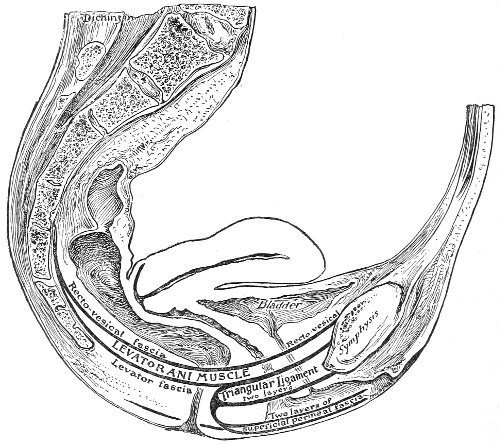
Fig. 22.—Sagittal section showing relations of the several layers of fascia within the pelvic floor (Dickinson).
The vagina extends, as a transverse slit in the pelvic floor, upward and backward, approximately in the direction 60 of a line drawn from the ostium vaginæ to the fifth sacral vertebra. It is approximately parallel with the conjugate of the brim, so that when the woman is erect the long axis of the vagina is inclined at an angle of 60° to the horizon. The vagina is not a vertical open tube: it is a slit in the pelvic floor, in health always closed by the accurate apposition of the anterior and posterior walls (Fig. 21). The anterior vaginal wall is about 2½ inches long in a vertical mesial line. The posterior vaginal wall is about 3½ inches long. The vaginal walls are triangular in shape, being broader above than below. The shape of the normal vagina at the pelvic outlet is shown by Fig. 23. The section here shows the vaginal 61 slit of the shape of the letter H. The portions of the slit extending backward and somewhat outward are called the vaginal sulci or furrows. They are directions of diminished resistance in which tears are liable to occur.
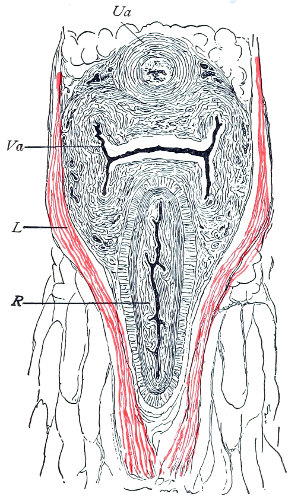
Fig. 23.—Section illustrating the characteristic form of the vaginal cleft (Henle): Ua, urethra; Va, vagina; L, levator ani; R, rectum.] 62
The injuries to the perineum that may result from childbirth are classified according to the position or the direction and extent of the laceration. They are as follows: slight median tear; median tear involving the sphincter ani; tear in one or both of the vaginal sulci; subcutaneous laceration of the muscles and fascia.
All these injuries demand operative treatment. The operation for the repair of injuries to the perineum is called perineorrhaphy. It is called immediate or primary, intermediate, and secondary perineorrhaphy, according to the time after the receipt of the injury at which the operation is performed. The primary operation is done during the first twenty-four hours. The primary operation should always be performed. A careful inspection of the perineum and the posterior vaginal wall should always be made after labor, and any laceration should be repaired within twenty-four hours. The advantages of the primary operation are many. The parts are usually so numb that it is not necessary to administer an anesthetic. No denudation is necessary, and therefore no tissue need be sacrificed. The woman is spared the pain and discomfort of granulation and cicatrization.
The bad results that follow neglect of the primary operation are very numerous, and will be studied hereafter. The injured muscles retract, and, being functionally useless, undergo atrophy, and when finally repaired never possess their former strength. Involution in the vagina and the uterus may be arrested, and all the disasters incident to subinvolution may appear. Vaginal and uterine prolapse occur; the natural supports of the 63 vagina and uterus become stretched, and, though afterward the perineum may be restored, yet it may be found impossible to retain the uterus in its proper position. It is always good surgery to repair an injury as soon as possible.
When practicable, a certain amount of preparation of the patient should be made before the operation of perineorrhaphy. This is most easily effected before the intermediate and secondary operations. The vagina and the vulva should be sterilized, and the intestinal tract should be emptied. Thorough evacuation of the bowels is most important when the sphincter ani has been injured, because it is desirable, after operation for this lesion, that the bowels should not be moved for five or six days. A saline purgative should be administered on an empty stomach about five hours before the operation, and a rectal injection of soap and water should be administered about one hour before the operation. Whatever purgative be employed, it should be administered at such a time that its action shall have ceased by the time of the operation. If this precaution is not observed, there may be a discharge of feces that will infect the wound and interfere with the manipulations.
For operation upon the perineum the woman should be placed in the dorso-sacral position (Fig. 1, page 23).
The intermediate operation is performed during the granulation period—ten days or two weeks after labor. At this time the raw surfaces are covered with granulation-tissue and bathed with pus. The edges of the wound and the surrounding tissue may be hard and swollen from infiltration with inflammatory products. In the intermediate operation it is necessary to administer an anesthetic or to anesthetize the parts locally with a 10 per cent. solution of cocaine.
All cicatricial tissue, granulation-tissue, and rough edges should be scraped away with the knife, the scissors, or the curet. The raw surfaces should be thoroughly 64 washed with a 50 per cent. solution of peroxide of hydrogen and a 1:1000 solution of bichloride of mercury. The sutures should then be introduced.
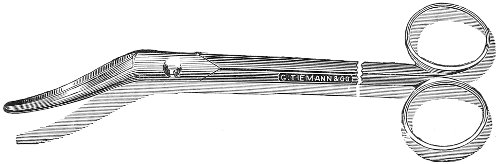
Fig. 24.—Emmet’s perineal scissors.

Fig. 25.—Curved scissors for denuding.

Fig. 26.—Tenacula for plastic operations.
The secondary operation is performed at any time after cicatrization has occurred—often many years after the receipt of the injury. This operation is at present one of the commonest in gynecology, because the injury is not detected, is neglected, or is improperly repaired after labor. In the secondary operation an anesthetic is necessary. The mucous membrane must be removed or denuded on the posterior wall and about the mouth of the vagina, in order that the lacerated structures may be brought again in apposition. The denudation is best made by means of scissors curved on the flat (Figs. 24 and 25).
The strip of mucous membrane to be removed is picked up with a tenaculum (Fig. 26) or with tissue forceps 65 (Fig. 27); the scissors are placed with the blades parallel to the surface to be denuded, and the strip is cut away evenly, in one piece if possible. A similar contiguous strip is removed, and so on until the necessary surface is bare. Sponges in holders (Fig. 28) or continuous irrigation may be used to remove blood.

Fig. 27.—Tissue-forceps.

Fig. 28.—Sponge-holder.
For all operations on the perineum round-pointed needles curved at the tip should be used (Fig. 29). The tissues are always sufficiently soft for the passage of such a needle. A needle with a cutting edge is unnecessary and may increase the bleeding.
The needle may be held in any kind of needle-holder preferred. The Emmet needle-holder (Fig. 30) is very convenient.
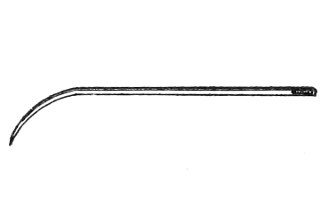
Fig. 29.—Emmet’s perineal needle.
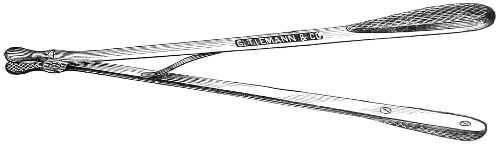
Fig. 30.—Emmet’s needle-holder.
The point of the needle should be guided and held by the tenaculum. The tenaculum must always be held in a plane parallel with the plane of the needle-holder; otherwise the needle-point may escape from the embrace of the tenaculum. 66
Silver wire and silkworm gut are the best sutures in the operation of perineorrhaphy.
The suture is conveniently attached to the needle by means of a silk carrier (Fig. 31).
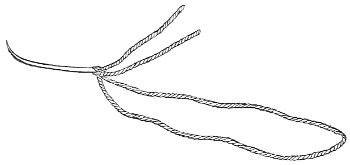
Fig. 31.—Perineal needle with silk carrier.
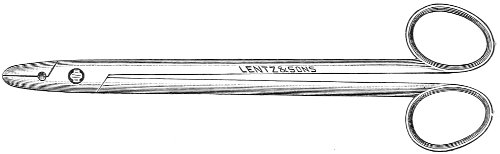
Fig. 32.—Shot-compressor.
The sutures may be fastened by passing the ends through a perforated shot which is slipped down to the line of union and compressed by the shot-compressor (Fig. 32). All blood should be carefully removed from the surfaces that are brought together. The sutures should only be sufficiently tense to produce accurate apposition. A light gauze drain should be introduced in the vagina, and should be removed in forty-eight hours. Afterward one vaginal douche of about a quart of warm bichloride solution (1:2000) should be administered every day. After the douche the labia should be separated and the vagina carefully dried by cotton held in dressing-forceps. Except in those cases in which the sphincter ani is involved, the bowels may be moved on the second or third day. The woman should stay in bed for two weeks, at the end of which time the sutures should be removed. 67 She should avoid heavy lifting, long standing, and bicycle- or horseback-riding for two months after the operation. Constipation should always be avoided. Coitus may be resumed six weeks after operation.
The special forms of operation will be discussed in the consideration of the varieties of perineal injury.
Slight Median laceration of the Perineum.—In this injury the tear takes place through the fourchette. Posteriorly it may extend as far as the sphincter ani muscle. Upward it may extend for an inch up the posterior vaginal wall. The appearance of this tear is shown in Fig. 33. It will be noted that, as this tear takes place in the median line, none of the muscles that support the perineum are involved, nor are the planes of fascia injured. The perineum is slightly split, and the insertions and origins of the muscles and the fascia are slightly separated. The supporting structures of the perineum and the pelvic floor are, however, uninjured.
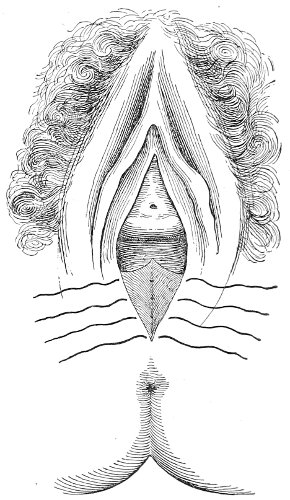
Fig. 33.—Recent slight median laceration of the perineum: sutures introduced.
If this tear is detected after labor, it should be closed by the immediate operation. A slight tear involving chiefly the cutaneous aspect of the perineum should be closed by three or four sutures introduced from the outside, as in Fig. 33. The needle should be introduced about a quarter of an inch from the edge of the wound. It should not be passed parallel with the plane of the lacerated surface, but should be swept outward and then inward toward the 68 angle at the bottom of the tear (Fig. 34). It may either emerge at the angle and be re-introduced, or it may be passed directly through to the skin-margin on the opposite side of the wound. If the suture is passed in this way, there will be perfect apposition throughout the whole surface of laceration. If the sutures are improperly passed, there may result only apposition of the skin-edges.
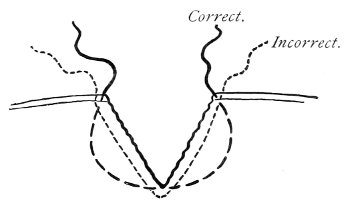
Fig. 34.—Diagram representing the correct and the incorrect method of passing the suture for closure of slight perineal laceration.
If the laceration extends up the posterior vaginal wall, two sets of sutures must be introduced—one on the vaginal aspect of the tear, and one on the skin aspect (Fig. 35).
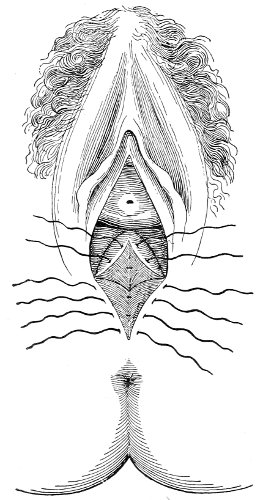
Fig. 35.—Recent slight median laceration of the perineum extending up the posterior vaginal wall: sutures introduced on the vaginal and cutaneous aspects.
The secondary operation of perineorrhaphy is not indicated in slight median lacerations of the perineum that may have been neglected at the time of labor, as the integrity of the pelvic floor is practically unaffected by them.
Median Tear involving the Sphincter Ani.—In this 69 form of injury the laceration takes place in the median line and extends backward through the sphincter ani muscle, and perhaps upward for one or more inches through the recto-vaginal septum. Permanent incontinence of feces results.
Though this is a most extensive injury attended by most unpleasant results, yet it will be seen that none of the supporting structures (the fascia and the muscles) that support the pelvic floor are injured by it.
The perineum is split in the middle, but the muscles attached to it, being uninjured, are still able to draw the two halves of the perineum forward, thus supporting the posterior vaginal wall and keeping the vagina closed. There is but very little tendency to separation of the two parts of the split perineum by lateral traction, the only muscle that acts at all in this direction being the feeble transverse perineal muscle.
Therefore, though there is loss of power of the sphincter ani muscle, yet in this injury the woman may not suffer any of the consequences of loss of power in the support of the pelvic floor, such as vaginal and uterine prolapse.
After laceration of the perineum through the sphincter ani the divided muscle retracts so that it embraces only the posterior margin of the anus. If the injury be not repaired immediately, retraction and atrophy progress, so that in time the sphincter muscle, lying posterior to the anal opening, may be but half an inch in length and of very much less than its normal thickness. Cicatrization takes place, and the parts present the appearance shown in Fig. 37.
Notwithstanding the atrophy and retraction of the muscle, continence may be re-established by operation, though many years may have elapsed since the receipt of the injury.
Notwithstanding the very obvious reasons for the performance of the immediate operation for the relief of this condition, it is yet very often neglected, and the 70 gynecologist is called upon to repair the injury many years after its occurrence.
The important part of the operation for this injury consists in the repair of the muscle. In many operations the recto-vaginal septum is repaired and the cutaneous portion of the perineum is repaired, but the operator fails to secure in his sutures the sphincter ani muscle, and consequently the incontinence is not cured (see Fig. 36). The mistake often made is that the sutures that are introduced to close the anterior margin of the anus are inserted too far forward and too far out to catch the ends of the sphincter ani muscle, which has retracted so that, in some cases, it lies altogether behind the anal opening. Or, perhaps, only the outer fibers of the sphincter ani are included in the suture, and partial incontinence results.
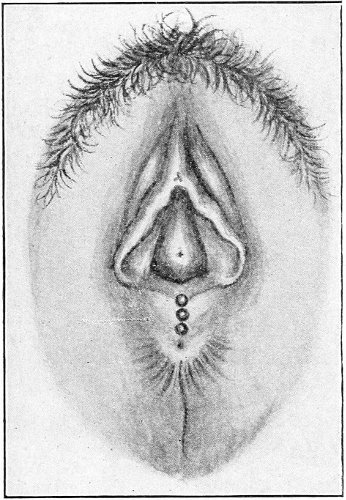
Fig. 36.—Imperfect repair of the sphincter ani. The muscle has not been included by the sutures, and does not surround the anal opening.
The position of the sphincter ani muscle is indicated by the corrugated or wrinkled skin overlying it. The ends of the muscles, being retracted, do not lie in the plane of the laceration, but their position is marked by a depression or dimple (Fig. 37).
The technique of the primary operation is included in a consideration of that of the secondary operation, the only difference being that in the latter operation denudation is necessary.
The parts should first be denuded, so that they present the same raw surface that was exposed in the original laceration. 71
The lower end of the recto-vaginal septum that forms the anterior margin of the anal opening is usually thin and cicatricial where the mucous membranes of the vagina and rectum unite. All this cicatricial tissue should be cut away, and the mucous membrane of the vagina may be drawn forward and separated by dissection from the mucous membrane of the rectum, in order to make a somewhat broader surface through which to pass the sutures.
Special care should be directed to the denudation of the ends of the sphincter muscle. The tissue lying at the bottom of the depression that marks the end of the sphincter should be picked up with forceps or a tenaculum and carefully cut away. In removing tissue attached to the mucous membrane of the rectum the operator should avoid cutting the healthy portion of this mucous membrane, as bleeding from it is often annoying.
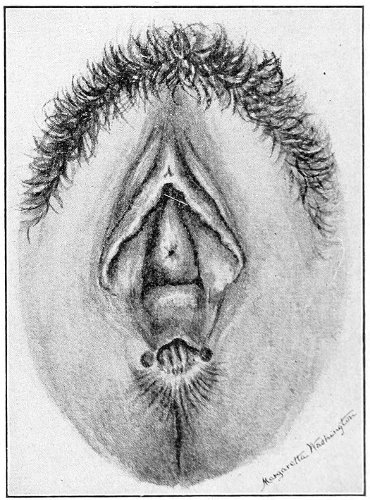
Fig. 37.—An old laceration through the sphincter ani. The sphincter muscle lies behind the anal opening. Its position is indicated by the wrinkled skin; its ends are marked by the depressions on each side of the anal opening.
The first suture should be introduced at the margin of the anal opening, within the area of corrugated skin that marks the position of the muscle, and behind the depression that marks the end of the muscle. The end of the muscle may be seized with a tenaculum or with tissue-forceps and drawn out to ensure that the suture includes muscular tissue. The needle is then passed near the edge of the rectal mucous membrane to the apex of the tear in the recto-vaginal septum. 72 whence it emerges. It is re-introduced here, and passed in a similar manner to emerge upon the opposite side, behind the other end of the sphincter ani muscle (Fig. 38). This suture is introduced very near the edge of the wound, so that there may not be any inversion of skin to prevent perfect apposition of the ends of the muscle. In case there has been much retraction of the sphincter ani muscle, the ends of the suture may appear to lie behind the anal opening. The second suture is introduced somewhat outside of the first—still, however, within the area of the sphincter muscle—and is passed in a similar manner to emerge in the apex of the recto-vaginal tear anterior to the first suture. The remaining sutures to close the perineum are passed as already described in the operation for slight median tear of the perineum. When the sutures are shotted, great 73 care must be exercised in making perfect apposition of the parts brought together by the first two sutures. Sometimes such apposition is more easily secured by shotting the anterior perineal sutures first. When the operation is completed the first suture through the sphincter is sometimes drawn upward, so that it disappears in the anal opening. If the muscle has been properly secured, it will be observed that the anal opening is surrounded by the ring of wrinkled or corrugated skin (Fig. 39).
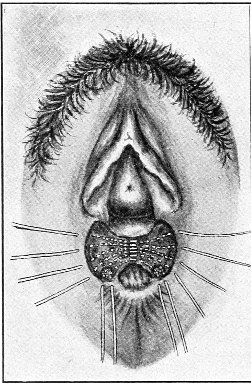 |
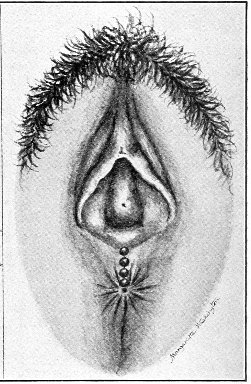 |
Fig. 38.—Denudation and sutures for repair of laceration. The two posterior sutures pass through the sphincter muscle. |
Fig. 39.—Completed operation. The anal opening is surrounded by the sphincter. One shot has disappeared in the anus. The anterior suture is omitted. |
After this operation the bowels should not be moved for five or six days. The intestinal contents should then be rendered as soft as possible by the administration of small repeated doses of some saline purgative, as Rochelle salts ʒj, every hour for five or six hours. If the woman feels that she may have difficulty in having a passage, a rectal injection of a pint of soapsuds and warm water should be very carefully administered. The nozzle of the syringe should be well greased and passed along the posterior margin of the anal opening. After this the bowels should be moved every forty-eight hours. The sutures should be removed at the end of two weeks.
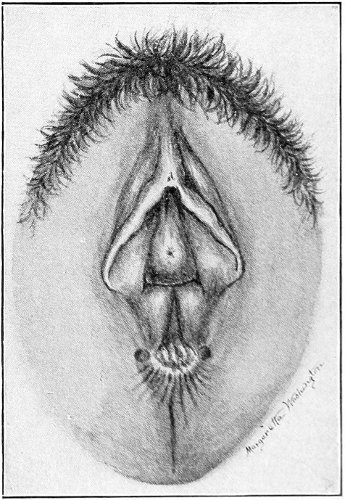
Fig. 40.—Laceration through the sphincter ani, extending up the recto-vaginal septum.
Laceration through the Sphincter Ani, involving the Recto-vaginal Septum.—In case the recto-vaginal septum has been torn, it may be necessary to repair the tear before operating on the perineum and the sphincter ani muscle. In some 74 cases the laceration extends for three or more inches up the septum (Fig. 40).
The edges of the septal tear should be denuded, the strip of tissue being cut away to the line of normal rectal mucous membrane. Annoying bleeding may occur if the mucous membrane of the rectum is injured. The denudation may be extended on the vaginal aspect as far as is necessary to obtain a sufficiently broad surface for approximation.
The tear in the septum should be closed by interrupted sutures introduced from the vaginal aspect. The suture is passed through the vaginal mucous membrane at about an eighth of an inch from the edge of the wound, and emerges in the edge of the rectal mucous membrane. It should not pass through the rectal mucous membrane.
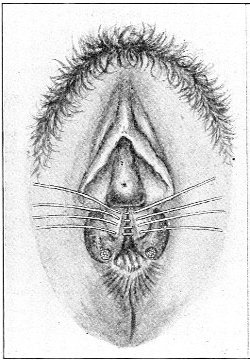 |
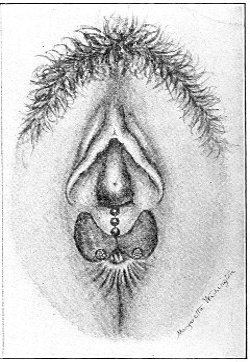 |
Fig. 41.—Denudation. Sutures introduced to close the laceration of the recto-vaginal septum. |
Fig. 42.—Laceration of the recto-vaginal septum closed. The operation is completed by the introduction of sutures as in Fig. 38. |
After the sutures in the recto-vaginal septum have been shotted, the operator may proceed to repair the perineum and the sphincter ani muscle (Figs. 41, 42). 75
There is a variety of perineal laceration (between the first slight median laceration and the second complete laceration through the sphincter ani) in which only the outer fibers of the sphincter muscle are injured. In this injury partial incontinence results. The woman may be able to control feces when the movements are hard, but loses control over liquid feces and flatus.
There is no loss of support of the pelvic floor, and the indication for operation is the partial incontinence. The operation is performed in a way similar to that already described for complete laceration. The ends of the ruptured fibers of the sphincter muscles are usually indicated by a slight depression on the overlying skin or mucous membrane.
Laceration in One or Both Vaginal Sulci.—In this form of injury the tear takes place not in the median line, but in the direction of the vaginal sulci or furrows. The left sulcus is usually the more deeply torn.
In this form of laceration the sphincter ani muscle usually escapes injury; the tear is directed toward the ischio-rectal fossa, and the rectum and anus are pushed to one side. The structures of importance that are injured are the fascia, the levator ani muscle, the sphincter muscle of the vagina, and perhaps the transverse perineal muscle. All the supporting structures of the perineum and of the posterior vaginal wall are injured. If the laceration be bilateral, complete loss of support of the perineum and the posterior vaginal wall results, and if the condition be untreated, all the disastrous consequences of loss of support of the perineum occur—prolapse of the vagina, of the uterus, and of the other pelvic organs.
It is unusual that this form of laceration is entirely limited to one sulcus, though one is usually more involved than the other. When the injury is limited to one side, the perineum is still supported by the muscles and fascia upon the other side, and the tendency to prolapse is not so marked.
The nature of this injury may always be detected by 76 examination after labor. The anterior vaginal wall should be elevated by a retractor, and the posterior wall should be carefully examined. An external tear of the skin, generally in the median line, usually accompanies laceration in the sulci; that is, the lacerations in the sulci converge toward the fourchette.
The immediate operation should always be performed. The torn sulci should be closed by sutures introduced on the posterior vaginal wall (Fig. 43), and the external tear should be closed by sutures introduced as in the first form of injury to the perineum, already described.
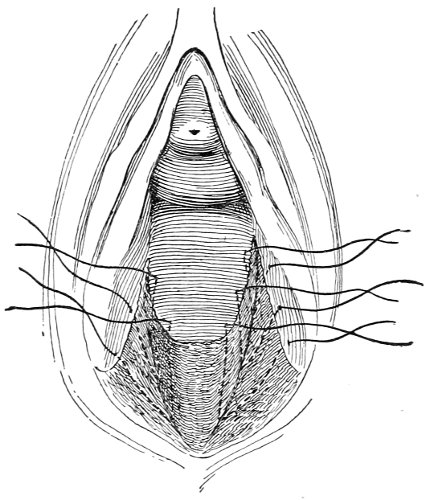
Fig. 43.—Sutures introduced for the closure of a recent perineal laceration in the sulci.
If this form of perineal injury is not repaired by the immediate operation, cicatrization takes place, and the tears in the mucous membrane and in the skin become healed. The fascia retracts, and the integrity of the supporting planes of fascia is destroyed. The torn muscles, the inner fibers of the levator ani and the sphincter vaginæ, also retract and cease to furnish any support to the perineum. In health these muscles embrace the lower portion of the posterior vaginal wall like a sling, drawing 77 it toward the symphysis pubis; after laceration in the sulci the support of one or both of the arms of the sling is destroyed.
The scars upon the mucous membrane and on the skin in time become faint, with difficulty perceptible. By elevating the anterior vaginal wall and closely inspecting the posterior wall immediately within the ostium vaginæ we may detect a fine irregular white line running in the direction of the vaginal sulcus and dividing the normal transverse ridges and furrows of the vaginal mucous membrane. This is the only sign of former injury to the vaginal mucous membrane. The injury to the underlying structures—the supporting structures of the perineum, the muscles and the fascia—is indicated by certain characteristic and unmistakable signs. These signs are best recognized after a careful study of the normal uninjured perineum.
If an uninjured woman be placed in the lithotomy position and the perineal region be carefully examined, we observe the following points:
The anus is not prominent: it is drawn upward and forward; the anal cleft is deep.
The perineum, or the surface between the anus and the fourchette, is shallow; the distance from the anus to a fixed point like the external meatus is relatively short: this surface is more or less convex, showing muscular tonicity.
If the labia are separated, it will be observed that the anterior and posterior vaginal walls are in close apposition. If the woman is made to strain or to bear down, the vaginal walls appear to come into close contact; the perineum is pushed directly downward, and becomes more prominent under the increased intra-abdominal pressure, but there is no tendency to eversion or rolling out of the vaginal walls.
If the vulva is pricked with a needle, reflex muscular action is immediately observed: the anus is drawn still more upward and forward; the perineum is shortened; 78 the ostium vaginæ is closed more firmly by the drawing forward of the posterior margin of the opening. The test shows that the muscles supporting the perineum are intact.
If the finger be introduced into the vagina and be pressed backward and outward in either vaginal sulcus, resisting structures are felt. There seems to be a band, perhaps half an inch in breadth, immediately within the ostium vaginæ, that holds forward the perineum and the posterior vaginal wall and resists the pressure of the finger.
Compare these characteristic features of the uninjured perineum with what we observe in a woman in whom there has been an untreated laceration of the perineum in the vaginal sulci. Here the supporting structures of the perineum have been destroyed.
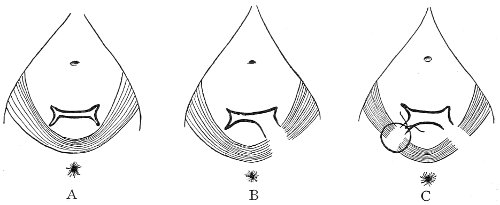
Fig. 44.—Diagram showing the sling of muscle and fascia supporting the perineum and the posterior vaginal wall. In A the parts are intact; in B there has been a laceration in the left vaginal sulcus; in C there has been a laceration in both sulci; a suture has been introduced on the right side.
The anal cleft is shallow. The anus is prominent; the surrounding structures present the appearance of relaxation. The perineum is deep; the distance from the anus to the external meatus is longer; the anus has really dropped back. The skin-surface of the perineum is flat and relaxed.
If the labia are separated, the anterior and posterior vaginal walls will not be found in close apposition. The 79 ostium vaginæ is patulous and gaps open (Fig. 45). If the woman is made to bear down, the anterior and posterior vaginal walls are not pushed together; they are rolled out and protrude through the ostium vaginæ.
If the vulva is pricked with a needle, the woman draws herself away; there is no reflex muscular action, closing the vagina and drawing up the anus. The muscles of the perineum have been destroyed.
If the finger is introduced in the vagina and pressed backward and outward in either vaginal sulcus, the tissues are yielding and soft; no supporting sling of muscle and fascia is felt.
These phenomena have an unmistakable meaning, and indicate clearly the loss of the supporting structures of the pelvic floor.
The student should acquire familiarity with these tests by repeated experiments on injured and uninjured women. It will easily be understood that the same phenomena characterize the fourth form of injury to the perineum—the subcutaneous laceration.
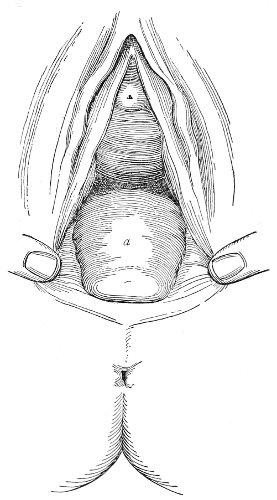
Fig. 45.—An old laceration of the perineum in both sulci. Rectocele. The mouth of the vagina is held open to show the appearance of the parts before operation: a, apex of the rectocele.
A perineum in this condition is often said to be relaxed. It is relaxed because the muscular and fascial supports have been destroyed.
Treatment.—The treatment is directed to the restoration 80 of these supports. Each vaginal sulcus must be denuded, so that the condition existing in the recent injury (Fig. 43) is reproduced, and the sutures must be passed so that the retracted muscles and the fascia are brought back to their normal attachments. The best method of operating for this condition has been devised by Emmet.
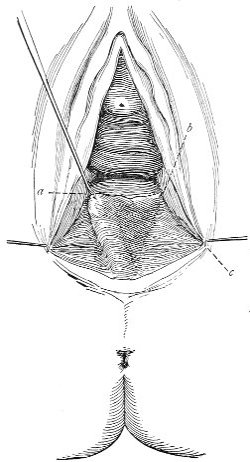 |
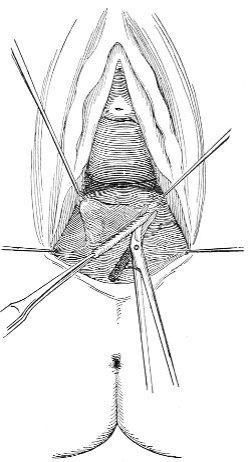 |
Fig. 46.—The rectocele is seized with the tenaculum at a, and is drawn to the right, exposing the left vaginal sulcus, a, b, c, which must be denuded. The point b should be secured with a tenaculum before denuding. |
Fig. 47.—Method of denuding the sulcus. |
Emmet’s Operation (Figs. 45-55).—When the labia have been separated, it will be observed that there is a bulging or prominence of the lower portion of the posterior vaginal wall, which is called a rectocele. The most 81 prominent point or the apex of the rectocele should be held by a tenaculum or by a silk ligature passed immediately beneath the mucous membrane.
This point should be such that it may without undue traction be drawn to either orifice of the vulvo-vaginal glands.
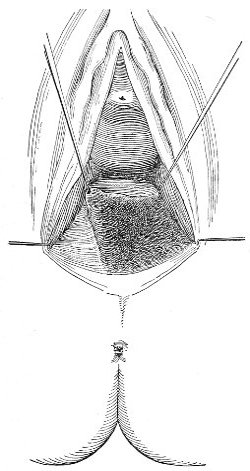 |
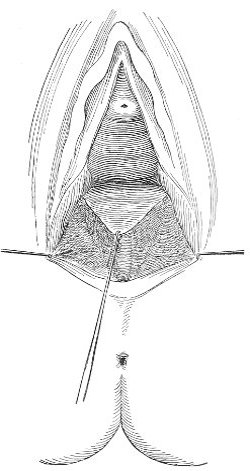 |
Fig. 48.—The left sulcus denuded. |
Fig. 49.—Both sulci denuded. |
If the apex of the rectocele is drawn to one side, there is formed on the other side a triangular area (Fig. 46, a, b, c). The base of this area (a, c) is at the ostium vaginæ. The inner side (a, b) runs along the side of the rectocele. The outer side (b, c) runs along the lateral vaginal wall. The apex b is approximately the highest point of the tear in the sulcus. The angle c is immediately below the orifice of the vulvo-vaginal gland. The angle b is fixed by a tenaculum held by an assistant, and the triangular 82 area is denuded. The denuded area does not correspond exactly with the original tear in the sulcus, but the denudation exposes the sulcus, so that sutures may be passed in such a way as to include the muscles and fascia. The sulcus on the opposite side is then denuded in a similar manner, and the lower face of the rectocele is denuded. It is best to begin the denudation by seizing with tissue-forceps the mucous membrane of the posterior vaginal wall at the ostium vaginæ, at the junction of skin and mucous membrane, and to remove contiguous strips of tissue by cutting upward toward the apex of the vaginal sulcus (Fig. 47).
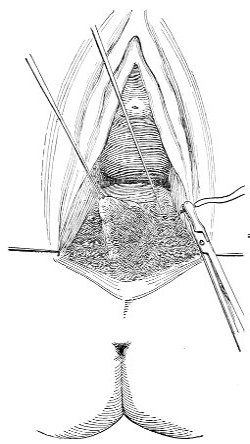 |
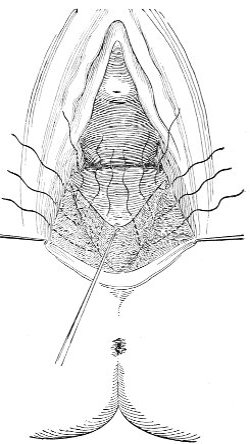 |
Fig. 50.—Introduction of the sutures. The point of the emerging needle is held by the tenaculum. |
Fig. 51.—Sutures introduced in both sulci. |
In the denudation no skin is sacrificed. The denudation is not carried below the line of junction of vaginal mucous membrane with skin. 83
Each sulcus is closed by sutures separately, as in the immediate operation. The first suture is passed across the upper angle b.
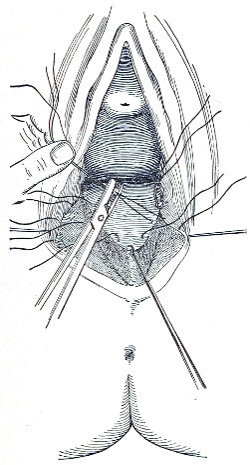 |
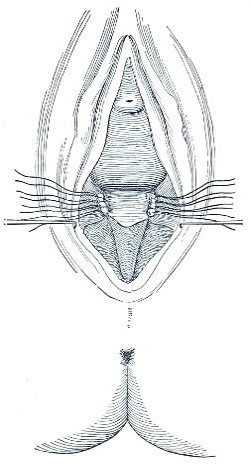 |
Fig. 52.—Method of securing sutures with perforated shot. |
Fig. 53.—Both sulci are closed. The support of the perineum is restored. The posterior wall of the vagina is brought forward. The rectocele is cured. |
The second suture is introduced about an eighth of an inch from the edge of the mucous membrane on the left vaginal wall, is passed backward, downward, and outward so as to grasp retracted muscular fibers, and is made to emerge at the bottom of the sulcus. It is then re-introduced and passed forward between the mucous membrane of the rectum and the denuded surface, and somewhat upward, to emerge on the edge of the mucous membrane of the rectocele. A third and, if necessary, 84 a fourth suture are passed in a similar manner. Similar sutures are then passed to close the right-hand sulcus.
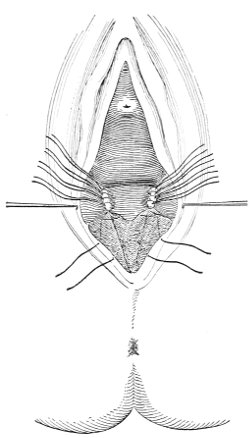 |
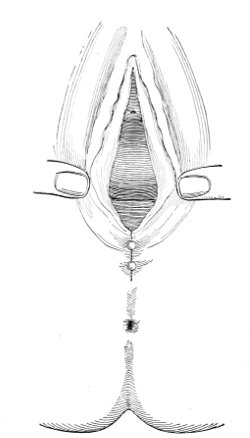 |
Fig. 54.—Sutures for closing the superficial perineum and fourchette. The anterior suture is called the “crown suture.” |
Fig. 55.—Emmet’s operation of perineorrhaphy completed. Compare this figure with that representing the condition of the parts before operation (Fig. 45). |
The sutures thus far introduced are sufficient to close the sulci, and therefore to restore the supporting structures of the perineum. The remaining sutures are merely to close the skin-perineum. The first of these sutures is called the crown suture. The needle is introduced on the cutaneous aspect of the perineum, at the anterior end of the lateral denudation. It passes outside of the denuded area, and emerges within the denuded area, at the edge of the mucous membrane of the vaginal wall, immediately below the last suture of the 85 sulcus. It is then passed so as to transfix the rectocele beneath the mucous membrane, and across the lateral denudation on the other side. When this suture is shotted the fourchette is restored. A second suture behind the crown suture is usually necessary to complete the closure of the skin-perineum.
The sutures in the sulci are shotted first, then the external sutures are shotted.
The second and third varieties of perineal injury are sometimes found associated in women who have borne more than one child, the injuries having in all probability occurred at different labors. In such a case the sulci should be denuded and closed as already described, and then the skin-perineum and the sphincter ani should be repaired.
Subcutaneous Laceration of the Muscles and Fascia.—The fourth variety of injury to the perineum—subcutaneous laceration of the muscles and fascia—is not uncommon. The structures which compose the pelvic floor are of different degrees of elasticity, and sometimes the mucous membrane and skin at the vaginal outlet will stretch, and not rupture, before the advancing head of the child, while the underlying structures—the muscles and fascia—may give way. Therefore the injury is said to be a subcutaneous laceration. The sphincter ani is never involved in this form of injury. The injury always takes place in the direction of the vaginal sulci, and the supporting muscles of the pelvic floor and the planes of fascia are the structures which are torn. The disability is exactly the same as in the third variety of perineal tear, with the absence of laceration of mucous membrane and skin.
It is not to be expected that this injury will be positively recognized at the time of labor, and therefore the immediate operation cannot be applied to it. The condition is often described as relaxation of the perineum. The disabilities following this injury, and the tests by which it may be recognized, are identical with those 86 already described under old lacerations in the sulci. The treatment is also the same. The vaginal sulci must be denuded as though the mucous membrane had in reality been torn, and the sutures must be introduced in such a way as to bring back the muscles and the fascia to the former attachments. 87
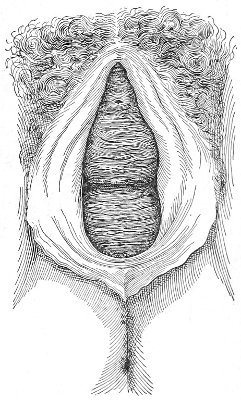
Fig. 56.—Rectocele and cystocele.
Rectocele.—A rectocele (Fig. 56) is the tumor formed by the protrusion of the lower part of the posterior vaginal wall into the vagina or through the ostium vaginæ. The condition is due to a prolapse of the posterior vaginal wall, and is caused by the loss of the support of the perineum, usually the result of laceration at childbirth. Sometimes the mucous membrane of the vagina alone prolapses, the anterior wall of the rectum remaining in place. Usually, however, the anterior rectal wall and the posterior vaginal wall protrude together. If the rectocele is not so extensive as to protrude through the ostium, the woman may be unaware of its existence. In many cases, however, the prolapsing vaginal wall protrudes at the vulvar cleft when the woman is erect, or when she strains at stool or performs work requiring heavy lifting. The woman often says that under such circumstances the “womb” protrudes. On account of the accompanying prolapse of the anterior rectal wall the passage of feces does not take place in the normal direction, but the fecal mass is forced 88 into the pouch of the anterior wall of the rectum, and straining efforts push it forward into the vagina. The woman says she feels as though the passages were about to take place through the vagina. This discomfort is relieved by pressing the rectocele back with the finger during defecation. Accumulation of feces in the rectal pouch may result in inflammation or ulceration. The condition is readily recognized by introducing a finger into the rectum, when it will be found to enter the rectocele.
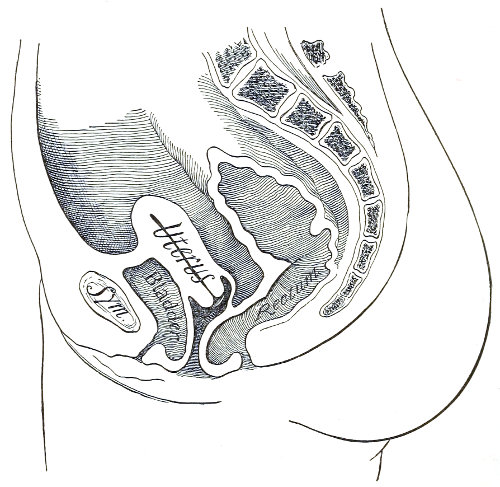
Fig. 57.—Median sagittal section of the pelvis of a woman in whom there has been a laceration of the perineum in the sulci, with rectocele and cystocele. The vagina is no longer a closed slit.
A rectocele is cured by Emmet’s operation, which restores the support of the perineum and the posterior wall of the vagina.
Cystocele.—A cystocele is a tumor formed by the protrusion 89 of the lower part of the anterior vaginal wall into the vagina or through the ostium (Fig. 56). The prolapse of the vaginal wall is accompanied by prolapse of the posterior wall of the bladder. A sound introduced into the bladder through the urethra will be found to enter the cystocele. This test, and the soft, reducible character of the cystocele tumor, enable us to diagnosticate between cystocele and cyst of the anterior vaginal wall. The condition is caused by a loss of the support of the anterior vaginal wall that is furnished by the posterior wall and the perineum.
In a case of cystocele residual urine often remains in the pouch of the bladder-wall. In some cases the woman learns that, in order to empty the bladder, it is necessary for her to push the cystocele upward and forward at every act of micturition. The result of this inability to empty the bladder is decomposition of the urine and resulting cystitis.
Many cases of so-called irritable bladder and chronic cystitis are caused primarily by laceration of the perineum, which produces cystocele or prolapse of the posterior wall of the bladder; and such cases can be cured only by curing the cystocele.
A cystocele varies much in size. Every long-standing case of laceration of the perineum in the sulci presents a certain degree of prolapse of the anterior vaginal wall. The tumor may remain within the vagina and be rendered prominent only upon efforts at straining, or it may protrude through the vulva as a mass the size of a duck’s egg.
As a cystocele is caused by laceration of the perineum, it can be cured only by repair of this laceration. The most important part of the treatment, therefore, is perineorrhaphy, which should always be performed. Usually this operation is sufficient. If the anterior wall of the vagina is supported, the tissues will recover their tonicity and contract, and the tumor will disappear.
In some cases, however, where the mucous membrane 90 of the anterior vaginal wall has become much stretched and redundant in the normal-sized vagina, it is advisable, in addition to the perineorrhaphy, to perform a plastic operation on the anterior wall in order to diminish the area of the vaginal mucous membrane. Such an operation is called anterior colporrhaphy. A variety of operations of this kind have been invented. The various forms are modified according to the requirements of the case and the whims of the operator. In one form of operation an oval area is denuded (Fig. 58), and the edges are brought together by interrupted sutures passed beneath the whole denuded surface.
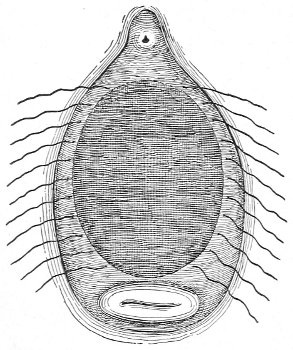
Fig. 58.—Oval denudation for cystocele: sutures introduced.
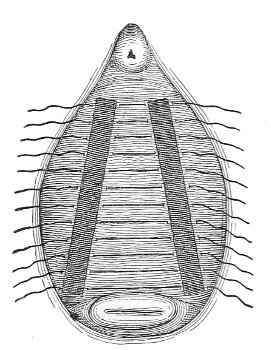
Fig. 59.—Sims’ operation for cystocele.
As the transverse measurement of the vagina is greater in the upper than in the lower part, an operation by which a greater amount of the excess of tissue is taken in above than below is often desirable. Such an operation is represented in Fig. 59. Two strips, about one-third to one-half inch in breadth, are denuded on each side of the anterior wall, extending from the position of the internal urinary meatus upward toward the lateral vaginal fornices. The length of these strips varies with the case, and depends upon the size of the upper portion of the vagina. It is often desirable to carry the 91 denudation to the level of the external os. The denuded surfaces are brought into apposition by interrupted sutures. By this operation the whole caliber of the vagina is narrowed from above downward. The degree of divergence of the denuded strips may be determined by seizing portions of tissue with tenacula upon each side and bringing them together, thus determining the amount of tension which will be put upon the sutures.
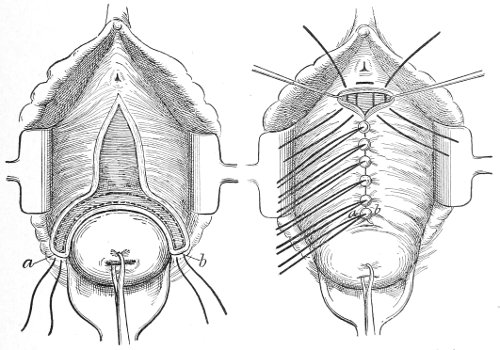
Fig. 60.—Dudley’s operation for cystocele (Ashton, modified from Dudley).
In Dudley’s operation the denudation is made and the sutures are introduced as shown in Fig. 60. The advantage claimed for this operation is that by it the upper end of the vaginal wall is attached to the bases of the broad ligaments.
The operation of anterior colporrhaphy must always be accompanied by perineorrhaphy. The anterior operation should be performed first. The woman should be placed in the Sims or the dorsal position.
Enterocele.—Enterocele, or entero-vaginal hernia, is a rare condition. It consists of a hernia, or prolapse, of 92 the intestine into the vaginal canal. Two forms of the disease have been described—the anterior and the posterior. The latter is the more common. In the posterior variety one or more loops of the intestine, or the omentum, reach the bottom of Douglas’s pouch and push the posterior vaginal wall forward, so that it encroaches upon the vaginal canal and in some cases protrudes from the ostium vaginæ.
The causes of this disease are not known. It is probably favored by loss of support of the perineum and the vaginal walls. An unusually deep pouch of Douglas would predispose a woman to this condition.
In the anterior form of the disease the hernia occurs at the bottom of the vesico-uterine pouch.
The posterior enterocele may be distinguished from rectocele by introducing a finger into the rectum and one into the vagina, when the prolapsed intestine or omentum may be felt between the anterior rectal wall and the posterior vaginal wall. The condition may be distinguished from vaginal cyst by percussion and palpation.
In the treatment of enterocele any existing injury to the perineum should be repaired, and the vagina should be narrowed by one of the plastic operations already described. Great care should be taken not to injure with the needle the intestine underlying the vaginal wall.
Subinvolution of the Vagina.—It should be remembered, in connection with the subject of prolapse of the vaginal walls as a result of loss of the perineal support, that there is always present, also, a condition of subinvolution of the vagina. During pregnancy all the elements of the vagina undergo a physiological hypertrophy analogous to that which occurs in the uterus. After labor the vagina normally undergoes certain changes by which it is again approximately restored to the dimensions, shape, etc. that existed before pregnancy. This change is called the involution of the vagina. Anything that arrests this process of involution produces a state of 93 subinvolution of the vagina; this structure is then found much larger and more relaxed than normal, and a certain hypertrophy of all the elements of the vaginal walls persists. Such subinvolution of the vagina is caused by the various pelvic lacerations, which, by causing loss of support to the pelvic vessels, result in a state of passive congestion.
These redundant vaginal structures usually disappear and contraction takes place after the operation of perineorrhaphy. In some cases, however, when the vagina is very much larger and more relaxed than normal, it is advisable to remove some of the excess of tissue by a plastic operation on the anterior wall similar to that described for the relief of cystocele. 94
The uterus normally lies with its anterior surface in contact with the posterior aspect of the bladder, no intestines intervening. The absolute and relative positions of the uterus depend upon the degree of distention of the bladder and the position of the woman. The uterus is pushed backward and the fundus is turned upward by distention of the bladder. When the woman is erect the uterus lies at a slightly lower level than when the woman is on her back, and the intra-abdominal pressure 95 acting upon the posterior surface of the fundus turns the uterus more forward, so that the fundus lies nearer the symphysis pubis. Fig. 61 shows about the normal range of position.
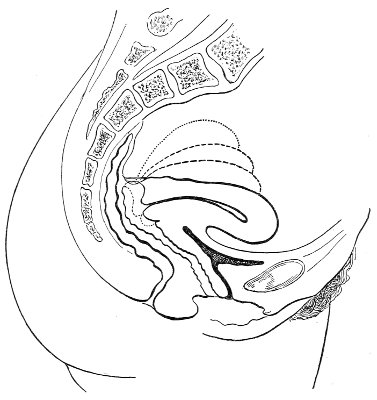
Fig. 61.—Normal range of position of the uterus, depending upon the distention of the bladder.
It may be said that in the normal woman the long axis of the uterus is approximately perpendicular to the long axis of the vagina (Fig. 62).
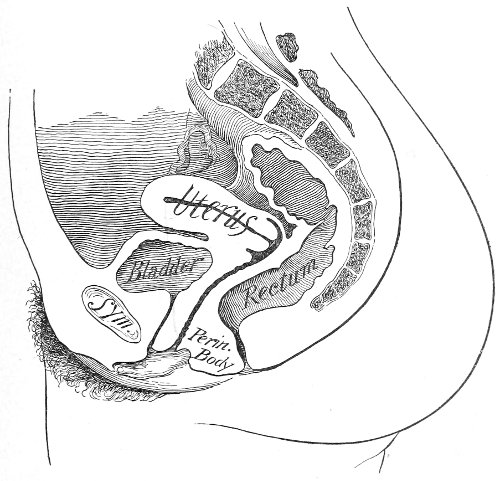
Fig. 62.—Median sagittal section of the normal female pelvis.
The uterus does not surmount the vagina with the axes of the two structures in the same line, as is shown in some anatomical plates.
The cervix looks backward toward the coccyx, from the tip of which it is situated 0.6 to 1.2 inches.
The uterus is maintained in position by a variety of factors. The ligaments, which have been described, are eight in number—broad ligaments, round ligaments, utero-sacral and utero-vesical ligaments. 96
With the exception of the round ligaments, which are muscular structures, the uterine ligaments are formed by peritoneal folds, including connective tissue, blood-vessels, lymphatics, and a small amount of unstriped muscle.
When the woman is erect the insertions and origins of the various uterine ligaments lie in the same horizontal plane. The insertion of no ligament is higher than its origin in the uterus; therefore these ligaments do not act as suspensory ligaments when the uterus is in its normal position. The truth of this fact is repeatedly demonstrated at operations. If the cervix be caught with a tenaculum when the woman is on her back, the uterus may, with but very little force, be drawn downward toward the ostium vaginæ to the extent of one or two inches; and similarly, by a slight digital pressure on the cervix, the uterus may be pushed upward from one to two inches above its normal position.
The ligaments of the uterus act as guys. They steady it, and prevent too great lateral and fore-and-aft movement; they do not, when the uterus is in its normal position or at its normal level, sustain it against the force of gravity. When, however, the uterus, for any reason, falls an inch or more below its normal level, the uterine ligaments become suspensory in character.
In the normal woman the vagina is always closed. As has already been said, it is a slit in the pelvic floor, valvular in character; consequently the abdominal and pelvic viscera may be considered to be contained in a closed vessel, in woman as well as in man. The uterus floats in this closed vessel at a level which is consistent with its own specific gravity. If, for any reason, the specific gravity of the uterus were increased, it would sink below the level at which it is normally situated.
Since, normally, there is no tendency in the uterus to change its position, the pressure upon it must be equal in all directions. The subject may perhaps be better understood by referring to a few simple facts in hydrostatics. If a fluid contained in a closed vessel be in a condition 97 of equilibrium so that its various particles are at rest, then the pressure upon any particle is equal and opposite in all directions (Fig. 63); otherwise the particles would not be in equilibrium, but would move. The bottom of such a vessel, however, is not, like the particles of the fluid, surrounded on all sides by the fluid, but above it is the fluid, and below it is the atmospheric air. Any point upon the bottom of the vessel is subjected to a downward pressure equal to the weight of the column of fluid above the point; this downward pressure is resisted by the strength of the material composing the vessel. If this material be yielding or elastic in character, the pressure above will make the bottom protrude to a certain extent. A particle within the fluid (like X immediately above the bottom of the vessel) will be subjected to a downward pressure equal to the weight of the column of fluid above it; but this pressure will be counterbalanced not by any strength in the particle, but by a counter-force acting from below equal and opposite to that acting from above.
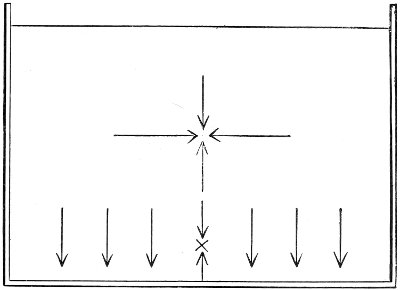
Fig. 63.—Vessel containing fluid in equilibrium. The arrows indicate the direction of the pressure at various points.
A similar state of things exists in the female pelvis. The uterus floats at a certain level, and the intra-abdominal pressure acting from above is counterbalanced by an 98 equal force acting from below, while the floor or bottom of this vessel (part of which is the perineum) is subjected to a force from above equal to the intra-abdominal pressure, and this force is opposed only by the strength of the perineum (see Fig. 64).
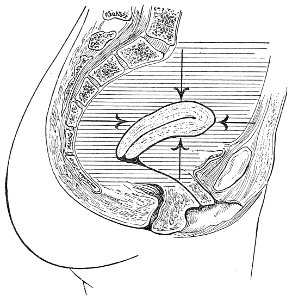
Fig. 64.—Diagram representing the directions of the intra-abdominal pressure upon the uterus in the uninjured woman.
If the vagina were an open tube admitting air, so that the uterus above was in contact with the contents of the pelvic vessel and below with atmospheric air, then the condition of things would be altered. In this case the uterus would in reality become part of the floor of the vessel, and would be subjected to a pressure from above equal to the intra-abdominal pressure, and to this pressure would be opposed only the strength of the uterus and its attachments. Such a state of things occurs when the perineum is torn and the vagina becomes a patulous open canal, and not a closed slit. Therefore when the opening of the vagina is torn and air constantly enters the vaginal canal, the normal hydrostatic equilibrium of the pelvic contents is destroyed, the resultant of the forces acting upon the uterus is downward, and the organ has a tendency to fall or to prolapse (Fig. 65).
The normal perineum and vagina do not sustain the 99 uterus by furnishing a mechanical support from below, any more than the bottom of a vessel sustains any single particle of fluid floating in it.
When the uterus tends to fall down or to prolapse, its progress is opposed at a certain level by its various attachments. The ligaments become suspensory in character as soon as their uterine attachments are below their pelvic attachments. The cellular tissue, fat, blood-vessels, etc. connected with the uterus restrain its downward motion. And, finally, this motion is restrained by what has been called the “retentive power of the abdomen,” which is merely the atmospheric pressure acting from below on the contents of a vessel the top and sides of which are closed.
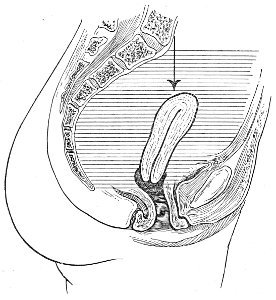
Fig. 65.—Diagram representing the direction of the intra-abdominal pressure in the woman with a laceration of the perineum.
Refer again to a simple physical example: If a glass tube be filled with water, a finger placed over one end, and the tube inverted, the water will not run out: it is sustained by atmospheric pressure acting from below. If the finger be removed, atmospheric pressure also acts from above, and the water will fall. If a hole be made in the side of the tube, atmospheric pressure will act through it, and the water below the hole will fall. 100
In order that the column of water be sustained, the sides of the tube must be rigid or unyielding. If the sides of the tube yielded slightly to atmospheric pressure, they would sink in and a certain amount of water would escape.
The abdominal and pelvic cavities in the erect woman may be considered as a tube filled with fluid contents. The top of the tube is closed by the diaphragm; the sides are the more or less rigid abdominal walls and the back; the floor is the perineum. When the floor is destroyed a hole is made in the bottom of the tube: the contents tend to fall, but the fall is resisted by atmospheric pressure acting from below. If the diaphragm and the parietes were rigid as glass, there would be no prolapse, any more than there is prolapse of the water in the glass tube. If the parietes yield somewhat, the amount of fall or prolapse is proportional. Thus the retentive power of the abdomen is dependent upon the strength or rigidity of the abdominal walls. 101
Prolapse of the uterus means a falling of that organ below its normal level. The condition is popularly spoken of as “falling of the womb.” There are an infinite number of degrees of prolapse of the uterus, between the slightest descent on the one hand and complete protrusion of the organ from the body on the other hand. The term “complete prolapse” should properly be applied to the entire protrusion of the uterus outside of the vulva. This condition, however, is most unusual. The term is generally used to designate those cases in which the cervix alone, or the cervix and part of the body of the uterus, protrude from the vulva (Fig. 66). In any case of prolapse of the uterus it is best to describe in detail the extent of the prolapse and the other conditions present. Thus, some of the various kinds of prolapse may be described as follows: “Prolapse of the uterus, the cervix resting on the pelvic floor;” “prolapse of the uterus, the cervix presenting at the vulvar cleft;” “prolapse of the uterus, the cervix protruding about two inches from the ostium vaginæ, with elongation of the supra-vaginal cervix,” etc.
Injury to the pelvic floor that allows air to enter the vagina destroys the normal equilibrium of the pelvic contents and exposes the uterus to a direct abdominal pressure from above, which is not counterbalanced by an equal force from below, but is opposed by the strength of the uterus and its attachments and the retentive power of the abdomen. Most cases of prolapse occur in women in whom the perineum has been injured at childbirth.
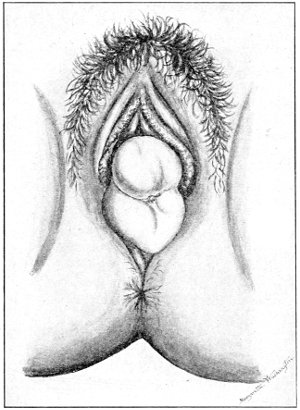
Fig. 66.—Prolapse of the uterus, the cervix protruding from the vulva. There is a bilateral laceration of the cervix.
There are a number of predisposing causes of uterine 102 prolapse that permit the descent to progress after the uterus has begun to fall—namely: Relaxation of the uterine ligaments that results from too frequent parturition, from old age, or from tissue-weakness which is part of a general condition, the uterine ligaments sharing the general feebleness of the other tissues and structures of the body; relaxation, loss of rigidity, or muscular weakness of the abdominal parietes, which diminishes the retentive power of the abdomen; diminution of the cellular tissue and the fat of the pelvis, such as occurs in wasting disease or in old age. Anything that suddenly increases the intra-abdominal pressure, such as lifting a heavy weight, may cause acute prolapse of the uterus. In some cases the uterus has suddenly protruded from the body as a result of heavy lifting. In cases of this character 103 it is probable that the muscular supports of the perineum have been weakened from some cause, or that the sudden increase of abdominal pressure drives the uterus downward before the perineal muscles have time to contract and close the vaginal outlet. In such cases there is also present rupture of the uterine ligaments. Constant violent coughing has produced uterine prolapse in a similar way.
Extreme uterine prolapse sometimes occurs in a nulliparous woman in whom the perineal supports are naturally weak. In such women there exists a condition of relaxation identical in results with subcutaneous laceration of the perineum.
Anything that increases the specific gravity of the uterus will make it sink somewhat lower in the pelvis. Subinvolution, congestion from inflammation, or retroflexion may do this. In such cases, however, the prolapse never becomes extreme, rarely extending beyond a slight sinking of the uterus.
In most cases uterine prolapse takes place slowly. Sometimes many years are necessary for the development of complete prolapse. The equilibrium of the pelvic contents is destroyed by one of the causes already mentioned. The uterus falls through a certain distance before the uterine ligaments become suspensory. Then, however, its further descent is impeded.
If the original cause continues to act, the uterine ligaments become stretched and the descent of the uterus gradually progresses, impeded to a varying degree also by the retentive power of the abdomen and the cellular tissue and other pelvic attachments.
As the uterus descends, the vaginal walls attached at the cervix are dragged down with it, so that when the prolapse becomes complete the vagina is turned inside out (Fig. 67).
When the perineum has been injured so that the lower portion of the vagina loses its support and the equilibrium of the pelvic contents is destroyed, two distinct 104 phenomena occur: The uterus falls as already described, and at the same time the lower part of the vagina begins to fall, so that there appear a prolapse of the anterior vaginal wall, or a cystocele, and a prolapse of the posterior wall, or a rectocele. The condition finally produced will depend upon which prolapse takes place the more rapidly—that of the vagina or that of the uterus.
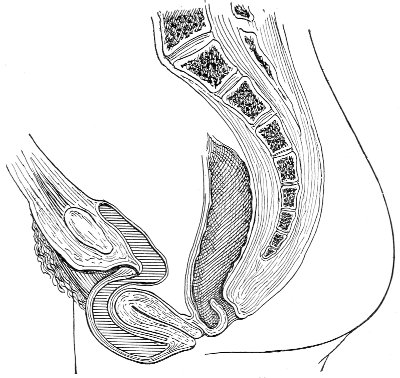
Fig. 67.—Complete prolapse of the uterus.
If the prolapse of the lower vagina progresses faster than that of the uterus, then the vagina will begin to drag upon the cervix, to which it is attached, and under these circumstances the uterus will be subjected to two downward forces—intra-abdominal pressure from above, and traction of the vaginal walls acting from below.
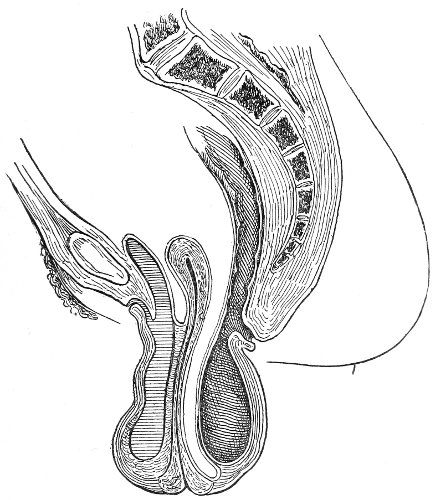
Fig. 68.—Prolapse of the vagina and the vaginal cervix, with great elongation of the supra-vaginal cervix.
As the traction is exerted upon the lower part of the cervix, and the body of the uterus is sustained by the uterine ligaments, which resist the downward traction, the isthmus, or point of junction of the body and cervix, is dragged out or stretched, so that in some cases a very 105 marked elongation of the supra-vaginal cervix, or the part of the cervix above the vaginal junction, appears. This elongation is sometimes so great that the length of the uterine cavity from external os to fundus measures six or eight inches. Such elongation of the cervix is usually found to a greater or less degree in every case of marked prolapse of the uterus caused by injury to the perineum. Such a condition should be described as prolapse of the uterus with elongation of the supra-vaginal cervix (Fig. 68). In many cases the prolapse of the vagina and the elongation of the cervix are the most marked features, the body of the uterus falling but slightly below its normal level. The cervix will be found protruding some distance from the vulva; the vagina will be found 106 turned inside out; while the fundus may be felt approximately at its normal level in the pelvis, and the presenting cervix and the body of the uterus are connected by a round, cord-like structure about the size of the little finger, which is the stretched, attenuated supra-vaginal cervix.
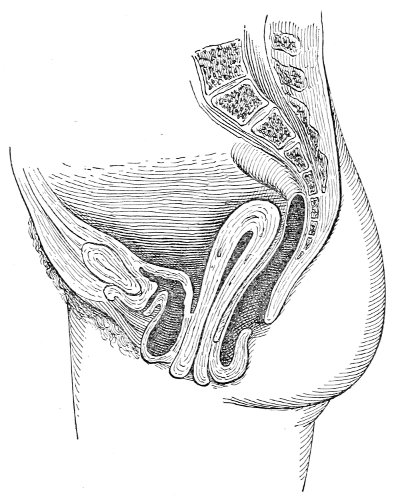
Fig. 69.—Prolapse of the vagina and cervix, with elongation of the supra-vaginal cervix.
As a result of the traction upon the cervix the blood-flow from the infra-vaginal cervix is impeded, and passive congestion results in hypertrophy. This hypertrophy is increased by irritation of the infra-vaginal cervix from friction against the clothing and from urine, etc. In such cases the presenting cervix becomes much larger than normal, sometimes measuring two or two and a half inches in diameter.
It will be seen that very pronounced structural changes are present in old cases of prolapse of the uterus. The uterine ligaments and the pelvic attachments become so stretched and atrophied that they can never become functionally useful again. The normal shape and size of the 107 uterus become very much changed from elongation of the supra-vaginal cervix and hypertrophy of the infra-vaginal cervix. The vaginal canal becomes patulous and stretched several times beyond its normal dimensions, and the delicate mucous membrane, from exposure, becomes tough and cutaneous in character. The large protruding mass of uterus and inverted vagina stretches the genital outlet far beyond its normal dimensions, and the muscular supports that may have remained after the original perineal injury undergo atrophy from pressure.
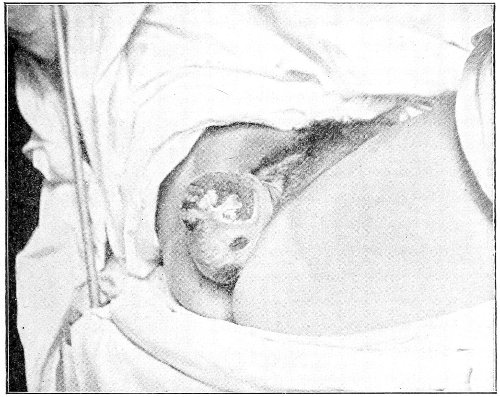
Fig. 70.—Prolapse of the vagina and the vaginal cervix, with elongation of the supravaginal cervix. Extensive ulceration.
Accompanying the prolapse of the uterus is usually prolapse of the bladder and of the anterior wall of the rectum, producing a condition already described under Cystocele and Rectocele.
Women who do hard manual labor are those who suffer with the most marked forms of uterine prolapse. The form of prolapse accompanied by elongation of the supra-vaginal cervix is usually characteristic of the hard-working 108 woman. Such prolapse of the uterus is common among the Western Indian women, who return immediately after delivery to hard labor and horseback-riding.
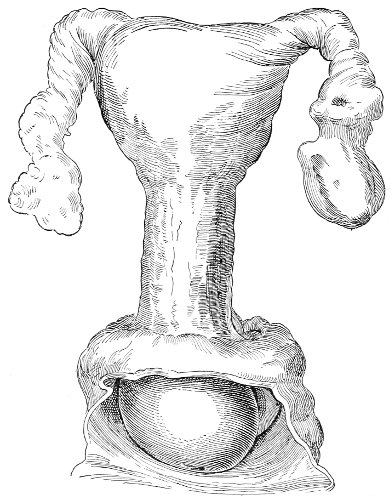
Fig. 70, A.—Elongation of supra-vaginal cervix (St. Bartholomew’s Hospital Museum).
Many cases of prolapse would be avoided, even though there might be serious perineal injury, if women remained in bed a sufficient time after delivery. By rising too early prolapse is favored, for a variety of reasons. The uterus is large and heavy; the uterine ligaments are elongated, and the abdominal walls are weak; consequently the retentive power of the abdomen is poor; the vagina is flabby and much larger than normal; the genital outlet has not contracted, and the muscular and fascial supports which may not have been torn are stretched and relaxed.
The subjective symptoms of prolapse vary greatly and are not characteristic. A woman in whom the uterus has 109 descended but slightly below the normal level may suffer so much with backache, weakness of the legs, and a feeling of pelvic weight, or “bearing down,” that her life will be rendered useless; while, on the other hand, a woman with complete prolapse of the uterus may suffer no inconvenience except from the presence of the protruding mass. In fact, the lesser degrees of prolapse seem to cause more suffering than the extreme degrees.
The first subjective symptoms of injury to the supports of the pelvic floor that appear when the woman leaves her bed are those referable to beginning prolapse of the uterus. Backache is the most common symptom, and occurs here as in almost every other disease of the uterus. The pain, a dull ache, is situated in the upper part of the sacrum. It is increased by standing, by walking, or by manual labor. It often disappears entirely when the woman lies down and the intra-abdominal pressure is removed from the uterus. Headache situated in the occipital region or the vertex is also usually present, and varies in severity with the severity of the backache.
Pain extending down the posterior aspect of the thighs, and a dragging feeling of loss of support in the pelvis, may also be present. The rectal and bladder symptoms occur later, when rectocele and cystocele appear.
There is often very marked general physical weakness, much of which may be referred directly to the loss of the muscular support of the perineum. Almost every effort that the woman makes is accompanied by increase of intra-abdominal pressure, and she feels keenly the loss of the accustomed perineal support which normally resists any increased abdominal pressure. In the sound woman the perineal muscles contract and the vagina is more tightly closed to meet the increased pressure incident to a muscular effort. In the injured woman the vagina is open and the pressure is resisted by weak vaginal walls and uterine supports. She feels that her point of resistance is gone. The best proof of the profound effect of injury to the perineum upon the general strength of a woman is given by the operation of perineorrhaphy. 110 The repair of this apparently slight lesion restores the woman to her former strength.
The diagnosis of prolapse of the uterus is readily made by examination. In the extreme cases the cervix and the greater part of the body of the uterus are found outside the vulva. In less marked cases the cervix is seen presenting at the vaginal orifice as soon as the labia are separated. In other cases the cervix is felt by the vaginal finger resting on the pelvic floor. It should be remembered that every case of prolapse is greater when the woman is standing than when she is being examined upon her back. Sometimes the cervix will present at the vulva, where it may be felt when the woman is erect; but when she lies down and intra-abdominal pressure is removed, it retreats beyond inspection except through the speculum. In order to determine the full extent of prolapse, therefore, when the woman is examined on her back she should be directed to strain or bear down, when much more marked descent of the uterus and vaginal walls will become apparent.
The lesser degrees of prolapse, in which the cervix has not yet fallen enough to rest on the pelvic floor, are more difficult to recognize by bimanual examination. It will be found that the upward range of motion of the uterus is greater than normal, and vaginal examination when the woman is erect will make the condition more apparent.
Extreme prolapse of the uterus, in which we find protruding from the vulva a pear-shaped tumor at the apex of which is the opening of the cervical canal, should not be mistaken for any other condition. Inversion of the uterus and a uterine polyp resemble it only in shape, and in no other particular. If there is any doubt, it may be dispelled by placing the woman in the knee-chest position, when the prolapse may readily be reduced and the normal anatomical relations restored.
Treatment.—As prolapse of the uterus is usually caused by injury to the pelvic floor, treatment should be directed in the first place to the restoration of the perineum. 111
In slight cases of prolapse that are seen early, restoration of the perineum by Emmet’s operation is sufficient for cure.
In cases of long duration, however, we have to deal with a variety of secondary conditions. These are as follows: Hypertrophy of the uterus from subinvolution or congestion; elongation of the cervix; hypertrophy of the cervix; elongation of the uterine ligaments; stretching of the vagina; stretching of the genital outlet; and atrophy of all the structures of the perineum from pressure. The atrophic changes give the most difficulty. The prognosis, therefore, depends upon the duration of the case.
In cases of prolapse in which the cervix has reached or has passed the ostium vaginæ, rest in bed in the recumbent position should always be prescribed for two to four weeks before any operative procedure. The woman should be placed in the knee-chest position and the prolapse of the uterus and vagina should be reduced. Reduction of this kind should be practised as often as the prolapse returns—as, for instance, after straining at stool. It may be performed by the woman herself or by the nurse. It is well for the woman to assume the knee-chest position three or four times a day, for five to fifteen minutes at a time. One or two hot vaginal douches of a gallon of 1:4000 bichloride solution should be administered daily. The intestinal contents should be kept soft by laxatives. As a result of such preparatory treatment the uterus will diminish very much in size, and the vagina and the vaginal outlet will contract, so that at the time of operating the amount of tissue to be removed may be more accurately determined. The diminution in the length of an elongated cervix as a result of rest is most striking, and demonstrates the truth of the explanation of the etiology of this condition that has already been given. A uterine canal that measures five or six inches in length may be reduced to three or four inches after traction on the cervix has been removed by rest in bed. 112
Ulceration of the cervix, which is often present as a result of friction from exposure, readily yields to this treatment of rest and douches.
From the considerations already referred to it will be seen that the operative treatment of any case of uterine prolapse varies according to the special conditions present.
Perineorrhaphy is always necessary. Emmet’s operation is usually the best one. The denudation in the lateral vaginal sulci should be extended well up the posterior vaginal wall, in order to diminish the caliber of the overstretched vagina. One of the operations already described should also be performed for the cure of the cystocele and to diminish the area of the anterior vaginal wall. The best of these operations are Sims’ and Dudley’s (Figs. 59 and 60). After all plastic operations for the cure of prolapse the woman should be kept in bed for three or four weeks—the longer the better—so that the perineal and vaginal structures and the ligaments of the uterus may contract and regain strength.
In some cases of long standing it is impossible, by operation, to restore the integrity of the pelvic floor, and to restore the shape, size, and direction of the vaginal canal so that the normal equilibrium of the pelvic contents will be re-established. In such cases operators have attempted to build a direct mechanical support for the uterus.
Le Fort’s operation is an ingenious method of attaining this object. The uterus should be replaced, and a longitudinal strip of tissue, about one-half to one inch in breadth and two to two and a half inches in length, should be denuded on the anterior vaginal wall, extending from a point near the vulva, where the two vaginal walls are in contact when the uterus is in place, up toward the cervix. A similar strip should be denuded on the posterior wall. These two denuded areas should be brought into apposition by interrupted sutures passed transversely. Perineorrhaphy should also be performed.
In those cases in which the vagina and the vaginal 113 outlet have become very much stretched by the protruding mass of prolapsed structures, Emmet’s operation seems to be insufficient. In such cases the following operation is useful. This consists in denuding a triangular area on the posterior vaginal wall (Fig. 77), the apex of the denudation being immediately below the cervix, and the base at the ostium vaginæ. The denudation should extend well on to the lateral vaginal walls. The denuded area is then closed by sutures passed transversely.
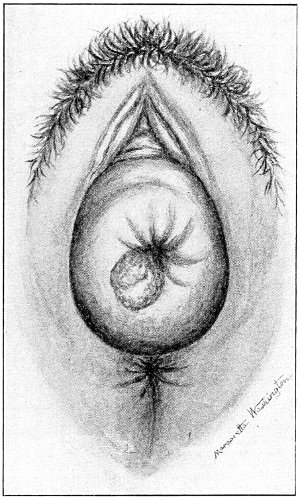
Fig. 71.—Prolapse of the vagina and of the infra-vaginal cervix. The sound showed the internal uterine length to be 5½ inches. An erosion appears on the posterior margin of the os uteri.
Judgment, derived from experience, is necessary in choosing and performing the various plastic operations for prolapse of the uterus.
In every case of prolapse a certain degree of retroversion of the uterus is present. In fact, the uterus could not escape from the vagina unless the fundus were turned somewhat backward. The operation of ventro-fixation of the uterus is therefore a useful adjunct in some cases 114 115 116 117 of uterine prolapse. The operation is not intended to furnish a mechanical support to the uterus, but only to keep it in a position of anteversion, so that it will less readily escape through the vaginal canal. The plastic operations and the ventro-suspension may all be done at the same sitting.
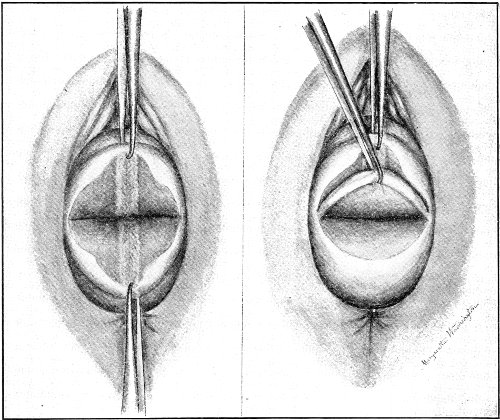
Fig. 72.—Amputation of the hypertrophied cervix: A. The cervix has been split laterally. B. The posterior lip is being amputated.
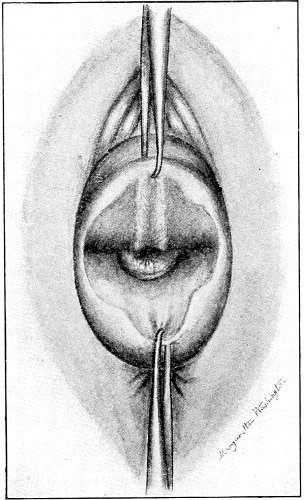
Fig. 73.—The posterior lip has been amputated.
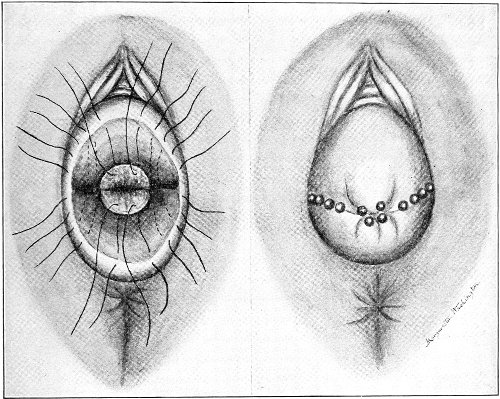
Fig. 74.—A. Both lips have been amputated and the sutures have been introduced. B. The sutures have been secured by the perforated shot.
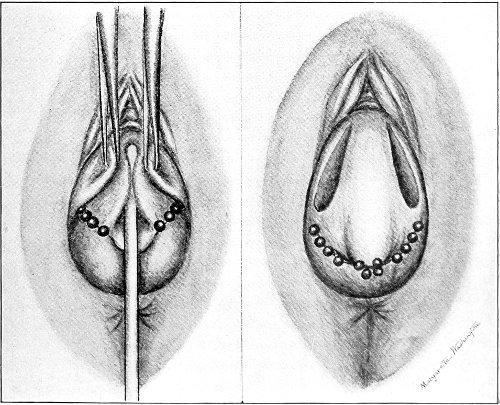
Fig. 75.—A. The anterior vaginal wall is pushed backward by the staff, while on each side of the median line portions of mucous membrane are grasped by tenacula and brought together in order to determine the position of the strips to be denuded. B. Denudation on the anterior vaginal wall (Sims’ operation).
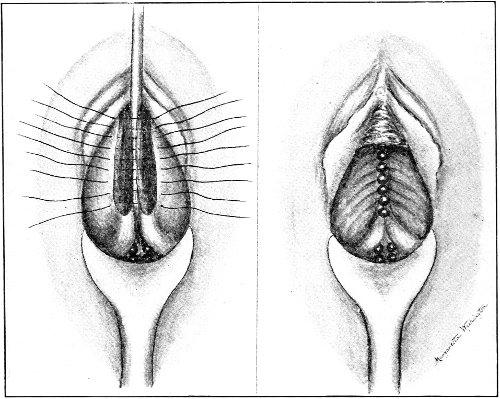
Fig. 76.—A. The sutures have been introduced. The prolapsed vagina and cervix have been reduced. The cystocele is pushed upward by the staff, so that the denuded strips may be brought into apposition. B. The sutures are secured. The cystocele has disappeared. The area of the anterior vaginal wall and the caliber of the vagina have been much diminished.
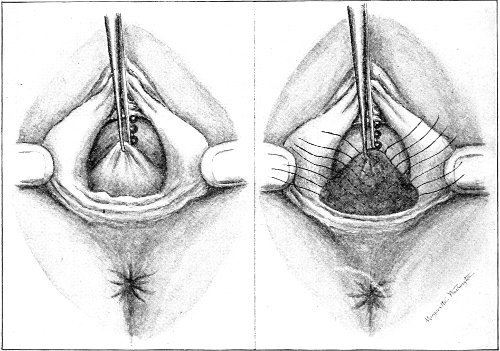
Fig. 77.—A. A point on the median line of the posterior vaginal wall, about an inch below the cervix, has been seized by the tenaculum. This marks the apex of a triangle the base of which is at the ostium vaginæ and the sides of which are on the lateral vaginal walls. B. The triangle has been denuded. The sutures have been introduced.
Whenever there is hypertrophy of the infra-vaginal cervix, this structure should be amputated in addition to the other operations.
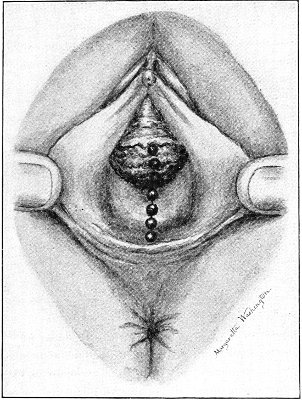
Fig. 78.—The sutures in the posterior vaginal wall have been secured. The caliber of the vagina has been very much diminished. A strong sling or band of tissue has been formed immediately above the ostium vaginæ, which supports the lower portion of the posterior vaginal wall. The operation is completed.
In those very rare cases of incurable prolapse that have resisted all conservative treatment the operation for the removal of the uterus may be considered. The writer has never resorted to it. The operation consists in supra-vaginal hysterectomy followed by fixation of the cervical stump by sutures to the abdominal wall.
This operation, however, should not be proposed hastily. 118 The surgeon should not become discouraged by one or even two failures of the more conservative methods of treatment. Though the first plastic operation may fail to retain the uterus inside the body, yet something is always accomplished by it, and when supplemented by a second or a third operation, cure will often result.
The operative procedures required in a case of prolapse of the vagina and of the infra-vaginal cervix, with hypertrophy of the infra-vaginal cervix and elongation of the supra-vaginal cervix, are illustrated in Figs. 71-78.
The condition represented in Fig. 71 is that which is commonly spoken of as “prolapse of the uterus.” It is the usual form of prolapse. It may be cured in the very great majority of cases by the operations which are here depicted.
A great number of mechanical devices have been introduced for the relief of prolapse of the uterus. Every vaginal pessary has been used for this condition. None of these implements cure the disease. All of them, if used continuously, produce ulceration of the vagina and of the cervix from pressure, and must be abandoned until such lesions heal. In those cases of prolapse in which pessaries remain in the vagina and support the uterus, without producing ulceration, operation would effect a cure.
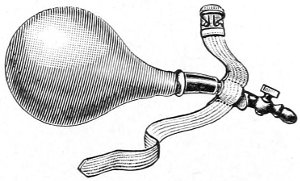
Fig. 79.—Braun’s colpeurynter.
Mechanical supports of this kind are only indicated in women in whom operation is contraindicated on account of old age or for some other reason. Perhaps the best instrument for supporting the uterus in such cases is Braun’s colpeurynter (Fig. 79). The uterus should be reduced, and the colpeurynter, well greased and containing about an ounce of water, should be introduced in the vagina and then distended with air. This instrument takes its support evenly from all parts of the vaginal outlet, and is therefore less apt to produce ulceration from pressure than the various pessaries. It should be removed at night. 119
As has already been said, the uterus normally lies with its anterior surface in contact with the posterior surface of the bladder, and with its long axis approximately perpendicular to the long axis of the vagina. The forward inclination of the uterus varies with the degree of distention of the bladder; it is greatest when the bladder is collapsed.
In the normal woman the long axis of the body of the uterus is inclined forward at an obtuse angle with the long axis of the cervix. In other words, the uterus is normally anteflexed. This angle is subject to rather wide variations within the limits of health. It is greater in the multiparous than in the nulliparous woman. It varies with the distention of the bladder, the position of the woman, and the intensity of intra-abdominal pressure. The axis of the uterus when removed from the body is usually straight. The anteflexion found in the organ when in situ in the living woman rarely persists. The normal or physiological anteflexion is maintained during life by the utero-sacral ligaments, which hold the cervix back, and the intra-abdominal pressure, which, acting upon the posterior aspect of the fundus, pushes the body of the uterus forward.
In the fetus and in early infancy the cervix is relatively much more developed than the body of the uterus, and there is a very marked angle of flexion between them.
Anteflexion of the uterus becomes pathological when 120 the bend in the cervical canal is sufficient to impede the escape of menstrual blood or other uterine discharges.
Obstruction of this kind depends upon two factors—the degree of the flexion, and the rigidity of the uterus, which diminishes the mobility that normally exists at the angle of flexion.
No matter how sharp the angle of flexion, it should not be considered a pathological condition unless obstruction in the cervical canal is present—unless the woman presents the symptoms of dysmenorrhea and sterility.
Three varieties of anteflexion have been described:
I. Corporeal anteflexion, in which the cervix has the normal backward direction, and the body of the uterus is bent forward upon it (Fig. 80).
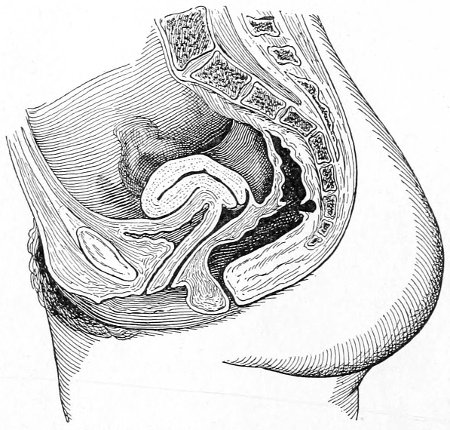
Fig. 80.—Corporeal anteflexion.
II. Cervical anteflexion, in which the axis of the body of the uterus is inclined forward to the normal degree, and the cervix is bent forward upon it (Fig. 81).
III. Cervico-corporeal anteflexion, when the cervix and body of the uterus are both bent forward upon each other (Fig. 82).
Anteflexion of the uterus is a disease of single and sterile married women. It is very rarely found in women 121 who have borne children. The disease is congenital or is caused by imperfect development during childhood.
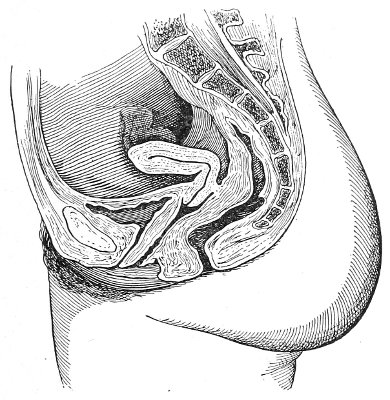
Fig. 81.—Cervical anteflexion.
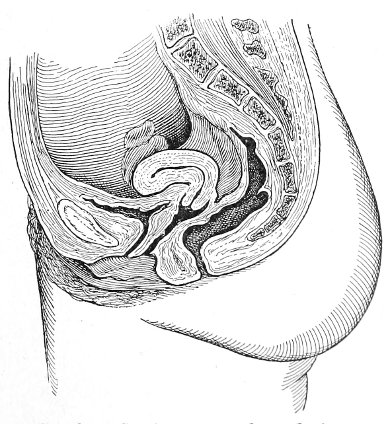
Fig. 82.—Cervico-corporeal anteflexion.
The fetal condition of a large cervix and a small, sharply-flexed body may persist. The posterior wall of the uterus may develop while the development of the anterior wall is arrested, and thus the uterus would be 122 flexed forward. A mark of such arrest of development is sometimes seen in the atrophied or undeveloped anterior lip of the cervix. Anteflexion is usually accompanied by a small, undeveloped condition of the whole of the uterus, and often by poorly developed vagina, tubes, and ovaries.
It is probable that improper dress and hygiene during the period of puberty have much to do with the development of anteflexion. The early menstrual history sometimes points to poor development of the sexual organs. The menses often make their appearance much later than usual—sometimes when a girl is nineteen or twenty years of age—and when established, the function is often irregular, the bleeding recurring at long intervals.
The most prominent symptom of anteflexion of the uterus is dysmenorrhea, or painful menstruation. The dysmenorrhea is characteristic: violent pains in the center of the lower abdomen, extending down the thighs, occur for several hours before the bleeding begins. In the later years of the disease the pain extends to the whole of the pelvis and the back. The pain is caused, in all probability, by the accumulation of blood behind the obstruction in the cervical canal. When the blood begins to escape freely, the pain is relieved, and may be absent during the remainder of the menstrual period. The blood is often clotted during the first part of the flow. Nausea and vomiting may be present during the height of the pain.
The menstrual period may be followed by several days of great physical weakness and debility.
Unless relieved by pregnancy or by proper treatment, the anteflexion will persist during the menstrual life of the woman. The suffering increases with time. Endometritis, salpingitis, and ovaritis follow old cases of anteflexion.
Sterility usually accompanies well-marked anteflexion. This may be due to the altered direction of the cervix in case of cervical anteflexion, to the obstruction in the 123 cervical canal that interferes with the ingress of spermatozoa, to the generally undeveloped condition of the genital organs, or to the inflammation of the mucous membrane of the cervix and the body of the uterus.
The diagnosis of anteflexion is easily made. The character, position, and time of onset of the pain indicate some obstruction to the escape of menstrual blood. Vaginal examination reveals the sharp angle of flexion at the junction of the body and neck of the uterus.
Treatment.—If in a case of anteflexion pregnancy does occur and runs a normal course the disease will be cured. After labor the uterus does not return to the infantile shape and size. The stimulus of pregnancy brings about full permanent development of that organ. Miscarriage, however, is very apt to occur during the early months of pregnancy, especially in cases of long standing.
Various methods of treatment have been introduced for the cure of anteflexion. The object of all these methods is the straightening and enlargement of the cervical canal. Slow dilatation by graduated bougies has been successfully employed. Gradual straightening of the canal by the introduction of the uterine sound with increasing angle of flexion will also cure some cases, if seen early.
The use of the stem pessary (Fig. 83), which is worn continuously in the cervical canal, is dangerous and should not be practised.
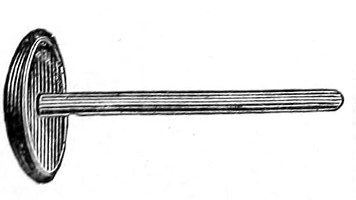
Fig. 83.—Stem pessary.
The best method of treatment consists in rapid forcible dilatation with the uterine dilator. Various instruments have been made for this purpose. The principle of all is the same. Two blades are introduced, in contact, in the cervical canal, and are then separated. Two of these instruments should be on hand—a small and a large dilator. The Goodell dilator (Figs. 84, 85) is so made that the 124 blades open parallel with one another, so that the whole of the cervical canal is uniformly stretched.

Fig. 84.—Goodell’s small uterine dilator. |
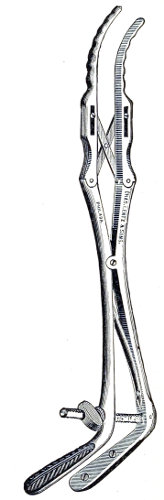
Fig. 85.—Goodell’s large uterine dilator. |
The best time to perform forcible dilatation is about one week after a menstrual period. The woman should be etherized and placed in the dorso-sacral position. The vagina should be sterilized. All aseptic precautions which one would follow in any gynecological operation should be observed here. There is always danger of producing septic inflammation of the endometrium. The cervix should be exposed through the Sims speculum, and the 125 anterior lip should be seized with the double tenaculum. Downward traction on the cervix straightens the cervical canal and renders easier the introduction of the dilator. The smaller dilator should first be introduced. No force should be used in passing it through the cervical canal. If an obstruction which cannot be gently overcome is met, the dilator should be introduced as far as the obstruction and the blades should then be separated. Slight dilatation of this kind below the angle of flexion will usually enable the operator to pass the instrument through the cervical canal at a subsequent attempt. After the smaller instrument has been introduced to the full extent the blades should be gradually separated, for a half inch or more, until the canal becomes large and straight enough to admit the large instrument. It should always be remembered that no force should be used in the introduction of either instrument. After introduction the blades of the large dilator should be slowly separated. On the handles of the Goodell instrument is a graduated scale showing the extent of the dilatation. In no case should the dilatation be carried beyond one and a half inches. In women in whom the cervix and uterus are small an inch of dilatation is sufficient. The maximum dilatation should be reached slowly and gradually. Laceration of the cervix or of the margin of the external os should be avoided. Sometimes ten or fifteen minutes are required before full dilatation is attained. When this point is reached the handles should be held in place by the screw, and the instrument should be kept in the uterus for ten or fifteen minutes longer. The longer the dilatation, the more permanent will be the result.
After the instrument is withdrawn the cervical canal and the vagina should be washed out with a 1:2000 solution of bichloride of mercury, and a light gauze pack should be introduced into the vagina. The pack should be removed at the end of forty-eight hours, and a daily douche of 1:4000 bichloride solution should be administered for the following week. The patient should remain 126 in bed for two weeks, or longer if there is any pelvic pain. Pain, however, does not follow this operation if we avoid operating upon those cases in which there is inflammatory disease of the tubes and ovaries. The too early resumption of the erect position may cause the failure of the operation. The abdominal pressure exerted upon the fundus uteri, before the organ has become fixed in its altered shape, may bring about a recurrence of the anteflexion. In case the external os be very small—too small to admit the dilators—it may be incised by small crucial incisions or reamed out with the closed blades of the scissors.
Dilatation of this kind usually produces a permanent broadening and shortening of the cervix. The cervical canal is rendered straighter and larger.
The good effects of the operation are not always apparent at the menstrual period immediately following the operation, because the results of the traumatism to the mucous membrane and the structures of the cervix are still present. At the periods after this, however, the dysmenorrhea is absent or is very much relieved. The benefit usually derived from this operation is a strong proof of the truth of the obstructive theory of the dysmenorrhea. If, after dilatation, conception takes place, the woman may look forward to perfect cure. In some cases the dilatation does not seem to be sufficient to produce a permanent open condition of the cervical canal, and the signs of obstruction (dysmenorrhea) return. In such a case the dilatation should be repeated. The more thoroughly the dilatation is performed the first time the less often will the second operation be necessary. 127
Retroversion of the uterus means a turning back or a backward rotation of that organ. The shape of the uterus may not be altered. The fundus, instead of lying forward upon the bladder, is directed backward, and sometimes lies in the hollow of the sacrum (Fig. 86).
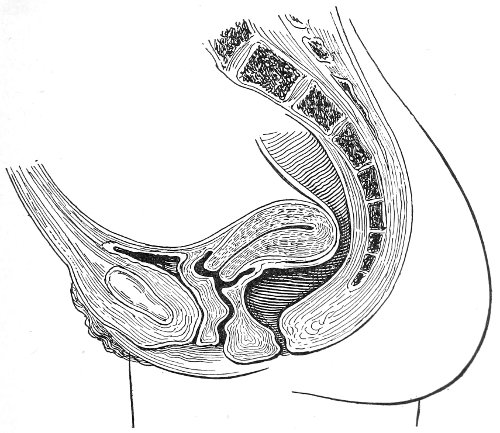
Fig. 86.—Retroversion of the uterus.
Retroflexion means a bending backward of the uterine axis. The axis of the body of the uterus is normally inclined forward at an obtuse angle with the axis of the cervix. When the axis of the body of the uterus is inclined 128 backward at an angle with the axis of the cervix, retroflexion exists. Retroflexion may vary in extent from an angle very little less than 180 degrees to an angle considerably less than 90 degrees (Fig. 87).
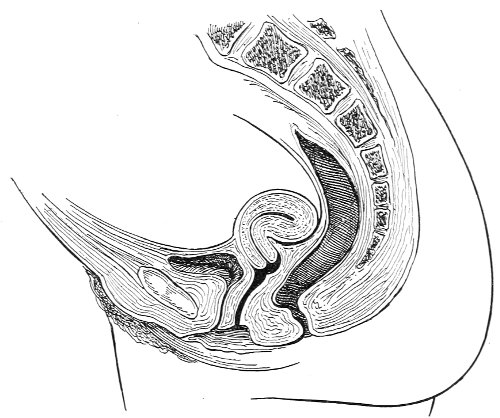
Fig. 87.—Retroflexion of the uterus.
Retroflexion and retroversion usually coexist. The conditions are due to similar causes. They may originate simultaneously, or one condition, occurring primarily, may induce the other.
An infinite number of degrees of retroversion may exist. For convenience of clinical description three degrees have been described. In the first degree the fundus uteri is directed upward approximately toward the promontory of the sacrum. In the second degree the uterus lies transversely across the pelvis, the fundus and the cervix being at about the same level. In the third degree the retroversion is extreme, and the fundus lies below the level of the cervix (Fig. 88).
Retroversion of the uterus is progressive. It usually proceeds from bad to worse. As soon as the downward 129 abdominal pressure begins to act upon the anterior face of the uterus there is a continuous force increasing the retroversion.
There are many causes of retroversion and retroflexion.
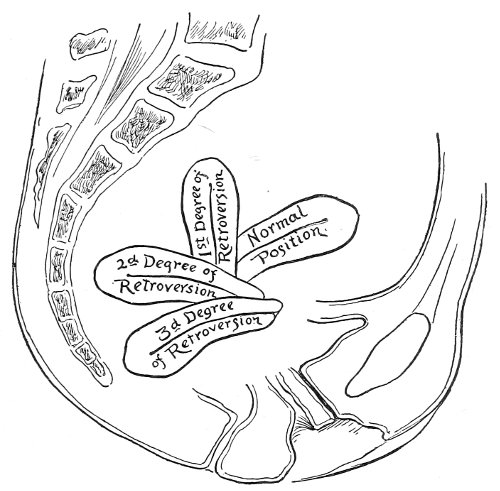
Fig. 88.—Diagram of the degrees of retroversion of the uterus.
The disease may be congenital. Extreme retroflexion has been found in the uterus of the new-born infant. Congenital retroversion and retroflexion may be due to imperfect development, and resulting imperfect invagination of the cervix. The condition may also be caused by arrest of development of the posterior wall of the uterus; the anterior wall thus outgrowing the posterior.
Many cases of retroversion undoubtedly originate during girlhood as a result of falls, blows, distortion of the body, or sudden efforts at lifting. The origin of the symptoms may be traced in many cases directly to some such cause.
The uterus may be considered to be balanced upon an axis running transversely. Anything that turns the uterus backward, so that the intra-abdominal pressure may act upon the anterior wall, will produce retroversion. 130 It is probable that an over-distended bladder occasionally acts as a cause of retroversion.
Retroversion is not at all rare in single women. It is very often discovered soon after the establishment of the menstrual function, the symptoms of the retroversion, which probably occurred during girlhood, first appearing at this time. Retroflexion, on the other hand, except to the slight extent caused by the retroversion, is unusual in single women.
Parturition is probably the most frequent cause of retroversion and retroflexion of the uterus. If the woman leaves her bed or goes to work too soon after miscarriage or labor, many conditions are present that favor retrodisplacement of the uterus. The uterus is larger and heavier than normal, as a result of imperfect involution: the uterine ligaments are lax; the vagina and the vaginal orifice are relaxed, and the support of the pelvic floor is consequently deficient; the abdominal walls are relaxed and the retentive power of the abdomen is diminished. It will be remembered that these are the causes that favor prolapse of the uterus; in fact, a slight degree of uterine prolapse usually accompanies such cases of retrodisplacement. A certain amount of retroversion must always exist before the uterus can pass along the vagina. It must turn backward, so that its axis becomes parallel to the axis of the vagina.
Retroflexion occurring after miscarriage or labor is sometimes the result of unequal involution in the uterine walls. If the involution takes place more completely in the posterior than in the anterior wall of the uterus, a bending back, or a retroflexion, will occur. Such inequality of involution may result from inflammation about the site of the placenta.
Retroflexion is a disease of the parous woman, as anteflexion is a disease of the single and the sterile woman.
Retroversion may be a direct result of laceration of the perineum. When the pelvic floor is destroyed and the posterior vaginal wall begins to prolapse, it drags 131 upon the posterior wall of the cervix, and may in this way turn the uterus backward.
Retroversion also results from traction of inflammatory adhesions in the pelvis. Cases of chronic inflammation of the Fallopian tubes accompanied by inflammation of the pelvic peritoneum present adhesions between the posterior wall of the uterus and the hollow of the sacrum; these adhesions drag the uterus backward (Fig. 89).
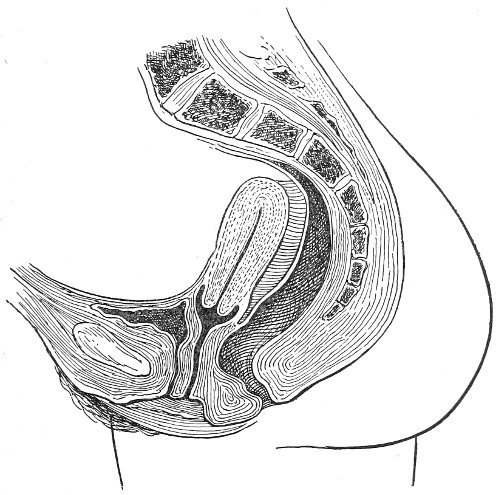
Fig. 89.—Retroversion of the uterus, with adhesions binding it to the anterior wall of the rectum and the hollow of the sacrum.
In cases of retroversion and retroflexion of the uterus serious derangement of the circulation results. A state of passive congestion follows interference with the venous supply. This congestion produces some enlargement of the uterus and chronic congestion or inflammation of the endometrium. Consequently, in all old cases of retrodisplacement endometritis is an accompaniment. 132
Retroversion of the uterus causes traction on the vesico-uterine connection, and the neck of the bladder is dragged upon; for this reason irritability of the bladder, characterized by frequent and perhaps painful micturition, is often present in cases of retroversion. It is not uncommon to see women who have received treatment directed to the bladder for conditions of this kind that disappear immediately when the uterus is restored to the normal position.
The pressure of the displaced fundus upon the rectum may also give trouble. Women in this condition often complain of a feeling of obstruction in the rectum. Pressure upon the hemorrhoidal veins results in hemorrhoids.
There usually accompanies retroversions of the uterus a backward and downward displacement of the ovaries—in other words, a prolapse of the ovaries.
The symptoms of retrodisplacement are numerous, and may be referred directly to the altered position of the uterus and the accompanying conditions. There are backache situated in the upper part of the sacrum, and headache situated on the top of the head or in the occiput. These may be considered the two constant symptoms. There is a feeling of weight and dragging in the pelvis, extending down the thighs. Physical weakness, or inability to walk or stand for more than a short time, is often very marked, and seems to be out of all proportion to the lesion of the uterus. The manner in which such weakness of the legs is produced is not very evident. That it is caused directly by the displacement of the uterus, however, is proved by the fact that it disappears as soon as the uterus is restored to its normal position.
The accompanying prolapse of the ovaries produces symptoms referable to these organs, the chief symptom being pain in each ovarian region.
The irritability of the bladder has already been spoken of. Menorrhagia and leucorrhea may be present as a result 133 of the congestion and the chronic inflammation of the endometrium. Menstruation is usually painful. At the menstrual period the backache, headache, ovarian pain, and vesical disturbance are increased. Dysmenorrhea due to obstruction is unusual in cases of retroflexion. Retroflexion usually occurs in parous women, in whom the cervical canal is large, and the flexion therefore does not cause sufficient obstruction to impede the escape of menstrual blood. All the symptoms arising from retroversion of the uterus are ameliorated by the recumbent posture.
The diagnosis of retroversion and retroflexion of the uterus is very easily made by bimanual examination. The abdominal hand fails to find the fundus in the normal position. The vaginal finger feels the cervix uteri directed not backward toward the coccyx, but forward in the direction of the vaginal axis or toward the symphysis pubis. The posterior wall of the cervix and the body of the uterus may be plainly felt inclined backward. In case of retroflexion the angle of flexion may be felt by the vaginal finger.
The accompanying prolapse of the ovaries is usually very easily demonstrated by vaginal touch.
Treatment.—As retroflexion does not usually cause obstruction of the menstrual flow, the treatment need not be directed toward rendering patulous the cervical canal, as in the case of anteflexion. Retroflexion is always associated with retroversion, and the methods that correct the retroversion place the uterus in such a position that the intra-abdominal pressure acts on the posterior face of the uterus and gradually reduces the flexion. Therefore the treatment of retroflexion and of retroversion may be considered together.
Retroversion is treated by the vaginal pessary and by operation.
The vaginal pessary is an instrument to be worn in the vagina, and designed to retain the uterus in its normal position. A great many different kinds of pessaries have 134 been invented. The large number of different-shaped instruments proves the inefficacy of the pessary as a means of treatment in many cases of retroversion.
The best pessaries for retroversion are the Hodge (Fig. 90, A), the Smith (Fig. 90, B), and the Thomas (Fig. 90, C). These instruments are made of hard rubber. They consist of an upper and a lower transverse bar joined by two lateral bars. They are so shaped that when introduced into the vagina they correspond very closely to the curvature of the vaginal slit.
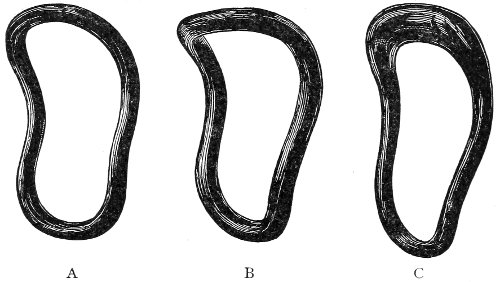
Fig. 90.—Pessaries for retroversion: A, Hodge pessary; B, Smith pessary; C, Thomas pessary.
Fig. 91 shows a side view of a pessary in position, and it will be observed that the curves of the instrument are closely adapted to the curves of the posterior vaginal wall, upon which it lies.
The vaginal pessary retains the uterus in place by raising the posterior vaginal fornix and keeping tense the posterior vaginal wall. It will be observed that the posterior wall of the vagina runs over the upper transverse bar of the pessary like a rope over a pulley; therefore there is maintained a continuous traction in an upward and backward direction upon the cervix, and a resulting continuous tendency to throw the fundus uteri in a forward position (Fig. 91). The tension of the posterior 135 vaginal wall and the traction upon the cervix vary with the position and occupation of the woman, and are increased by anything that increases the intra-abdominal pressure.
The vaginal pessary does not maintain the uterus in place by pressure upon the body of the uterus, nor does the vaginal pessary correct a retrodisplacement. The uterus should be restored to its normal position as nearly as possible before the pessary is introduced.
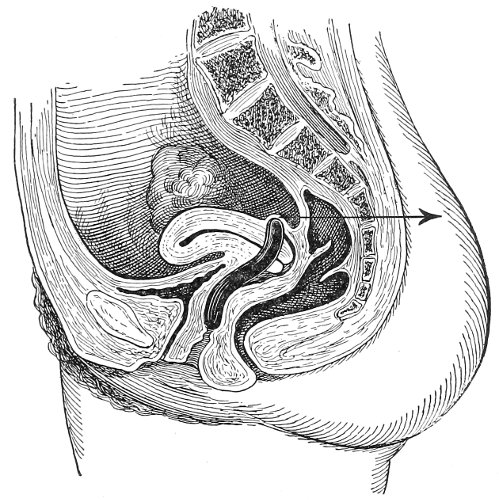
Fig. 91.—The retroversion pessary in position. The arrow shows the direction of the traction of the posterior vaginal wall upon the cervix.
Replacement of the uterus may be effected in one of two ways: by bimanual reposition while the woman is in the dorsal position; or by instrumental reposition while the woman is in the knee-chest position.
In bimanual reposition the uterus is manipulated between the vaginal finger or fingers and the abdominal hand until the organ is brought to its normal position of anteversion (Fig. 92). Sometimes this may be more easily accomplished by introducing one or two fingers into the rectum.
After bimanual reposition the pessary should be introduced 136 in the vagina, and the upper bar of the instrument should be carried behind the cervix by manipulation with the vaginal finger.
Bimanual reposition is often difficult or impossible in fat women and in those with rigid abdominal walls.
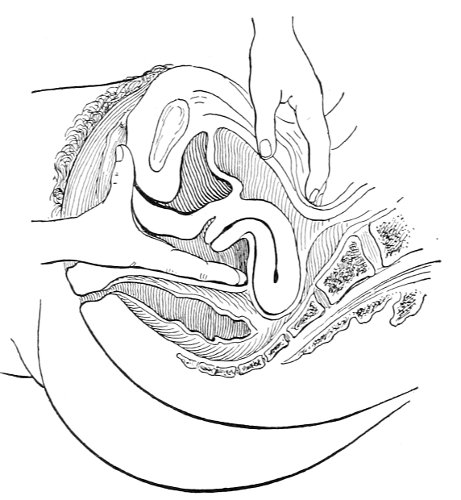
Fig. 92.—Bimanual reposition of the retroflexed uterus.
Instrumental reposition in the knee-chest position, however, is applicable to all cases in which a pessary is indicated. As this method is the one that should in general be followed, it will be described in detail.

Fig. 93.—Uterine repositor.
The woman should be placed in the knee-chest position. The perineum should be retracted and the cervix exposed with a Sims speculum. It will be observed that the cervix is directed forward toward the symphysis pubis. The uterine repositor (Fig. 93) is then introduced, and pressure is made in the posterior vaginal 137 fornix upon the displaced fundus. The fundus may be felt with the repositor in this position. Sometimes, by grasping the cervix with a tenaculum and drawing it downward, the repositor may be applied with better effect (Fig. 94). It will often be observed that under this pressure the fundus immediately drops forward, while the cervix is turned backward through an angle of 90° or perhaps 180°, so that the external os looks no longer toward the symphysis pubis, but toward the hollow of the sacrum. The direction of the cervix shows plainly when the uterus is in the normal position. Instead of the uterine repositor we may use a small firm ball of cotton held in long forceps.
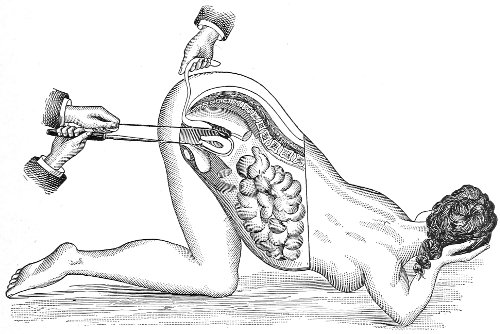
Fig. 94.—Replacement of retrodisplaced uterus by means of the uterine repositor, with patient in the knee-chest position (Baldy).
Sometimes it is not possible to make the entire correction of the displacement at one time. The uterus may perhaps be reduced from retroversion of the third degree to that of the first degree, and at a subsequent attempt it may be reduced still more, until finally it is brought to its normal position. In some cases the difficulty of producing complete reduction at one time is due to the fact 138 that the woman is unaccustomed to the position and the manipulations, and is constantly straining and involuntarily resisting. Complete relaxation of the abdominal walls is necessary.
If the uterus can be reduced to the normal position, the pessary may be immediately introduced. If the reduction is not complete, it is best to pack the vagina with cotton to maintain the degree of reduction that has been attained, and to repeat the attempt the next day, continuing in this way until the uterus has been brought approximately to its normal position, when the pessary should be introduced. The cotton should be packed into the vagina in the form of balls or pledgets about one and a half inches in diameter, which should be introduced with the forceps (Fig. 95) and carefully and tightly packed into the posterior vaginal fornix. Other pieces should then be packed against the anterior aspect of the cervix, and then the rest of the vagina should be rather loosely filled.
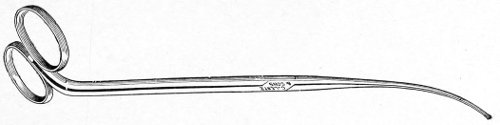
Fig. 95.—Uterine forceps.
The pessary should be introduced with the woman in the knee-chest position. A number of pessaries, of various sizes and shapes, should be at hand, in order to have a suitable assortment for choice. The pessary must be of the proper length, breadth, and shape; these requirements differ in various cases. The length of the pessary should be such that when the upper transverse bar lies in the posterior vaginal fornix the lower transverse bar is over the position of the internal urinary meatus. The course of the urethra is marked by small transverse folds of mucous membrane 139 on the middle of the anterior vaginal wall, and the internal urinary meatus is situated approximately where these small transverse folds cease and become merged into the larger oblique folds of the vaginal walls. This distance may be measured upon the uterine repositor or it may be estimated with the eye.
It should be remembered that all the dimensions of the vagina are exaggerated in the knee-chest position, as the vaginal canal is distended by atmospheric pressure. The width of the pessary should be such that there is no lateral tension put upon the vaginal walls.
The curvature of the pessary should be such that the upper transverse bar does not press upon the posterior aspect of the cervix, but is so placed that the posterior vaginal fornix is drawn upward and backward.
The curvature of the pessary may be altered to suit any case by dipping the instrument in oil and gently heating it over the flame of a spirit-lamp. In this way the rubber is softened and may be pressed into any shape. While soft and under pressure it should be plunged into cold water to set it in the altered form.
The pessary may be introduced while the perineum is retracted with the speculum; or it may be passed into the vagina first, the speculum then being introduced and the pessary moved into the proper position. The pessary should be greased, the lower transverse bar should be grasped with the thumb and the index finger, and the instrument should be introduced in such a direction that one lateral bar lies in the vaginal sulcus. The upper transverse bar may readily be placed behind the cervix, by manipulation with the finger or the forceps, when the perineum is retracted with the speculum.
The speculum should be removed, and the woman should assume the Sims posture for a few minutes. She may then get up from the table, and the examination may be made in the erect posture, for in this position, better than in any other, the fit and the action of the pessary may be determined. It will be found that the 140 lower bar of the pessary is in relation with the anterior vaginal wall at the position of the internal urinary meatus. It should not protrude from the ostium vaginæ. It should be possible to pass the finger readily between the vaginal walls and the lateral and lower bars of the pessary. The cervix should be felt directed backward through the upper portion of the ring of the pessary. It will be felt that the pessary is retained in the vagina not by any pressure against the vaginal walls, but by a suction—in other words, by the retentive power of the abdomen.
A vaginal douche of warm water should be administered once a day while the pessary is worn.
The woman should be directed to return for examination three days after the introduction of the pessary, or sooner if any discomfort is experienced. Sometimes the uterus becomes retroverted while the pessary is in position, and becomes flexed over the upper bar of the instrument, considerable pain resulting. In other cases, where the vagina is patulous and too small an instrument is used, the pessary becomes turned so that the long axis lies transversely. It is well to advise the woman to remove the instrument herself if it makes her very uncomfortable.
The pessary should be examined digitally in the dorsal or the erect position, or visually in the knee-chest position. If it is found that the retroversion has returned, the uterus should be replaced and a pessary better suited in size and shape should be introduced. It is always desirable to use as small an instrument as practicable. The intervals between examinations may be gradually lengthened to two weeks or a month. A woman using a pessary should always be under the supervision of a physician. The retroversion pessary does not interfere with sexual connection.
The bowels should be carefully regulated. The clothing should be supported from the shoulders, not from the waist, and heavy lifting should be avoided as much as possible. 141
After a woman has worn a pessary for three or four months, and it is found that the uterus remains in the normal position, the instrument should be removed and the result carefully watched.
If the uterus continues in its normal position of anteversion, a cure has been accomplished and the pessary may be discarded. If the retroversion returns, as it very often does, the pessary should be introduced again, and an unfavorable prognosis of cure by this means should be made. The patient must then choose between the use of the pessary for an indefinite period, under medical supervision, and cure by means of an operation.
The Smith pessary is better adapted to the shape of the vagina, which normally narrows from above downward, than is the Hodge instrument. The Thomas pessary, in which the upper bar is made very broad, is applicable to cases of sharp retroflexion with retroversion, in which the upper bar may become fixed in the angle of flexion in case the retroversion returns. The upper bar is made so broad that the angle of flexion would be spanned by it in case of such an accident.
The action of the pessary depends upon the integrity of the vagina and the pelvic floor. The retroversion pessary, therefore, cannot be used when there is a laceration of the perineum. In such a case the perineum must always be closed as a preliminary step.
The pessary should not be used when there is a laceration of the cervix uteri, for traction upon the posterior lip of the cervix increases the eversion.
The pessary is contraindicated in all cases in which there are pelvic adhesions restraining the uterus, in those cases in which there is inflammatory disease of the Fallopian tubes, and in cases where there is prolapse of the ovary, which may be pressed upon by the upper bar of the pessary.
Before making any attempt to replace a displaced uterus the physician should always make a careful bimanual examination to determine the existence of any 142 acute or chronic inflammation of the Fallopian tubes or the ovaries. Such inflammation is a contraindication to the use of the pessary and to any of the manipulations for replacement of the uterus that have already been described.
If the uterus is adherent, the pessary should not be used. Cure of the retroversion by it is practically impossible, and operative treatment is safer and more certain.
Operative Means of Treating Retrodisplacement of the Uterus.—A great many kinds of operation have been introduced for curing retrodisplacement of the uterus. The fundus has been attached to the anterior abdominal wall by passing a needle and a suture into the uterus and thrusting it through the uterine wall and the anterior abdominal wall; the uterine cornua have been sutured to the anterior parietes; the round ligaments have been shortened by folding each upon itself, and fixed in this position by suture; the round ligaments have been drawn back through openings made in the broad ligaments and attached by suture to each other and to the posterior surface of the uterus; the utero-sacral ligaments have been shortened; the uterus has been held forward by sutures applied through the anterior vaginal fornix.
The two operations that have deservedly met with the greatest favor are ventro-suspension of the uterus, in which the abdomen is opened and the fundus is sutured directly to the anterior abdominal wall, and Alexander’s operation, in which the uterine displacement is corrected by shortening the round ligaments as they emerge from the inguinal rings. The latter operation is designed to be extra-peritoneal. The following is the method of performing Alexander’s operation:
The uterus should first be replaced as already described, and held in position by a gauze or cotton pack. A two-inch incision is made from the pubic spine in the direction of the inguinal canal. The external inguinal ring is opened without wounding the pillars. The thin layer of fascia over the ring is divided, the fat is separated, and the round ligament is sought with a blunt hook. If 143 the ligament is not found here, the canal may be opened to the internal ring. When one ligament has been found, it is secured with forceps and the wound is protected while the other ligament is secured in a similar way. The ligaments are then gently drawn out until they become tense. If the inguinal canal has been opened, it should be repaired by a catgut suture.
The ligament should be sutured to the pillars of the ring by two or three sutures. The excess of the ligament, sometimes amounting to two or three inches, should be cut off. The incision should then be closed.
The field of this operation is very limited. It is not applicable when there are adhesions nor when there is disease of the tubes or ovaries requiring operative treatment.
Many of the cases of retroversion of the uterus that require operative treatment are complicated by salpingitis and pelvic adhesions, though these extra-uterine conditions are very often not recognized by bimanual examination before the abdomen is opened.
The operation that at present seems to possess most advantages for the cure of those cases of retroversion of the uterus that cannot be cured by the pessary is the operation of ventro-suspension of the uterus (Fig. 96). It is performed as follows:
An incision, one and a half to three inches in length, is made in the median line of the anterior abdominal wall, immediately above the pubis. Two fingers are introduced into the abdominal cavity, and the fundus uteri is lifted forward. The plane of the abdominal incision is exposed, and a curved needle carrying a medium-sized silk suture is passed through a few fibers of the rectus muscle and the peritoneum on one side, immediately above the lower angle of the incision. The needle is then passed through the tissue of the fundus uteri on the line joining the uterine cornua or a little posterior to this line. The amount of uterine tissue included in the suture is about one-quarter of an inch broad and one-eighth to one-quarter of an inch deep. The needle is 144 then passed through the peritoneum and a few fibers of the rectus muscle on the side of the abdominal incision opposite the point of entrance. The fascia of the rectus should not be included. A similar suture is passed about one-third of an inch above this, traversing the uterine wall on a line about one-third of an inch posterior to the first suture. While the fundus is held forward by the finger of an assistant these sutures are tied, so that the fundus uteri is brought into contact with the anterior abdominal wall. The ends of the sutures are cut short. The abdominal incision is then closed by three layers of sutures—silk for the peritoneum, catgut for the muscle and fascia, and the intra-cutaneous suture for the skin. Accompanying disease of the tubes and ovaries may be treated directly by this operation, and any adhesions may readily be broken.
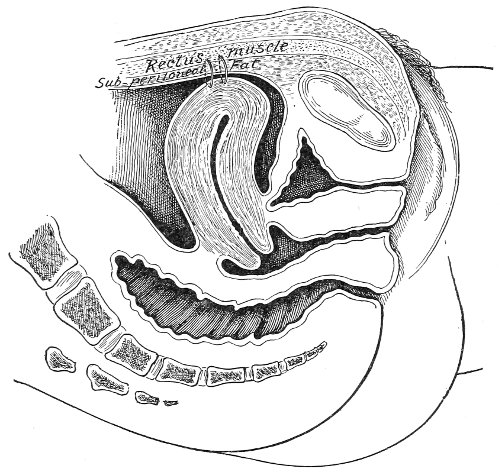
Fig. 96.—Position of the sutures in ventro-suspension of the uterus.
In performing this operation it should be remembered that we do not wish to make a fixation of the uterus to 145 the anterior abdominal wall. The inclusion of a broad mass of uterine tissue in the suture, and scarification of the anterior face of the uterus, which is sometimes practised, may result in a broad, unyielding adhesion which will interfere with the normal mobility of the uterus and with the course of pregnancy and labor.
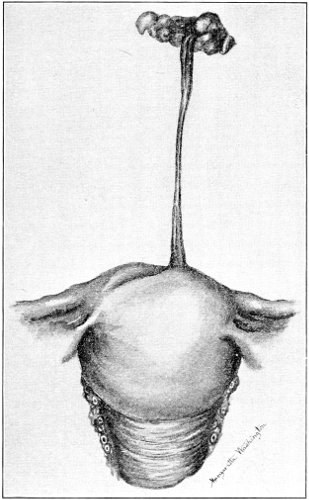
Fig. 97.—The suspensory ligament two years after the operation of ventro-suspension. The ligament measured three inches in length.
After this operation of ventro-suspension the fundus uteri does not remain permanently in contact with the anterior abdominal wall. In time it drops somewhat backward and downward. The silk sutures drag out a ribbon-shaped fold of tissue consisting of peritoneum and a little muscle-fiber from the anterior abdominal wall, 146 and a similar fold of peritoneum and perhaps some muscular fibers from the uterus, so that in time the uterus becomes attached by a slight pliable ligament from one to three inches in length (Fig. 97). Bimanual examination of the uterus one year after this operation shows that the uterus has about the normal range of mobility. If this operation is properly performed, the course of subsequent pregnancies and labors seems to be in no way impeded.
The operation of ventro-suspension should always be accompanied by perineorrhaphy in case there has been laceration of the perineum. The two operations may be done at the same time.
The treatment of retrodisplacement of the uterus may be briefly summarized as follows:
The cases of retrodisplacement of the uterus suitable for treatment by the pessary are those in which there are no adhesions and in which there is no disease of the Fallopian tubes or the ovaries. If a prolapsed ovary returns to its normal position when the displacement of the uterus is corrected, it will of course not be pressed upon by the bar of the pessary. But in some cases the ovarian prolapse continues even though the uterus is in its normal position, and under such circumstances a pessary usually cannot be tolerated.
The cases that offer the best prospect of cure by the pessary are those cases of retroversion, occurring as the result of labor, in which the perineum is intact, and which are seen within one or two years after the occurrence of the lesion. The prognosis becomes more unfavorable the longer the condition has existed before treatment.
Cases of congenital retroversion, or those occurring in young unmarried women, are very difficult to cure with the pessary. This instrument should always be tried for a few months, however, before operative measures are advised. In such cases the uterus has been so long in an abnormal position that its natural supports have become 147 permanently altered, and some continuous additional aid is necessary to maintain the normal position.
Every woman who uses a pessary should be under the supervision of a physician, and for this reason it is often most advisable to recommend immediate operation to poor women as the quickest and surest method of cure.
Immediate operation should always be advised in all cases of retroversion with adhesion or with disease of the tubes and ovaries.
It should not be forgotten that we occasionally see women with retroversion of the uterus who present no symptoms whatever referable to this lesion. In such cases no treatment is required.
Note (in fourth edition).—The operation of ventro-suspension as described above has been done by the writer and his assistants 310 times during the past seven years, 1893-1901. Two hundred and eleven of these women have recently made written reports of their condition, which are tabulated as follows:
Legend: A Number of cases relieved of the symptoms for which treatment was sought. B Number of cases improved C Number of cases not improved D Number of cases who became pregnant and went to full term E Number of cases who miscarried.
A B C D E Ventro-suspension with unilateral salpingo-oöphorectomy. 20 7 7 1 0 Ventro-suspension with perineorrhaphy and trachelorrhaphy. 34 15 5 6 3 Ventro-suspension with perineorrhaphy. 22 12 8 4 1 Ventro-suspension with trachelorrhaphy. 20 6 5 4 4 Ventro-suspension alone. 35 9 6 5 0 131 49 31 20 8 Of the 20 women who became pregnant and went to full term, the course of pregnancy was normal, and the children were all born alive. One woman had a prolonged and difficult labor, though forceps were not used. In 1 case forceps were used to deliver a ten-pound child, who presented in occipito-posterior position; in the remaining 18 cases labor was normal.
The operation of ventro-suspension seems to have had nothing whatever to do with producing the miscarriages. In fact, the number of miscarriages is small for any series of 211 women, most of whom were of the dispensary class.
Note.—Since collecting the statistics in the preceding note, we have continued to perform this operation in all cases of retroversion suitable for operation, with equally satisfactory results.
148
Laceration of the neck of the uterus is of very frequent occurrence. It is said that nearly every woman suffers with a laceration of greater or less extent at her first labor. The majority of such lacerations, however, undoubtedly heal during the puerperium and give no subsequent trouble. The lacerations that concern the gynecologist are those that persist, remaining ununited after the woman leaves her bed. The description of the injured parts and the treatment therefor will be applicable to such old cases of laceration. It is true that some gynecologists have advised immediate examination and the primary operation for repair in case of laceration of the cervix, as in case of injury to the perineum; but such a course has at present but little endorsement. It is difficult to obtain a satisfactory examination under such circumstances. A digital examination alone, unless the sense of touch be very acute, would often fail to detect the lesion in the soft cervical tissue. The woman is exposed to the danger of infection of the upper genital tract from the manipulations of the examination and the operation, and such exposure may be unnecessary, because there is no doubt that many lacerations of the cervix unite of themselves.
It has been found necessary to perform the operation immediately after labor on account of severe hemorrhage from the lacerated wound.
Laceration of the cervix may take place in any direction, and the injury is described according to the direction and number of the tears. A lateral laceration takes 149 place on either side of the cervix. A bilateral laceration involves both sides (Fig. 104, A). The left is the more usual lateral laceration (Fig. 98), and in case of a bilateral tear the injury on the left side is usually the more extensive. The stellate laceration (Fig. 99) occurs when three or more lacerations radiate from the cervical canal. The less common varieties of laceration seen by the gynecologist are through the anterior and through the posterior lip. It may be that such lacerations occur as often as the lateral lacerations, and that spontaneous repair more often occurs, so that they produce no subsequent trouble. The relations of the neck of the uterus are such that accurate apposition of the injured parts is more likely to occur in case of antero-posterior laceration than in the lateral form of the injury. In some cases there seems to be no doubt that the laceration has extended through the posterior lip of the cervix into the cellular tissue above the posterior vaginal fornix, and that spontaneous repair has taken place, leaving a dense band of scar-tissue to mark the site of the lesion.
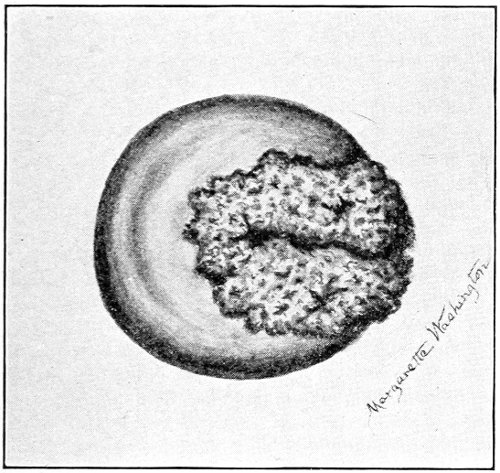
Fig. 98.—Left lateral laceration of the cervix with erosion.
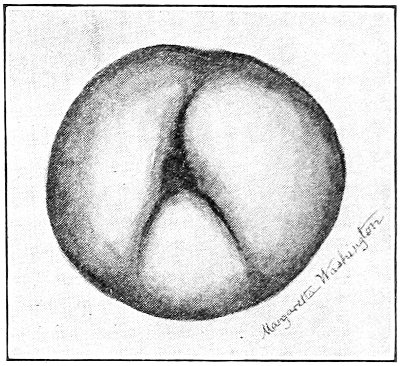
Fig. 99.—Stellate laceration of the cervix.
An incomplete laceration of the cervix is sometimes found. In this injury the tear has extended but part way through the wall of the cervix. The mucous membrane 150 of the cervical canal and the muscular wall of the cervix are lacerated, but the injury does not involve the mucous membrane of the vaginal aspect, beyond, perhaps, a slight splitting of the external os (Fig. 100). The lesion is thus concealed, and separation of the portions of the cervix is prevented. The injury may be detected by introducing a sound in the cervical canal and placing a finger on the vaginal aspect of the cervix, when it will be found that at this spot the point of the sound and the finger are separated only by the thickness of the vaginal mucous membrane, and not by the normal thickness of the wall of the cervix.
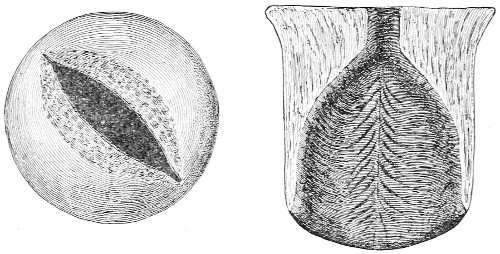
Fig. 100.—Incomplete laceration of the cervix.
The appearance of a lacerated cervix varies with the time that has elapsed since the receipt of the injury. A few weeks or months after the occurrence the torn portions of the cervix will be found, by sight or touch, lying in more or less close apposition, the general conical shape of the cervix being unaltered. After the lapse of a longer period, however, the edges of the laceration become rounded, and a certain amount of eversion, or turning out, of the portions of the cervix takes place, so that the mucous membrane of the cervical canal becomes exposed. This eversion is always most pronounced in the bilateral laceration, and is especially striking when the tear has extended entirely through the cervix into the lateral 151 vaginal fornices. In such cases the cervix assumes the shape of a split stalk of celery (Fig. 101). The cases of laceration with eversion of the lips are those in which the most marked symptoms are found. When eversion occurs, and the mucous membrane of the cervical canal is exposed, the shape and appearance of the cervix are very much altered from the normal. Before the true nature of this lesion had been pointed out by Emmet such a cervix was said to be ulcerated, the raw-looking surface, corresponding to the exposed, irritated, and inflamed mucous membrane of the cervical canal, having been mistaken for an ulcer. Even at the present day such a mistake is not infrequently made.
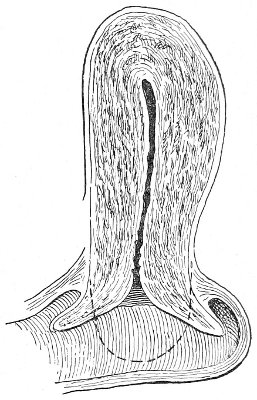
Fig. 101.-Bilateral laceration of the cervix with eversion. The dotted line shows the normal shape of the cervix.
Microscopical examination of such raw-looking surfaces shows that they are in no sense ulcers. “The surface is covered with a single layer of epithelium; the cells are smaller than those which line the normal cervical canal, and, being narrow and long, have a palisade-like arrangement; the thin layer of cells allows the subjacent vascular tissue to shine through, hence the redness of color. The surface is further thrown into numerous folds, producing glandular recesses and processes; these processes cause the granular appearance of the surface” (Hart and Barbour).
These red patches are larger than the surface of the everted mucous membrane of the cervical canal; they are continuous with, but extend beyond the limits of, this mucous membrane. It is said that this increase is occasioned 152 by proliferation of the epithelium that lines the cervical glands.
As a substitute for the misleading term “ulceration,” applied to this condition, there have been proposed the terms “erosion,” “ectropion,” or “eversion” of the mucous membrane, and “catarrhal patch.”
A true ulcerated surface is sometimes found on a lacerated cervix as a result of excessive irritation, but such a condition is rare.
As the laceration occurs in the cervix before involution has begun, this process is impeded, so that a state of subinvolution of the cervix results, and the part remains hypertrophied or much larger than normal.
The cervical glands share in this condition of subinvolution, retaining much of the increased size and activity that are normal in the pregnant state.
Changes due to chronic congestion and inflammation also take place. The connective tissue increases in amount, and the cervix becomes hard, indurated, or sclerotic.
The racemose glands, which open upon the cervical mucous membrane, become inflamed, and, as a result of change in the consistency of the glandular secretion or of obstruction of the gland-orifices, retention takes place, with the production of small cysts called Nabothian cysts. Such cysts often extend peripherally, so that the distal end of the occluded gland approaches the vaginal aspect of the cervix, and appears beneath the mucous membrane as a translucent vesicle about the size of a small pea. Puncture of such a vesicle permits the escape of a drop of gelatinous fluid.
The whole of the body of the cervix may be filled with innumerable cysts of this kind, of varying size. When projecting beneath the mucous membrane they feel like small shot imbedded in the cervix. A cervix in this condition is said to have undergone cystic degeneration. The inflammation of the lower exposed portion of the mucous membrane of the cervical canal extends upward, 153 so that a condition of general chronic cervical catarrh results. This exceedingly common disease is usually caused by laceration of the cervix.
The focus of continuous irritation in the cervix interferes with the normal involution of the body of the uterus, so that there occurs a condition of uterine subinvolution, which may be the cause of the chief symptoms with which the woman suffers. The endometrium shares in the subinvolution, and, as a consequence of this, and perhaps also from extension of inflammation from the cervical mucous membrane, various forms of endometritis may occur.
In some cases of laceration of the cervix no groove corresponding to the angle of the laceration can be felt or seen, because it has been filled with a plug or mass of cicatricial tissue. In such cases this plug of scar-tissue may be felt, distinguished by the palpating finger from the softer surrounding tissues of the cervix.
Symptoms.—The symptoms of laceration of the cervix uteri are usually referable to pathological conditions that are secondary to the laceration, and are in no way characteristic. Leucorrhea, or a discharge from the exposed and inflamed cervical mucous membrane, is usually present. Menstruation is often irregular, and is increased in duration and amount as a result of the subinvolution of the uterus and the chronic congestion, and perhaps inflammation, of the endometrium. Backache and vertical headache may also be present from the same cause.
If the tear is at all extensive—and especially if it extends through the cervix into the cellular tissue of the broad ligament—pelvic pain, referred to the general position of the scar, may be experienced.
Movement of the cervix or of the uterus that causes traction upon the scar in the broad ligament produces pain. Such pain may result from the bimanual examination, from jarring or movements of the body, from defecation, or from coitus.
Much of the pelvic pain with which women suffer in 154 laceration of the cervix is probably due to the pelvic lymphangitis and lymphadenitis that are caused by the continuous irritation of the diseased cervix.
Sterility is a not unusual accompaniment of laceration of the cervix. It may be due to the malposition of the external os or to the profuse cervical discharges. In case conception occurs, abortion may follow on account of the pathological condition of the body of the uterus and of the endometrium.
Sometimes very marked reflex nervous disturbances are caused by a laceration of the cervix. Such disturbances are most pronounced in those cases in which there is much cicatricial tissue, and in those in which the cervix is hard and sclerotic or cystic as a result of long-standing inflammation—in other words, in those cases in which the substance of the cervix is most affected.
Neuralgia may occur in any part of the body. It is usually situated in the pelvis, or it may extend to the groin and down the thigh. Reflex nausea and vomiting may result from this as from other lesions of the uterus. Cataleptic convulsions and neurasthenia may also result from an old laceration of the cervix. The pelvic focus of irritation is constantly wearing and exhausting nervous energy.
Diagnosis.—The diagnosis of laceration of the cervix is readily made by digital examination. The palpating finger feels the one or more angles of laceration. The cervix loses its normal dome-like shape and becomes broader and flatter. In those cases of bilateral laceration where the eversion of the lips of the cervix is so marked that the angles of laceration are obliterated—becoming, in fact, 180 degrees—or where the angles have become filled up by a plug of cicatricial tissue, the angles of the laceration, of course, cannot be felt. We may often, however, detect the presence of the plug of cicatricial tissue, which feels harder than the surrounding tissues of the cervix; and we can always determine the presence of the eversion which seems to have obscured the lesion. 155 As the finger is passed over the flattened presenting cervix it is found that the shape is not round, but oval, with the long axis antero-posterior. The finger passes around a corner or edge as it glides into the anterior or posterior vaginal fornix. This corner or edge is the extremity of the torn everted lip of the cervix. It corresponds approximately with the margin of the normal external os. The apparent external os, or the opening of the cervical canal, which occupies the center of the presenting cervix, is really a part of the cervical canal higher up than the normal os—a part of the canal that has been exposed by the laceration and separation of the lips. This fact should be remembered when the length of the uterus is measured by the sound. The measurement taken from the apparent external os is often half an inch, or even one inch, less than it would be if the cervix were restored. The degree of subinvolution of the uterus indicated by the measurement of the length is often, therefore, considerably greater than would be supposed after such imperfect measurement.
The presence of an erosion on the face of the cervix may also be determined by palpation. The eroded surface has a soft and somewhat velvety feeling, in contrast with the smooth surface of the normal vaginal cervix covered with squamous epithelium.
The cystic degeneration is readily detected by feeling the small shot-like cysts that cover the cervix; and the sclerotic condition is indicated by the increased hardness or induration, which is easily perceptible to the finger.
The most satisfactory visual examination of a lacerated cervix is made through the Sims speculum, with the woman in the Sims or the genu-pectoral position. The bivalve speculum, by separating the upper vaginal walls, often increases the eversion of the lips and masks the lesion.
The nature of the injury in cases of bilateral laceration with eversion may readily be proved in examining through the Sims speculum. If the anterior and posterior 156 lips of the cervix be seized with tenacula and then drawn together, it will be observed that the area of erosion disappears and the normal shape of the cervix is approximately restored.
Treatment.—All forms of laceration of the cervix in which there exist eversion, erosion, cystic degeneration, and sclerosis should be operated upon. A slight laceration in a young woman in the active childbearing period does not demand operative treatment if there are no symptoms referable to the laceration. In women approaching middle life (forty years of age) all lacerations of the cervix should be closed, whether or not they produce symptoms.
It should always be remembered that cancer is most likely to originate in a cervix that has been lacerated, and the woman should be protected against this danger.
The treatment of laceration of the cervix is operative. A definite mechanical injury has been inflicted, and the parts must be repaired by operation.
The operation for the repair of a lacerated cervix is called trachelorrhaphy. The operation consists in denuding or excising the tissues on the torn surfaces and bringing the freshened surfaces together with sutures.
The form of the operation for a bilateral laceration is shown in Fig. 104. The operation should preferably be performed immediately after a menstrual period.
The instruments necessary for the operation of trachelorrhaphy are two double tenacula, two single tenacula, tissue-forceps, needle-holder, shot-compressor, Sims’ speculum, needles, (Fig. 102), knife, and scissors, sharp-pointed and curved on the flat (Fig. 103). The needles should be spear-pointed and should be strong and sharp, as the cervical tissues through which they are passed are often very dense. The straight or the curved needle may be used.

Fig. 102.—Cervix-needles.
Silkworm gut, shotted, is an exceedingly good suture-material. 157
The woman should be placed either in the Sims or the dorso-sacral position. The vulva, vagina, and cervix should be thoroughly cleansed and rendered as aseptic as possible. The cervix should be exposed through the Sims speculum. The anterior and, if desirable, the posterior lip of the cervix should be seized with a double tenaculum and held by an assistant; or the lip may be transfixed by a silk ligature, with which the cervix may be held.
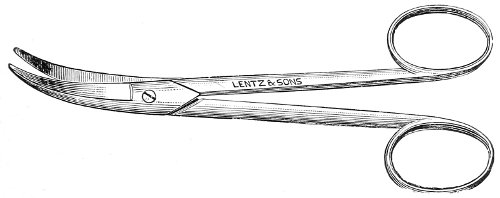
Fig. 103.—Curved scissors for performing trachelorrhaphy.
The denudation, which may be made with a knife or with scissors curved on the flat, should be begun upon the lower lip. The tissue to be removed may first be marked out with the knife. The tissue to either side of the old external os is seized with a tenaculum or with toothed tissue-forceps, and a strip is elevated by an incision extending into the angle of the tear. A corresponding opposite portion of tissue on the anterior lip is then seized in a similar manner, and a similar strip of tissue is excised, meeting and joining the strip first raised in the angle of the tear. We thus remove a wedge-shaped portion of tissue. The operation is then repeated upon the other side. The strip of mucous membrane that is left on the center of the lips to form the new cervical canal should be about a quarter of an inch in width.
If the finger be passed over the freshened surfaces, small indurated masses of tissue are sometimes felt. Such tissue should be caught with the tenaculum or the 158 forceps and excised. This condition is most usual when the tear has been of long standing and the cervix has undergone sclerotic changes. It is important that the excision of tissue should be carried well up in the angle of the laceration, in order that all hard cicatricial tissue may be excised.
The excision of tissue should be done as nearly as possible in the plane of the laceration. A frequent mistake is to remove too much tissue from the vaginal aspect of the cervix.
There is usually but little bleeding in the operation of trachelorrhaphy, and whatever bleeding there is may always be controlled by properly placed sutures.
The first suture should embrace the angle of the laceration. It should be introduced on the vaginal aspect of the cervix, near the edge of the mucous membrane, and should emerge on the edge of the mucous membrane of the cervical canal. It should then be reintroduced at a corresponding point on the opposite lip, and should emerge on the mucous membrane of the vaginal aspect. It is often difficult to bring the first suture out on the mucous membrane of the cervical canal. This, however, is not necessary if the suture embraces the whole of the denuded angle.
The other sutures, usually two or three in number, are introduced in a similar manner near the edge of the mucous membrane of the vaginal aspect, pass around the whole of the denuded surface, and emerge on the mucous membrane of the cervical canal, near the edge. They are then re-introduced on the opposite lip, and emerge at a corresponding point on the vaginal aspect of this lip.
A frequent mistake is to bring the sutures out on the raw surface so that the lateral union of the torn lips is shallow and superficial, often consisting only of the thickness of the mucous membrane of the vaginal aspect of the cervix. As the result of such an operation the new-formed cervical canal is spindle-shaped, much broader 159 160 than normal, and the condition of an incomplete laceration of the cervix results.
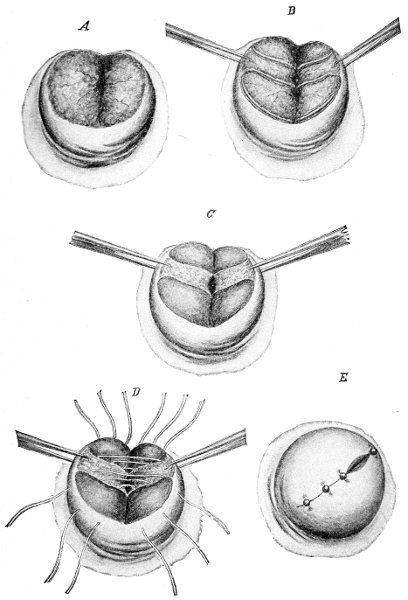
Fig. 104.—Steps of the operation of trachelorrhaphy for bilateral laceration of the cervix uteri: A, bilateral laceration with erosion; B, the area to be denuded has been marked out with the knife; C, the denudation has been accomplished; D, sutures introduced; E, completed operation.
After the operation the vagina should be washed out with a 1:2000 solution of bichloride; it should then be dried with sponge or gauze, and a light vaginal pack of sterile gauze should be introduced.
The gauze pack should be removed at the end of forty-eight hours, and after this a daily douche, with subsequent drying of the vagina, should be administered. The woman should remain in bed for two weeks. There is always present some subinvolution of the uterus, which is much benefited by rest in the recumbent position.
The sutures may be removed at any time after two weeks. To do this the woman should be placed in the lithotomy position. The perineum should be retracted with a Sims speculum, and the anterior vaginal wall should be supported by an elevator in the hand of an assistant.
If a perineorrhaphy is necessary, it should be performed at the same time as the trachelorrhaphy. In this case the cervix sutures should not be removed for three or four weeks, in order to avoid pressure upon the perineum by the retracting speculum.
If there is present marked subinvolution of the uterus with accompanying endometritis, the cervical canal should be slightly dilated and the body of the uterus should be thoroughly curetted immediately before performing the trachelorrhaphy.
If the operation of trachelorrhaphy is performed within a few months after the receipt of the laceration—before sclerotic, cystic, and erosion changes have appeared—there is usually required but little preparatory treatment. When, however, there is a marked and widespread erosion, and the cervix is full of numerous Nabothian cysts, or is hard and sclerotic from inflammatory exudate, it is necessary to devote from two to six weeks to preparation of the cervix for operation. Many failures in the operation of trachelorrhaphy are due to neglect of such preparatory 161 treatment. The hard, cystic cervix may unite but imperfectly after operation, or the symptoms referable to the diseased cervix may remain unrelieved by the operation. We often see women in whom laceration of the cervix has been closed with good union, and yet the sclerotic cystic condition of the cervix, and perhaps subinvolution of the uterus, persist, and symptoms continue as pronounced as before operation.
The preliminary or preparatory treatment consists of the administration of vaginal douches, regulation of the bowels by saline purgatives, and local applications to, and puncture of, the cervix uteri.
The woman should take, two or three times a day, a vaginal douche of one gallon of hot water (110° F.). The douche should be administered in the recumbent posture.
One or two watery fecal movements should be produced daily by Rochelle salts, sulphate of magnesium, or some similar preparation.
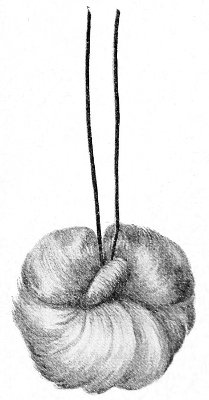
Fig. 105.—Cotton tampon.
Every five or six days the woman should be placed in the knee-chest position and the cervix should be exposed with the Sims speculum. The Nabothian cysts, which appear as translucent vesicles beneath the mucous membrane, should each be punctured with a sharp knife-point. If the cervix is much enlarged and congested, it should be freely punctured over the whole vaginal aspect to produce local depletion. Half an ounce or an ounce of blood may be removed in this way. The cervix should then be thoroughly dried, and an application of Churchill’s tincture of iodine should be made over the whole of the cervix and the vaginal 162 vault. The excess of iodine should be removed with a little cotton, and a cotton tampon (to which is attached a string) saturated with glycerin should be placed against the cervix (Fig. 105). The hygroscopic action of the glycerin is most useful in depleting the cervix. The woman should be told to remove the tampon by traction on the string at the end of twelve hours, and to follow the removal with a vaginal douche of hot water.
Such local treatment should be instituted immediately after a menstrual period and should be repeated every five or six days, and continued until the erosion and the cysts have disappeared and the induration has diminished. Three weeks of such treatment usually produce a very marked change. The cervix not only becomes much more healthy in appearance, but most of the symptoms of which the woman complained vanish. The leucorrhea diminishes or ceases; the backache and headache disappear. The relief is often so marked that the patient suggests the advisability of deferring operation. This, however, should never be countenanced, as all the symptoms will return with cessation of treatment.
If, after the careful administration of the treatment here prescribed for five or six weeks, the induration and cystic degeneration do not disappear, then the case is not one that will be benefited by trachelorrhaphy. The mere closure or union of the indurated and cystic lips of the cervix will not cure the woman if these conditions persist.
If the inflammatory changes secondary to the laceration have become so deeply seated that they are not relieved by the preparatory treatment, amputation of the cervix is necessary. In any doubtful case, therefore, this preparatory treatment is to a certain extent indicative of the character of the ultimate operation to be performed.
The description of the operation already given is applicable to the most usual form of laceration—a bilateral laceration. If the injury be unilateral, it may be necessary to split the cervix on the sound side in order to denude, and to introduce sutures, on the injured side. The 163 case may then be repaired as in the bilateral form of injury. In the case of the unusual stellate laceration the lacerations must be separately repaired, or two lacerations may be converted into one by excision of the intervening tissue.
The incomplete laceration may be recognized in the manner already described, by introducing a sound into the cervical canal and a finger in the vaginal fornix. Such an injury should be treated by splitting up the cervix and converting the incomplete into a complete tear, and then denuding where necessary and closing as in the case of an open laceration.
If, in an old laceration, the sclerotic and cystic condition of the cervix does not yield to the preparatory treatment advised, amputation of the cervix is necessary.
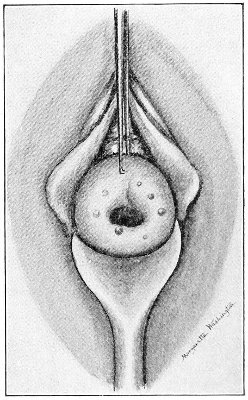
Fig. 106.—An old incomplete laceration of the cervix with hypertrophy and cystic degeneration. Amputation is necessary.
Amputation of the Cervix.—This operation is performed as follows: The cervix is split bilaterally to the vaginal junction with knife or scissors. Two flaps are formed in this way, and each flap is then amputated separately, the posterior one first (Figs. 107-109). An incision is made on the vaginal aspect of the posterior flap, extending from the angle of the split on one side to the angle of that on the other. The knife is thrust deeply into the cervical tissue and is directed toward the cervical canal. An incision is then made across the mucous membrane of the cervical canal, on the anterior aspect of this flap. The posterior lip is thus removed. The anterior 164 165 lip is removed in a similar manner. The stump of the cervix is then closed by sutures. Two or three sutures are introduced on each side of the cervix to close the angles, just as in the operation of trachelorrhaphy for a bilateral tear, and two sutures are introduced on each flap to attach the mucous membrane of the cervical canal to the mucous membrane of the vaginal aspect, to form the new external os. The first sutures should be passed well up in the angles at the lateral vaginal fornices, to control bleeding. Bleeding is more likely to be free in this operation than in a simple trachelorrhaphy, but it may always be controlled by the proper application of the first sutures placed in the angles.
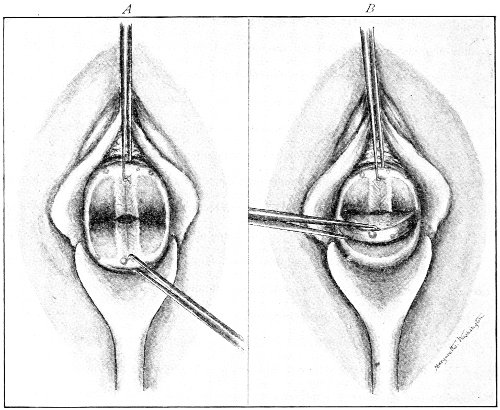
Fig. 107.—Operation of amputation of the cervix uteri: A, the cervix has been split laterally, forming an anterior and a posterior flap; B, the posterior flap has been partly amputated.
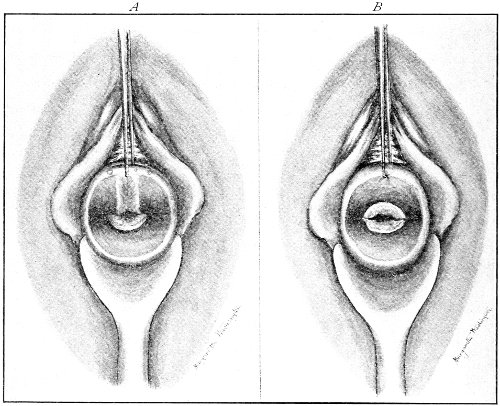
Fig. 108.—A, the posterior flap has been amputated; B, both flaps have been amputated.
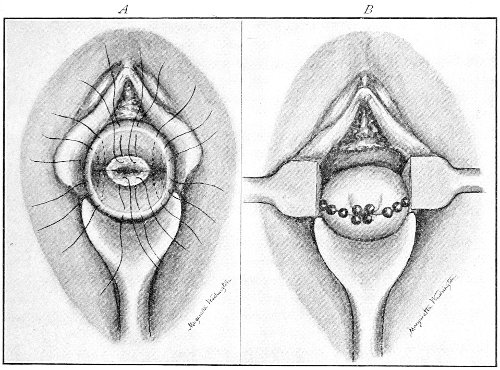
Fig. 109.—A, the sutures have been introduced; B, completed operation.
The post-operative treatment is similar to that after the operation of trachelorrhaphy.
Amputation of the cervix does not interfere with conception, with the course of pregnancy, or with labor. 166
The mucous membrane of the cervical canal may be the seat of acute or chronic inflammation. Acute inflammation usually occurs as part of a general acute process affecting the whole of the endometrium, and is commonly the result of gonorrheal or septic infection. It will be considered under General Endometritis.
Chronic inflammation of the mucous membrane of the cervical canal (cervical catarrh or cervical endometritis) is an exceedingly common affection. Unless caused by gonorrhea, it is nearly always secondary to some local or general condition.
The pathological changes that take place in the mucous membrane resemble those found in a similar process in other parts of the body. There is a very marked congestion and hypersecretion of the racemose glands of the cervical canal, so that the most prominent symptom of cervical catarrh, a profuse cervical leucorrhea, is produced. This discharge resembles the normal secretion of the cervical glands. In its physical properties it is characteristic. It is a thick, tenacious mucus, and differs decidedly from the thin, more serous discharge from the vagina or from the body of the uterus. The discharge is often opaque; it is rarely purulent, and is very rarely streaked with blood. The mucous membrane of the cervical canal becomes swollen, and may project or prolapse beyond the limits of the external os, so that the external os has around it a ring of red congested mucous membrane. A similar condition is observed on the 167 eyelids in conjunctivitis. Such a prolapse of the mucous membrane would bring the orifices of some of the racemose glands upon the vaginal aspect of the cervix, where it will be remembered they are not normally present. The inflammatory action extends beyond the limits of the external os on to the vaginal aspect of the cervix. The squamous epithelium exfoliates over a limited area around the external os, and there is produced an erosion resembling that already described under Laceration of the Cervix. Consequently, the red eroded area surrounding the external os that appears in many cases of chronic inflammation of the cervical mucous membrane is due to extension of the inflammatory process on to the vaginal aspect (with desquamation of the superficial squamous cells) and to prolapse of the mucous membrane of the cervical canal. The racemose glands may become obstructed, either as a result of thickening in the character of the secretion or of occlusion of the orifices, and small retention-cysts are formed, which often fill the body of the cervix, and, extending peripherally, appear beneath the mucous membrane of the vaginal aspect. The cervix is then said to have undergone cystic degeneration. Deep-seated inflammatory changes may also take place as a result of cervical catarrh, so that at first a slight hypertrophy from inflammatory exudate results, and later the formation of connective tissue produces a sclerotic condition of the cervix.
As has been said, chronic cervical catarrh, unless of gonorrheal origin, is nearly always secondary to some local or general condition. The most usual cause of the disease is laceration of the cervix, which causes inflammation of the mucous membrane by direct injury and exposure.
The various flexions and displacements of the uterus are often accompanied by cervical catarrh, which probably is caused by the chronic congestion brought about by interference with the circulation of the body and cervix. The use of frequent douches of cold water to prevent 168 conception is said to result in chronic inflammation of the cervical mucous membrane.
Imperfect involution after labor, miscarriage, or menstruation may cause cervical catarrh from the chronic congestion that results.
Gonorrhea seems in many cases to be communicated directly and primarily to the cervical mucous membrane, and results in a most obstinate form of chronic inflammation.
The scrofulous and tubercular diatheses seem undoubtedly to predispose a woman to chronic inflammation of the mucous membrane of the cervix, as of other mucous membranes of the body. Cervical catarrh often appears in such women without any local lesion to account for it. The severity of the local trouble depends upon the general condition, diminishing when the general health improves.
In all cases of cervical catarrh, even though dependent upon a distinct local lesion like a laceration of the cervix or a flexion of the uterus, the severity of the catarrh, as measured by the quantity of the discharge, is very much dependent upon the general health. The woman is often troubled by leucorrhea only at those times at which her general health is impaired by overwork, anxiety, or from some other cause; and even though the disease may be apparently cured by appropriate treatment, the symptom, leucorrhea, is very apt to reappear whenever the woman is subjected to such depressing influences.
The most conspicuous symptom of cervical catarrh is the leucorrhea—the discharge from the cervical glands. As has already been said, in its physical properties it is characteristic. It is a thick, opaque, tenacious mucus. The quantity is often so great that the clothes of the woman are soiled and she is obliged to wear a napkin.
There may be present slight backache and a feeling of vague discomfort or pain in the pelvis as a result of the inflammation of the cervix. It is difficult, however, to separate symptoms referable distinctly to the cervical 169 inflammation from those due to the primary trouble, to which the cervical inflammation is also to be attributed. The only one distinct symptom of cervical inflammation is the leucorrhea.
Digital examination in a case of cervical catarrh usually reveals an altered condition of the cervix. The vaginal cervix may be somewhat enlarged and soft in the early stages of the disease, or cystic and sclerotic in the later stages. The external os is usually enlarged, often admitting the tip of the index finger even in those who have not suffered with laceration of the cervix. The prolapsed mucous membrane is present, and the erosion may be readily felt around the external os, being easily distinguished from the smooth, less velvety squamous mucous membrane of the vaginal aspect.
Speculum examination shows a congested vaginal cervix and a patulous external os around which is the red erosion already described. Escaping from the external os is seen the thick cervical mucus, which is often so tenacious that it may be lifted from the cervical canal with forceps.
The diagnosis of cervical catarrh is usually very easily made from a consideration of the signs described. The important thing in any case is to determine the cause of the inflammation of the cervical mucous membrane, in order that the proper treatment may be directed to it.
Treatment.—As has been said, cervical catarrh is always secondary to some local or general condition, except in the case of direct gonorrheal infection. The gonorrheal cases must be determined by the history of the disease and by the distinctive signs of gonorrheal infection which will be described later.
In every case of cervical catarrh a thorough examination to determine the local cause of the disorder must be made. If, as will usually be the case, such a local cause is discovered, the treatment should be applied to it, and the inflammation of the mucous membrane may be disregarded, with confidence that it will disappear when the 170 exciting cause is removed. Many cases are treated by local applications, the whole attention of the physician being wrongly directed to the secondary condition, while the exciting lesion, such as laceration of the cervix, subinvolution, or a flexion or version, is neglected. Such treatment, of course, results in but temporary benefit.
Besides such cases of chronic local inflammation dependent upon a distinct local lesion, there are many others in which the catarrh is but a local manifestation of a general state of depressed or poor health, or of a distinct dyscrasia like tuberculosis, syphilis, or scrofula. Local treatment in such cases, to the neglect of the general health, is wrong.
If the advice here given—to seek for the primary cause of the cervical catarrh and to cure it—is followed, it will be found that there are but very few cases that depend for cure upon local applications. Simple local treatment by douches, etc. may, however, be valuable aids in hastening the cure of the disease after the exciting cause has been removed.
The treatment may be considered under two heads, the general and the local treatment.
General tonic treatment is required in most cases of protracted cervical catarrh. The preparations of iron are the most valuable in this condition.
The contraindication to the use of iron in uterine disease is menorrhagia or metrorrhagia—profuse bleeding from the uterus. If in any case this symptom is present, and it is found that the bleeding is increased after the administration of iron, then this drug should be discontinued.
The following are useful prescriptions in those cases in which iron is indicated:
Bland’s pill, the prescription for which may be written:
| ℞. | Pulv. ferri sulph. exsic., | ||
| Potass, carb. puræ, | āā. | ʒij. | |
| Ut fiat, massa dividenda in pilulas No. xlviii. | |||
| Sig. One pill three or four times a day. 171 |
|||
Basham’s mixture, the formula for which is—
| ℞. | Tinct. ferri chloridi, | fʒiss; | |
| Acidi acetici diluti, | fʒij; | ||
| Liquor, ammoniæ acetat., | fʒxiv; | ||
| Elix. aurantii, | fʒvj; | ||
| Glycerin., | f℥j; | ||
| Aquæ, | f℥iv. | ||
| M. | Sig. Tablespoonful after each meal. | ||
The prescription which Professor Goodell called the “mixture of the four chlorides” is—
| ℞. | Hydrarg. chloridi corrosivi, | gr. j-ij; | |
| Liq. arsenici chloridi, | gtt. xlviij; | ||
| Tinct. ferri chloridi, | |||
| Acidi hydrochlorici dil. | āā. | fʒiv; | |
| Syrupi, | f℥iij; | ||
| Aquæ, | ad | f℥vj. | |
| M. | Sig. One dessertspoonful in a wineglassful of water after meals. | ||
This prescription should not be given for more than two weeks at a time.
Careful attention should always be paid to the regularity of the bowels, in order to prevent pelvic congestion, which may result from constipation.
Two or three drams of Rochelle salts may be administered in a tumblerful of water every morning, one hour before breakfast.
A useful prescription, combining the saline purgative and the iron, is—
| ℞. | Ferri sulph., | gr. xij; | |
| Magnes. sulph., | ℥iss; | ||
| Sodii chloridi, | gr. xij; | ||
| Acid. sulph. dil., | ʒiss; | ||
| Infus. quassiæ, | ad | ℥vj. | |
| M. Sig. | One tablespoonful one hour before meals. | ||
172
An excellent laxative pill is—
| ℞. | Extract. colocynthidis, | ||
| Extract. hyoscyami, | āā. | gr. x; | |
| Massæ hydrargyri, | gr. xx. | ||
| M. | Fiat massa dividenda in pilulas No. xx. | ||
Sig. One pill three times a day.
Strychnine in addition to the iron is often a most useful medicine in cervical catarrh.
Various medicines have been administered internally to control the hypersecretion from the cervical glands. Such therapeutics, however, is not to be relied upon.
Any distinct pathological condition, like tuberculosis or syphilis, should, of course, receive the appropriate treatment.
Local treatment may be directed to the vaginal aspect of the cervix or directly to the cervical canal. The former treatment should always be tried first, and it will usually be found sufficient. It consists of the administration of hot vaginal douches, the application of Churchill’s tincture of iodine to the vaginal vault, and the use of the glycerin tampon as described under the treatment of laceration of the cervix. Puncture of the cervix in order to produce local depletion, as already mentioned in the preparatory treatment of laceration of the cervix, may also be tried.
If any case of cervical catarrh persists after the cure of the primary local or general lesion, in case such a lesion is present, and after the additional local treatment by douches and applications to the vaginal vault, then we may be obliged to make applications directly to the mucous membrane of the cervical canal.
These applications should be made as follows, any time in the menstrual interval being appropriate: The cervix should be exposed through the Sims or the bivalve speculum, and should be steadied by seizing it with a tenaculum. The cervical canal should then be wiped out with cotton either in the grasp of long thin forceps or 173 upon an applicator. The cervical mucus should be removed in this way, in order to permit the direct application of the desired solution to the mucous membrane. The applicator or forceps, armed with cotton saturated with the solution, should be introduced in the cervical canal and applied to all portions of the mucous membrane.
In place of the applicator we may use the glass pipette or instillation-tube (Fig. 110), as recommended by Skene. This instrument, charged with a few drops of the solution, should be introduced as far as the internal os, and the solution should be expressed as the pipette is slowly withdrawn.

Fig. 110.—Instillation-tube.
In most cases of cervical catarrh the external os is sufficiently large and the canal sufficiently patulous to permit the applications already described. Sometimes, however, when the external os and the canal are contracted, it is desirable to dilate slightly with the small uterine dilators before making the application. Such dilatation to one-quarter or one-half an inch may be performed without an anesthetic, and may be repeated as often as necessary.
Various solutions are used for application to the cervical canal. Violent caustics should be avoided. The solutions of mild strength are preferable. A solution of 1 or 2 grains to the ounce of chloride of zinc, sulphate of zinc, tannic acid, nitrate of silver (5 to 10 per cent.), or bichloride of mercury (1:1000) is often useful. An application of pure carbolic acid is sometimes followed by good results. Perhaps the most generally useful application is Churchill’s tincture of iodine or a solution of 2 parts of tincture of iodine and 1 part of carbolic acid. 174
In describing the lesions of laceration of the cervix and cervical catarrh, frequent mention has been made of the cervical erosion or the catarrhal patch. The erosion, or red granular area, surrounding the external os seems to be caused by various factors. In laceration it is due to the eversion and exposure of the normal cervical mucous membrane, and perhaps to slight proliferation of the cylindrical cells of this mucous membrane on to the mucous membrane of the vaginal aspect of the cervix. In cervical catarrh it is caused by swelling and prolapse of the mucous membrane of the cervical canal, and extension of the inflammatory process beyond the limits of the external os, with partial desquamation of the squamous cells.
There are other cases, however, in which the erosion appears to be congenital. Such erosions have been observed by Fischel and other investigators surrounding the external os in new-born infants. Erosion of this character has been found, in a more or less marked degree, in 36 per cent. of new-born infants. Microscopically, these erosions appear to be a direct continuation of the mucous membrane of the cervical canal. They are covered with a single layer of cylindrical epithelium, and they possess mucous glands, resembling in these features the cervical mucous membrane, and not the mucous membrane of the vaginal aspect of the cervix, which, it will be remembered, is covered with squamous epithelium and contains no glands. This congenital erosion usually is of very limited extent, but in some cases it covers the greater part of the vaginal aspect of 175 the cervix, and may then give rise to decided symptoms. The condition is due to imperfect development of the external os. In the well-formed woman there is, at the external os, a sharp line of demarcation between the squamous epithelium of the vaginal aspect and the cylindrical epithelium of the cervical canal. In the congenital erosion the epithelium of the canal extends beyond the limits of the external os, and meets the squamous epithelium at a lower level than normal.
Such congenital erosions usually give rise to no trouble, though perhaps they predispose the woman to cervical catarrh as a result of exposure of the mucous membrane. In extreme cases, however, in which the cylindrical epithelium of the cervical canal persists over the greater part of the vaginal cervix, and in which the glandular elements of the canal are found on the vaginal aspect, a distinct pathological condition arises. The symptoms of this condition resemble closely those of laceration of the cervix with ectropion. There is backache, a feeling of weight in the pelvis, and perhaps some ovarian pain. In addition, the woman complains of a leucorrhea presenting the characteristics of the cervical mucus. Decided nervous and digestive disturbances may be present.
If this condition of congenital ectropion exists along with a laceration of the cervix, the diagnosis becomes very difficult. If, however, we can exclude the possibility of a former conception, we may by careful study determine the real nature of the case.
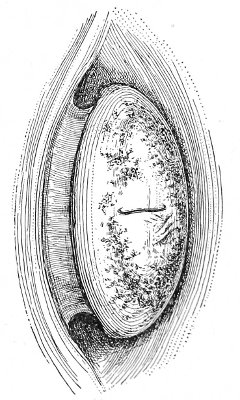
Fig. 111.—Congenital erosion of the cervix.
Fig. 111 represents the appearance of the cervix in a case of marked congenital erosion in a virtuous single woman twenty years of age. It will be observed that the appearance 176 resembles somewhat that seen in a bilateral laceration of the cervix with eversion. The following are the points of difference:
In laceration—
There is a history of previous pregnancy.
The presenting face of the cervix is oval, with the long axis antero-posterior.
The angles of laceration may be determined, by sight or touch, either as more or less well-marked depressions or as hard plugs in case they are filled up by scar-tissue. The mucous membrane of the cervical canal may be made out as a strip on the anterior and posterior lips, from which there extends laterally a more or less well-marked erosion.
The vaginal cervix is not of the general mushroom shape seen in the figure.
If microscopic examination of the cervix be made, racemose glands will be found discharging only on the mucous membrane of the cervical canal—not all over the vaginal aspect.
In the congenital ectropion—
There may be no history of pregnancy.
The presenting face of the cervix is approximately circular.
There is no angle of laceration determined by sight or touch.
The erosion may extend evenly around the external os, and there is no one strip that corresponds to the exposed mucous membrane of the cervical canal.
The vaginal cervix is mushroom-shaped, with a decided stalk.
Microscopic examination reveals racemose glands discharging over the greater part of the vaginal cervix, to the sides of the external os, as well as in front of and behind it.
The ultimate test of this condition is the discovery of the glands discharging on the vaginal aspect of a cervix in which the mucous membrane of the cervical canal had not been exposed by laceration. 177
The treatment of congenital erosion of the cervix, when it is so marked as to produce distinct symptoms, is amputation of the cervix.
Congenital Split of the Cervix.—There is sometimes found a congenital split of the cervix, closely resembling a unilateral or bilateral laceration following labor or miscarriage. The recognition of this fact is of great medico-legal importance. One of the most positive signs of a former conception is a laceration of the cervix. In some cases, however, a condition resembling such a laceration may exist from birth. Marked lateral split of the cervix has been discovered in the new-born infant, and several cases have been observed in which this condition has been found in adults of undoubted virginity.
It is possible that this condition may become pathological. Cervical catarrh might be produced from exposure of the mucous membrane of the cervical canal. The lesion, however, is not of nearly such serious moment as a laceration after miscarriage or labor, for the last injury occurs in a uterus which must undergo involution, and the chief symptoms of laceration of the cervix are usually those incident to arrested involution. 178
Cervical Polypi.—Polypoid tumors are found growing from the mucous membrane of the cervical canal, projecting into the canal or protruding from the external os. The mucous polypus is the most usual form, and is caused by cystic degeneration of the Nabothian glands of the cervical mucous membrane. Sometimes such polypi protrude from the ostium vaginæ. Less often a papillary or warty growth is found on the mucous membrane of the cervical canal, in the neighborhood of the external os. There is usually present dilatation of the external os and cervical canal. The symptoms of cervical polypi are not characteristic. Inflammation of the cervical mucous membrane and cervical catarrh may result. There may be slight, and rarely profuse, bleeding from the external os. The bleeding may follow efforts at straining, sexual connection, long standing, or exercise. Occurring at the time of the menopause or later, this symptom would excite the suspicion of beginning cancer of the cervix.
Pediculated polypi should be twisted or cut away. Bleeding is usually very slight. The sessile growths, like the papillomata, should be excised, the incision being carried well below the base of the tumor into the healthy tissue of the cervix. The wound may then be closed with an interrupted suture. In every case of such tumor a careful microscopical examination should be made to determine its benign or malignant character.
Hypertrophic Elongation of the Vaginal Cervix.—In 179 this condition there is a marked increase in the length of the vaginal portion of the cervix uteri, though the thickness of the cervix may be but little, if any, greater than normal. The vaginal cervix may be so long that the external os may lie outside the ostium vaginæ.
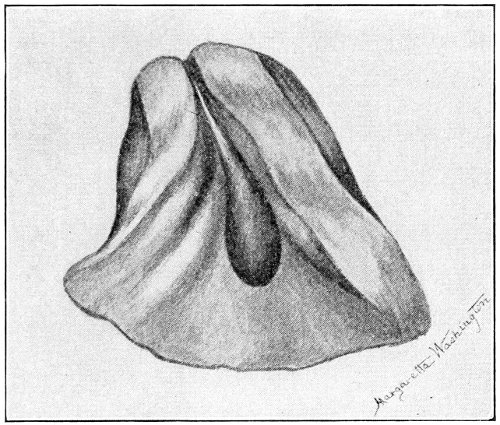
Fig. 112.—Mucous polyp of cervix.
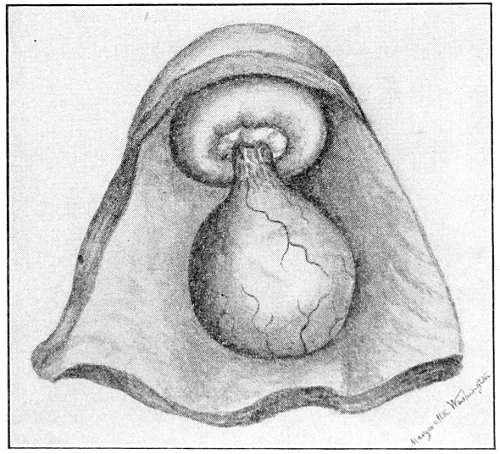
Fig. 113.—Cervical polyp.
The condition is a true hypertrophic growth, the cause of which is unknown. It is probably congenital, as it is found in the virgin.
The diagnosis between elongation of the vaginal cervix and the various forms of prolapse of the uterus and the 180 vagina may be readily made. In elongation of the vaginal cervix the fundus uteri is at the normal level; there is no inversion of the vagina; the vaginal fornices are in the normal position.
Elongation of the vaginal cervix to a degree sufficient to be considered pathological is very rare.
The treatment consists in amputation of the cervix.
Chancre of the Cervix.—Chancre of the cervix is a rare lesion. One observer, Rassennone, found 117 uterine chancres in a series of 1375 cases of venereal sores on the female genitals. The sore may occur on either lip of the cervix and may extend into the cervical canal. The appearance is that characteristic of similar sores in other parts of the body.
The diagnosis may be made from a history of coitus with a man having active syphilis, by microscopic examination if necessary, and by the later appearance of secondary syphilitic symptoms.
Tuberculosis of the Cervix.—Tuberculosis of the cervix is a very rare condition. The appearance of the cervix in such cases resembles that of cancer. In fact, hysterectomy has been performed for this condition under the mistaken diagnosis of malignant disease.
The diagnosis may be made by the microscopic examination of the discharge and of excised tissue.
Complete hysterectomy should be performed for tuberculosis of the cervix. 181
Cancer of the cervix uteri is a very common disease. About one-third of all cases of cancer in women affect the uterus. Like cancer in other parts of the body, the disease has been observed at almost every period of life except infancy. It occurs most frequently during the active mature life of the woman, between the ages of thirty and fifty. It is probable that more cases occur during the latter decade of this period than during the former.
Cancer of the cervix is a disease of the childbearing woman. It is very rare in women who have never conceived. Statistics show that women who develop cancer of the cervix have borne on an average five children. The stout, well-nourished mother of a large family is very prone to cancer of the cervix.
It is probable that the chief predisposing cause of cancer of the cervix is a fissure or laceration caused by miscarriage or labor. A focus of irritation, an area of diminished resistance, is thus developed, where cancer may start in a woman predisposed to this disease. In some of the cases of cancer of the cervix occurring in sterile women it has been found that previous traumatism had been inflicted by dilatation or incision of the cervix.
Cancer of the cervix uteri originates in one of three structures: I. The squamous epithelium covering the vaginal aspect of the cervix; II. The cylindrical cells lining the cervical canal; III. The epithelial cells of the cervical glands. The first variety is called squamous-cell carcinoma of the cervix. The second and third varieties are called adeno-carcinoma of the cervix. 182
The early appearance of the disease, the gross form assumed by the cancer, the direction of growth, and the clinical course depend upon the place of origin. In the late stages of the disease, characterized by extensive destruction of tissue, all forms appear alike.
I. Cancer of the vaginal aspect of the cervix (squamous-cell carcinoma) very often begins in a benign erosion of an old laceration. The early stages of transition from the benign to the malignant condition are not apparent to the unaided senses, and can be recognized only by the microscope. Later a superficial ulceration is developed, or the cancer may assume the polypoid or vegetating form, and become readily recognized by the unaided senses.
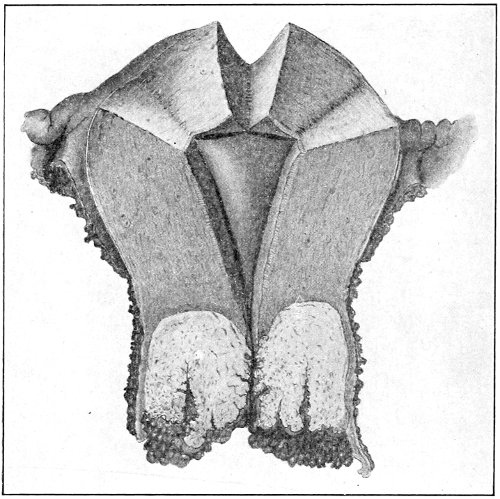
Fig. 114.—Cancer of the vaginal aspect of the cervix.
It will be remembered that true ulceration as a benign condition is very rare on the cervix uteri. The erosion of a laceration is in no sense an ulceration. An ulceration of the cervix, therefore, should always excite the gravest suspicion. The polypoid or vegetating growths vary very much in size. They are sometimes very exuberant, 183 forming large cauliflower-like masses filling the upper part of the vagina (Fig. 114). In other cases they are small warty growths or rounded protuberances about the size of a pea. The disease usually spreads to the mucous membrane of the vagina. Less often it extends to the cervical canal and to the body of the uterus.
II. When the cancer begins in the mucous membrane of the cervical canal (adeno-carcinoma), extensive destruction of tissue may take place before any appearance of the disease is observed at the external os (Fig. 115). This is most likely to occur in those cases in which there is not present a bilateral laceration of the cervix with eversion of the mucous membrane. In some cases the whole of the cervix is destroyed, leaving only a shell, the lower portion of which is the vaginal aspect of the cervix.
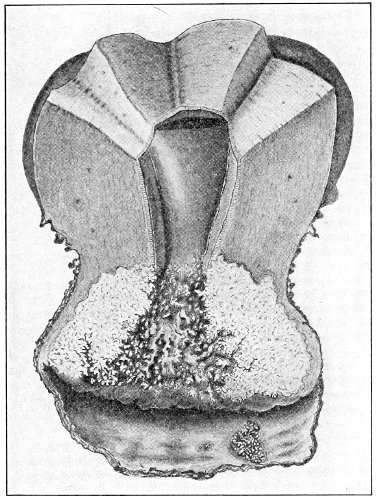
Fig. 115.—Cancer of the cervical canal, with metastasis to the vagina.
When the cervix is lacerated and the mucous membrane of the canal is exposed, the disease is more early apparent, and we may then observe the malignant ulceration 184 of the exposed mucous membrane or the presence on it of cancerous outgrowths. This form of cancer of the cervix uteri is more likely to extend upward to the endometrium than is the form first described.
III. When the cancer begins in the distal ends of the cervical glands (adeno-carcinoma), it may appear as a nodule in the body of the cervix. It will be remembered that sometimes these glands become so distended peripherally that they appear beneath the mucous membrane of the vaginal aspect of the cervix as Nabothian cysts. In a similar way, when the glands become seats of cancerous infection, hard nodules of various size may appear or be felt beneath the vaginal mucous membrane. In other cases the nodule is situated beneath the mucous membrane of the cervical canal. These nodules disintegrate and perforate the overlying mucous membrane, and in this way form a malignant ulcer which may appear either in the cervical canal or on the vaginal aspect of the cervix.
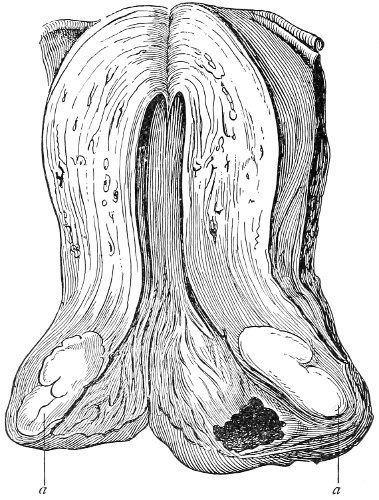
Fig. 116.—Nodular cancer of the neck of the uterus (a) (Ruge and Veit).
As has been said, when ulceration and destruction take 185 place, in the last stages of the disease, all the varieties of cancer present a similar appearance and are accompanied by similar symptoms.
Cancer of the cervix uteri may extend to the vagina, to the body of the uterus, to the broad ligaments, the bladder, rectum, ureters, and the peritoneum, and it may be carried by the lymphatic vessels to the pelvic and inguinal lymphatic glands.
In nearly all cases of long standing the upper part of the vagina is involved. Sometimes the whole of the vaginal canal, from the cervix to the vulva, is infiltrated with cancerous growths.
The body of the uterus always becomes involved sooner or later. This is most apt to occur in those cases in which the disease begins in the cervical canal. The endometrium is affected by direct extension, the malignant disease being often preceded by some benign form of endometritis.
Sometimes the cervix becomes hypertrophied by general infiltration to three or four times its usual size.
The broad ligaments are very usually involved by direct extension of the disease. They become thick, hard, and very rigid, holding the uterus fixed in the pelvis. When only one ligament is affected, the uterus is drawn to that side. The ureters become involved by extension of the infiltration to their walls or by pressure upon them by the thickened broad ligaments.
The bladder, on account of its close relationship to the cervix, is always involved in the last stages. The disease may extend to the vesical mucous membrane, and symptoms of cystitis will appear. Sometimes the vesico-vaginal septum is destroyed and a urinary fistula results. Extension to the rectum is not so common. As the disease extends upward the peritoneum may be perforated, though this is an unusual accident. In most cases peritoneal involvement is preceded by local inflammation and by adhesions which prevent direct penetration of the peritoneal cavity. 186
The pelvic and retroperitoneal lymphatic glands become affected in the later stages of cancer of the cervix.
The inguinal glands are rarely involved in the last stages of the disease. Metastasis to remote parts of the body is unusual. Cancer of the cervix usually remains localized and does not become metastatic.
From this description it will be observed that in the early stages of cancer of the cervix the disease presents a variety of appearances. As cure of the disease depends upon its early recognition, it is of the utmost importance that the physician should be familiar with these early phenomena.
When cancer begins in an erosion of a laceration, we find that the eroded surface bleeds more easily than in the non-malignant condition, and is somewhat more elevated than the surrounding surface of the cervix. We may by palpation detect around the erosion a more or less indurated edge which is not felt around a benign erosion. The submucous structures of the cervix may feel brawny and indurated. If the erosion has become an ulcer, the indurated edges and the involvement of the deeper structures of the cervix are more marked. It must always be remembered that an ulcer of the cervix is very rare as a benign condition.
In the vegetating form of cancer of the cervix we may find small warty growths, or large cauliflower-like masses, or rounded or irregular protuberances growing from the surface of the cervix. There is here also felt an induration around the base of the growth and throughout the cervix.
A very striking characteristic of cancerous growths of the cervix uteri is their friability. The warty growths or cauliflower-like masses break off readily upon even gentle palpation, and profuse bleeding often results. There is no other disease of the cervix in which the outgrowths are of such a friable and vascular character. Even in the ulcerated form of cancer the edges of the ulcer are of this same friable nature. 187
When the disease begins immediately within the external os, this opening becomes enlarged, the cervical canal is destroyed, and there is presented the appearance of a deep conical excavation, with ulcerated, unhealthy edges, in the center of the vaginal cervix. When the disease begins still higher up, the cervical canal may be the seat of extensive destruction of tissue before any lesion is visible below the external os. Usually, however, the os is sufficiently open to permit the condition of the canal above to be seen.
When the disease begins in the racemose glands of the cervix, the nodules may be felt beneath the mucous membrane of the vaginal aspect of the cervix. The whole cervix is usually indurated and somewhat enlarged. The mucous membrane overlying the nodule may appear congested, and upon palpation it is found that the overlying mucous membrane does not glide readily over the nodule, but seems to be more than normally adherent to the underlying structures.
In all the forms of cancer of the cervix there is present to a greater or less extent a general induration of the cervix. The elasticity or resiliency of the cervix is diminished or lost; this is shown not only by the sensation upon palpation, but by the fact that the cervix is not capable of dilatation, by sponge tent or otherwise, as in the normal condition.
In the last stages of the disease the gross appearance is the same in all forms of cancer of the cervix. The cervix may fill the whole vaginal vault, sometimes hypertrophied to the size of the adult fist. The presenting mass is ulcerated, gangrenous, and covered with friable vegetations bathed in thin fetid pus and blood. The vaginal vault itself is usually involved by extension of the disease. The body of the uterus is found to be enlarged, and the mass of the cervix is held rigidly in the pelvis by the thickened cancerous broad ligaments.
In some other cases, instead of a protruding mass we discover an immense crater in the vaginal vault—a crater 188 with indurated edges and sides, surmounted by the body of the uterus. The size of the crater shows that the destruction of tissue has extended far beyond the normal limits of the vaginal and supra-vaginal cervices. The interior of the crater presents an ulcerated, sloughing surface.
There is no condition which should be mistaken for cancer of the cervix in the last stages. A sloughing uterine polyp presents superficially a similar appearance, but the gangrenous mass will be found surrounded by a ring or collar, often very attenuated, of healthy cervical tissue, and the presenting tumor is usually elastic to the touch, not unyielding and friable like the cancerous mass.
In the early stages of cancer the appearance resembles closely the erosion of a bilateral laceration of the cervix. In the simple laceration, however, the erosion is soft, not indurated; there are no palpable edges; the cervix is not brawny; and it will be found that the simple erosion yields to local treatment, while the cancerous erosion does not.
Syphilitic ulceration and the ulceration of lupus are very rare upon the cervix. Syphilitic ulceration sometimes presents all the gross appearances of cancer. The history, the microscopical examination, and the therapeutic test will enable one to make a differential diagnosis.
Cystic degeneration of the cervix should not be mistaken for the nodular form of cancer, for the cysts may be seen and punctured and their character determined.
Benign fibroid tumors of the cervix are very rare, are usually single, and are larger than the nodules of cancer.
In every case of doubt, in every case in which the physician has the least cause to suspect malignancy, microscopic examination of an excised portion of tissue should be made. Examination of tissue scraped off should not be relied upon. The most suspicious portion of tissue should be seized with a tenaculum and freely 189 cut out. Pieces of tissue may be thus excised from two or more situations. In the nodular form of cancer a nodule should be seized and excised. It is perfectly justifiable, in cases which cannot thus be elucidated, to amputate the cervix and examine the whole structure.
The excision of small pieces of tissue may be done without an anesthetic, as little or no pain is caused by the operation. Bleeding is very slight, and may always be controlled by a light vaginal compress of gauze or cotton. If the case is not malignant, healing is rapid. The specimen removed should be placed in absolute alcohol and submitted to microscopical examination by an experienced pathologist.
Symptoms of Cancer of the Cervix.—A study of the early symptoms of cancer of the cervix is of the greatest importance. In the early stages the disease may be eradicated with every probability of permanent cure. Cancer of the uterus is more favorable for surgical attack than cancer in most other parts of the body. Excision of the disease is not done in the continuity of an organ or a structure, but the whole organ attached by distinct structures may be removed.
The great majority of women with cancer of the cervix come to the operator when the disease has extended too far to permit any radical treatment. Hopeless palliation is the only course to be followed. This unfortunate condition of things is due to the ignorance of the woman in regard to the significance of the early symptoms of the disease, and to the failure of the physician first consulted to insist upon a thorough examination as soon as any suspicious symptoms appear.
There is no one symptom of cancer of the cervix present in all cases, and all the common symptoms may be absent in exceptional cases until the last stages of the disease—until the disease has extended so far that cure is impossible. It is of great importance to remember this fact, so that the absence of one or more of the classical symptoms of cancer shall not engender a feeling of security 190 that may cause the postponement of a thorough physical examination.
The usual symptoms of cancer of the cervix are hemorrhage, pain, and discharge.
Hemorrhage.—The first symptom that should direct our attention to this disease is bleeding from the vagina. Such hemorrhage often first appears as a menorrhagia—as an increase in the amount of blood lost at the normal menstrual periods. The loss of blood may be greater, and the duration of the period longer. Sometimes, if the woman keeps quiet during the period, the loss of blood and the duration are about as usual; but if she is upon her feet the loss is increased, and if she begins an active life immediately after the usual duration of the menstrual period has elapsed, bleeding may reappear for one or more days.
In other cases slight bleeding appears in the menstrual interval. A spot of blood may be discovered upon the clothing. The accustomed leucorrheal discharge may occasionally be streaked with blood. Such appearances are most frequent after long walking or standing or physical work, or after straining at stool, or very often after coitus.
If the woman has passed the menopause, the hemorrhage of cancer may appear as a re-establishment of menstruation—often to the satisfaction of the woman. This post-climacteric bleeding may occur with more or less regularity—every month or every three or four months—or it may appear as an occasional loss of blood after unwonted effort.
All hemorrhage of this kind, in women over thirty years of age, demands immediate and careful physical examination. Any bleeding from the vagina in a woman who has passed the menopause should arouse the gravest suspicion. From the slight hemorrhages just described the bleeding increases in intensity and duration, until there is a continuous loss of blood that saps the strength of the woman and produces the profound anemia characteristic 191 of the last stages of cancer of the cervix, Sudden fatal hemorrhage in this disease is rare.
Pain is not a constant accompaniment of cancer of the cervix in the early stages, nor is it in any way characteristic. The intensity and character of the pain may depend upon the direction of the growth of the disease. In some cases pain is absent throughout. The pain may be dull and gnawing in character, or it may be sharp and lancinating. The pain may resemble that of uterine colic. It may be referred to the back in the region of the sacrum, or to one or both ovarian regions, or to some part of the pelvis remote from the uterus, as the crest or the anterior superior spine of the ilium. It may extend down the posterior or anterior aspects of the thighs or into the rectum. In most cases of cancer of the cervix pain is not a prominent symptom until the later stages.
Discharge from the vagina may be present in cancer of the cervix before there are any symptoms of hemorrhage or pain. The discharge depends upon the position and character of the growth and the stage of the disease. It may first appear as an ordinary cervical leucorrhea in a woman previously free from such discharge; or the discharge of cancer may first appear as an increase of an accustomed leucorrhea. In such cases it is due to hypersecretion from the irritated cervical glands.
Later in the disease, when ulceration takes place or when the friable vascular vegetations appear, the leucorrhea becomes puriform in character and streaked with blood. It then becomes thinner, less mucous in consistency, and of a constant brownish color from the admixture of blood. The pus and débris from the breaking-down cancerous mass increase, and a horrible odor characteristic of the later stages of cancer of the cervix appears. This odor is not peculiar to cancer. It is caused by the sloughing tissue, and is observed when such a process occurs in other conditions, as in sloughing fibroid polyp. The discharge is irritating in character, and the ostium vaginæ, the vulva, and the inner aspects 192 of the thighs become excoriated in those who do not observe strict cleanliness.
Systemic absorption of the cancerous discharges produces a general septic condition, which, with the anemia from hemorrhage and the uremia from obstruction of the ureters, results in the so-called cancerous cachexia.
The symptoms that have just been described are those most usual in cases of cancer. It must always be remembered, however, that these symptoms vary very much in intensity or prominence and in the stage of the disease at which they appear. Sometimes acute pain, hemorrhage, and excessive discharge are present from the very beginning—even before the presence of cancer can be demonstrated without the aid of the microscope. In other cases all these symptoms may be absent until the disease is very far advanced. None of the symptoms are absolutely pathognomonic of cancer. During the menstrual life of the woman hemorrhage from the womb occurs as a symptom of a great variety of diseases; and even in the post-climacteric period, though hemorrhage should always excite alarm, yet it may be caused by a benign form of endometritis or intra-uterine growth. The pain of cancer may also characterize a variety of benign conditions; and the vaginal discharge, even when most offensive, may be simulated by that from a sloughing intra-uterine fibroid.
The symptoms, however slight, which we know may occur with cancer of the cervix should never be disregarded. Examination should be made immediately. There should be no postponement or expectant plan of treatment. If physical examination is not satisfactory in elucidating the condition, resort should be had to the microscope. If this is not conclusive, the case should be watched as long as the suspicious symptoms continue, and further frequent examinations should be made.
If this plan of treatment is followed, and if women are taught to view with distrust, and not with complacency, any irregularities of menstruation occurring near the time 193 of the menopause, or any post-climacteric return of menstruation or of irregular bleeding, the surgeon will be able to save many women with cancer of the womb who are now doomed to horrible deaths.
Cancer of the cervix, like cancer in other parts of the body, is of variable duration. Usually from one to three years elapse between the time when the first symptoms of the disease appear and the time of death. The disease may run its course, in exceptional cases, in a few weeks; in other cases it may last as long as five years, especially if the progress is delayed by palliative treatment.
Treatment.—Complete removal of the uterus is the only curative treatment for cancer of the cervix. If the disease is seen in the earliest stages, amputation of the cervix beyond the limits of the growth seems, theoretically at least, to be a proper plan of treatment. Practically, however, the operator can never be certain that the excision is made in healthy tissue. The senses of touch and unaided sight are not capable of defining the limits of malignant infiltration. Moreover, it must be remembered that the endometrium is very often involved secondarily from a cancerous focus in the cervix. Complete removal of the uterus should therefore always be practised in all cases in which there is a possibility of removing all of the disease.
The manner of performing this operation will be described subsequently.
The cases that are not suitable for the operation of hysterectomy are those in which the disease has extended to structures that are surgically inaccessible. Such cases include those in which the bladder or the rectum are involved, those in which the vagina is extensively implicated, and those in which the disease has extended into the broad ligaments or the cellular tissue of the pelvis.
When the bladder is involved, there are dysuria, vesical pain, and tenderness on vaginal pressure upon the base of the bladder, while the urine is altered in character, 194 containing blood, pus, and, in the later stages, broken-down necrotic tissue. Involvement of the rectum is manifest by digital examination.
When the broad ligaments are involved the uterus is held rigidly in the pelvis or is drawn to one side, and the bases of the broad ligaments, palpated through the lateral vaginal fornices, are thick and hard. When the cellular tissue of the pelvis is generally involved the whole vaginal vault feels indurated and the uterus seems fixed in the unyielding matrix.
In examining with the view of determining the practicability of hysterectomy, it is important to distinguish between cancerous and simple inflammatory involvement of the broad ligaments. The uterus may be fixed in the pelvis by inflammatory adhesions resulting from old tubal disease, and yet the cancer of the cervix may be strictly local and in a stage suitable for hysterectomy. In the simple inflammatory cases the adhesions are more attenuated, are higher in the pelvis, and lie chiefly posterior to the uterus. They are not directly continuous with the cervix. Frequently the enlarged tube and the adherent ovary may be felt. When the uterus is fixed by cancerous involvement of the broad ligament, we readily feel that it is the base of the broad ligament that is involved. The induration is broad, it is directly continuous with the induration of the cervix, and it lies to the side of the uterus.
Involvement of the pelvic lymphatic glands may sometimes be determined by vaginal palpation, one or more such enlarged indurated glands being felt lying posterior to the uterus. In most cases, however, glandular involvement can be determined only after the abdomen has been opened.
In general, it may be said that the operation of hysterectomy should be performed in all cases in which there is no cancerous involvement of the bladder and rectum, in which the vaginal disease may all be removed, and in which the uterus is freely movable. 195
In those cases in which complete removal of the disease is impossible the operation of hysterectomy should not be performed, because, cure being out of the question, the symptoms of hemorrhage, pain, and discharge may be as well relieved by less dangerous forms of palliative treatment. When the disease extends beyond the limits of the uterus, hysterectomy is much more difficult and dangerous than when the uterus is freely movable.
The remote results of hysterectomy for cancer of the cervix are poor. In the very great majority of all cases submitted to operation recurrence has taken place. It seems very probable that a few of the cases of recurrence are due to transplantation of cancer-cells into healthy tissue during the operation; but the vast majority die because all of the diseased tissues have not been or can not be removed. The hope for better results from the surgical treatment of cancer of the cervix depends, not upon improvement in the surgical technique, but upon the ability of the general practitioner to recognize the disease in its earliest stages, before inaccessible structures have been involved.
Palliative Treatment of Cancer of the Cervix.—The palliative treatment consists in removing as thoroughly as possible, with the sharp spoon-curette, scissors, or knife, all the cancerous cervix, and the maintenance of the surfaces thus exposed, as far as possible, free from septic infection.
The woman should be placed in the lithotomy position; the cervix should be exposed with the Sims speculum and, if necessary, with the lateral vaginal retractors. All vegetations and all of the degenerated cervix should then be cut away. It is usually necessary to carry the excision of tissue as high as the internal os. Bleeding during this procedure is sometimes very profuse. It diminishes, however, as the more degenerated portions of the cervix are cut away and the healthier uterine tissue is reached, and therefore it is always best to complete the operation, notwithstanding hemorrhage. 196
The bleeding may be controlled by packing the cavity with gauze or cotton, plain or saturated with Monsel’s solution. Moderate bleeding may be checked by packing with cotton saturated with a 5 per cent. solution of antipyrine.
In rare cases, in which the excision of tissue has been carried high up in the lateral vaginal fornices, it may be necessary to ligate the uterine arteries in order to control the hemorrhage. This may be done by passing around the vessel, close to the cervix, a curved needle carrying a heavy ligature. Bleeding from the circular artery may readily be controlled in a similar way, the ligature being passed like the first suture in trachelorrhaphy.
If the operation has been thoroughly performed, there will be left a large crater or conical cavity in the vaginal vault. This cavity may then be packed with sterile gauze, or, if there is much bleeding, with gauze saturated with Monsel’s solution. Some surgeons sew together the walls of the cavity to diminish as much as possible the raw surface. Others char the walls with the actual cautery, in order to carry the destruction of tissue still farther than has been done with the knife. If the removal with the curette and knife has been thorough, it is not necessary to make a caustic application. If, however, the cavity is walled by obviously cancerous tissue, the use of the caustic is advisable. This is usually the case.
Chloride of zinc is a valuable caustic in cancer of the cervix. It should be applied as follows: After the cancerous tissue has been removed as thoroughly as possible with the knife, the scissors, and the curette, bleeding from the walls of the cavity should be checked by packing with gauze, dry or saturated with a 5 per cent. solution of antipyrine. The bleeding may very often be checked in this way in a few minutes, and in this case the caustic may be immediately applied. In case, however, the bleeding is not so quickly controlled, the packing must be left in the cavity for twenty-four hours, at 197 the end of which time it may be removed, without anesthesia, and the caustic application may be made.
Before introducing the caustic the vagina and the vulva should be protected by thorough greasing with an ointment composed of 1 part of bicarbonate of soda to 3 parts of vaseline.
The strength of the caustic should depend somewhat upon the thickness of the tissue that separates the cavity from the peritoneum or other important structures. The thickness may be approximately determined by palpation. Usually a 100 per cent. solution of chloride of zinc may be safely employed. If the walls of the cavity appear very thin—less than a quarter of an inch—the caustic may be reduced to a 50 per cent. solution. Small balls of cotton, about half an inch in diameter, should be saturated with the caustic and carefully packed in the cavity. The operator should be careful to remove quickly with the sponge any excess of caustic that may be expressed from the cotton. Much unnecessary pain may be experienced if the caustic comes in contact with the vagina or the vulva.
When the cavity has been filled with the cotton balls carrying the chloride of zinc, a large vaginal tampon of cotton well greased with the alkaline ointment should be placed in the vaginal vault. The packing should be removed from the vagina in forty-eight hours, and vaginal douches of bichloride of mercury, 1:4000, should be administered.
If this operation is carefully performed, the subsequent pain is usually slight. In some cases, however, the action of the caustic may be so painful that morphine is required.
The slough from the caustic may be discharged in one piece or in shreds. It is usually separated in from five to ten days.
The subsequent treatment of the woman consists in the frequent use of cleansing vaginal douches, such as a solution of bichloride of mercury (1:4000), carbolic acid (3 198 per cent. solution), permanganate of potash (10 grains to the ounce of water), and peroxide of hydrogen (1 part of the commercial peroxide to 3 or 4 parts of water).
The palliative treatment of cancer relieves the pain, the hemorrhage, and the discharge. The relief is usually immediate, and may continue throughout the disease. The hemorrhage is usually arrested for several weeks, or even for months, and the discharge is much diminished with the destruction of the necrotic cancerous mass. The progress of the disease is delayed, and life is somewhat prolonged. 199
Acute inflammation of the mucous membrane of the body of the uterus is called acute corporeal endometritis. The disease is usually the result of septic infection occurring at a labor or a miscarriage. Occasionally acute gonorrheal endometritis is seen, but this disease usually produces an inflammation of the mucous membrane of the cervix and the body of the uterus that is chronic or subacute from the beginning. Septic infection through operative traumatism, through the use of the uterine sound, or through other gynecological methods of examination may, of course, result in acute endometritis.
The pathological changes that take place in an endometrium that is the seat of acute inflammation resemble those seen in acute inflammation of mucous membranes of other parts of the body. The secretion of the utricular glands becomes much increased in quantity and altered in character, becoming purulent and sometimes containing blood.
As would be expected, whenever the inflammation is at all severe the middle or muscular coat of the uterus is involved by the process; in other words, a metritis follows and accompanies the endometritis. In puerperal metritis abscesses varying in size from a pin-head to that of a hen’s egg are sometimes found in the uterine wall.
The septic infection may extend through the muscular wall of the uterus and involve the peritoneal covering, producing in this way a perimetritis.
Acute inflammation of the endometrium sometimes occurs during the course of the exanthemata. The 200 changes that take place in the mucous membrane of the uterus are similar to those seen in other mucous membranes during the course of these diseases. The local condition is usually limited by the duration of the general disease.
It is probable that some of the cases of arrested development of the internal organs of generation, and cases of chronic tubal and ovarian disease seen in later life, may be traced to this exanthematous form of endometritis occurring during girlhood.
The symptoms of acute endometritis vary very much in severity. Dull pain in the region of the uterus, referred to the supra-pubic region and the sacrum, is usually present. Reflex disturbance of the bladder, characterized by frequent and often painful urination, may be present; and it is very probable that mild cases of endometritis have been diagnosed and treated as light attacks of cystitis. The temperature in the puerperal cases may be very high. The discharge from the cervix is very much increased, is puriform in character, and is occasionally streaked with blood.
Digital examination shows that the external os is patulous, the cervix enlarged and soft, and the body of the uterus somewhat enlarged and tender upon pressure. This tenderness may be elicited by pressing the fundus between the vaginal finger in the anterior vaginal fornix and the abdominal hand. Examination through the speculum shows the discharge escaping from the external os. In case the cervical mucous membrane is also involved, a red area of erosion will be seen surrounding the os.
Acute endometritis of non-puerperal origin is best treated by rest in bed, vaginal douches of hot boric-acid solution (ʒj to a pint of water) or of bichloride of mercury (1:4000) at a temperature of 100° to 110°, and the continuous use of saline purgatives. Active intra-uterine treatment in these cases is not necessary. When, however, the disease occurs, as it usually does, from septic infection at a miscarriage or a labor, more 201 radical treatment must be used. This treatment comprises frequently-repeated intra-uterine douches, thorough curetting of the uterus, and, finally, hysterectomy in extreme cases.
Every case of acute endometritis should be carefully watched and treated until the disease is cured. Acute endometritis, especially if gonorrhea is the cause, is very prone to become chronic and to extend to the mucous membrane of the Fallopian tubes and the ovaries.
Chronic inflammation of the endometrium, or chronic endometritis, is much more frequently seen in practice than the acute form. It may occur as a primary disease, but it very often occurs as the result of some other pathological condition of the uterus, as, for instance, subinvolution or uterine fibroid.
A variety of confusing terms have been used to designate the different forms of endometritis. There seem to be two chief forms of the disease: I. Chronic interstitial endometritis; II. Chronic glandular endometritis.
In the first form of the disease the interglandular tissue is chiefly involved. The spaces between the glands are infiltrated with connective-tissue cells.
In the second or glandular form of endometritis the disease affects the glandular apparatus. The utricular glands become much elongated, branched, and increased in number. The accompanying illustrations (Figs. 117, 118) show the microscopic appearance of interstitial endometritis and glandular endometritis.
These two forms of endometritis are often mixed, and the same uterus may present the glandular form of inflammation upon part of the endometrium, the interstitial form upon another part, and the mixed form upon still another part.
The gross appearance of the endometrium varies with the form of the disease and its duration. It will be remembered that in the mature uterus, in the menstrual 202 203 interval, the mucous membrane is a thin reddish-gray structure about 1 millimeter (1/25 inch) in thickness. In the different forms of endometritis the mucous membrane may become hypertrophied to three or four times this thickness. In some unusual cases the mucous membrane may become even still further hypertrophied, attaining a thickness of half an inch. A special name, fungous endometritis, has been given to the disease when it assumes this form. Microscopic examination shows that fungous endometritis is merely a mixed form of the glandular and the interstitial varieties, with a great increase of all the elements of the mucous membrane. In fungous endometritis the hypertrophy of the mucous membrane may be uniform throughout the body of the uterus or it may occur only in localized areas.
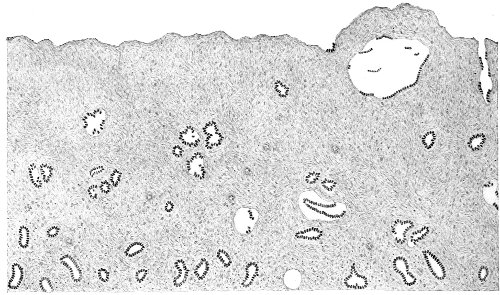
Fig. 117.—Interstitial endometritis: microscopic section of endometrium removed by the curette (Beyea).
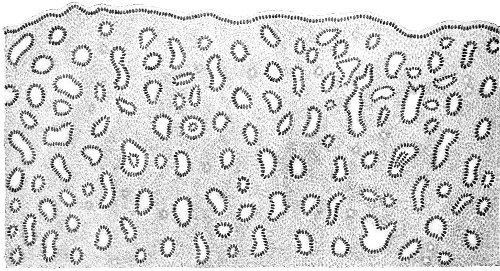
Fig. 118.—Glandular endometritis: microscopic section of endometrium removed by the curette (Beyea).
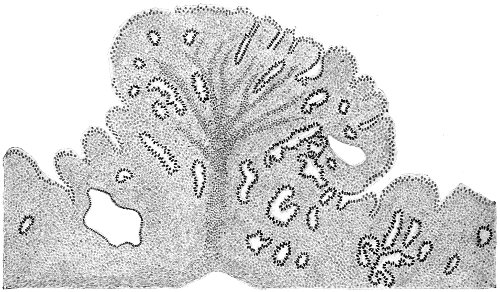
Fig. 119.—Polypoid endometritis (Beyea).
In some cases the glandular hypertrophy of the mucous membrane assumes the form of polypoid growths projecting into the uterine cavity (Fig. 119).
In the advanced stages of all the forms of endometritis cicatricial formation takes place. The normal ciliated epithelium of the endometrium is cast off, and is replaced by flat squamous cells. The glands atrophy; the glandular openings become dilated, and ultimately appear as simple depressions on the surface. In time secretion from the glands ceases, and the cavity of the uterus becomes lined with simple connective tissue.
Chronic endometritis is always accompanied to a greater or less extent by inflammation of the muscular coat of the uterus. The pathological changes that take place resemble those occurring in chronic inflammation in similar musculo-fibrous structures in other parts of the body. A section of the uterine wall is much lighter in appearance than normal, and the whitish bundles of connective tissue are seen interlacing with the more vascular muscular fibers.
At first there is an hypertrophy of the uterine wall from infiltration of inflammatory material. In the latest stages organized connective tissue is formed, and there is 204 produced a sclerotic condition of the uterus, with atrophy of its normal muscular elements.
The hypertrophy of the uterus, however, that accompanies most of the forms of endometritis is not due altogether to the presence of inflammatory deposits. The uterus possesses the peculiar property of enlarging, by a general hypertrophy of its elements, whenever there is present in its cavity any gross pathological condition. We see this in fibroid tumor. And, as a general rule, the enlargement is proportional to the mensurable size of the disease.
The metritis may involve the whole of the uterine body, or it may occur in localized areas. It may affect only the body of the uterus, or the body and the cervix, or, as we have already seen, the cervix alone. When the disease is localized to part of the uterine wall, the induration of the affected area may sometimes be determined by palpation.
Symptoms.—The symptoms of chronic endometritis are often obscured by symptoms that are to be referred to other accompanying conditions. For instance, the endometritis very often accompanies subinvolution of the uterus, laceration of the cervix, uterine displacement, or ovarian and tubal disease. Cases of simple uncomplicated endometritis are the exception.
The menstrual function is usually affected. The period is of longer duration, the loss of blood is greater, and the periods may occur more frequently than normal; in other words, there is present menorrhagia. In this disease bleeding also occasionally occurs between the menstrual periods. Hemorrhage is a symptom that is most prominent in cases of interstitial and fungoid endometritis.
The secretion of the utricular glands is also increased in amount. This symptom is most pronounced in cases of glandular endometritis. The secretion is thin and purulent in character, and is often streaked with blood. It decomposes very readily, and consequently is often 205 offensive and excites the suspicion of malignant disease.
The character of the typical discharge from the body of the uterus is usually obscured by admixture with discharge from the cervical mucous membrane. Cervical catarrh, or inflammation of the cervical mucous membrane, may, and usually does, occur alone, without involvement of the upper endometrium, but chronic corporeal endometritis is usually associated with inflammation of the cervix. If the discharge is observed at the vulva, it will be still further altered by admixture with the vaginal secretion. The discharge from the corporeal endometrium is thinner and more serous than the mucus of the cervical canal, and is more usually purulent and streaked with blood.
The discharge from the endometrium is very often increased very decidedly immediately before and after the menstrual period.
Pain is a general symptom of chronic endometritis. The pain is uterine in character, and is referred to the lower abdomen and the back. There is also very constantly present reflex headache localized on the top of the head or in the occiput.
The pain may be present at all times, but it is usually most marked when the woman is upon her feet and the pelvic congestion is increased. The pain is always greatest immediately before and during the menstrual period.
General physical weakness and debility are often very pronounced, and seem to be out of proportion to the extent of the local disease. This same phenomenon has been spoken of in the consideration of uterine displacements. The weak and aching back, the dragging sensations in the pelvis, the tired legs, may all appear after the woman has been upon her feet but a short time, and utterly incapacitate her for any kind of labor.
Nervousness, neurasthenia, hysteria, and mental depression and melancholia are apt to occur in this disease. Such nervous phenomena are common to all diseases of 206 the uterus. The mental depression is often very marked, and is exaggerated before and during each menstrual period.
The woman with chronic endometritis is usually sterile; or if she becomes pregnant, abortion will probably occur. The discharges in the uterine cavity are inimical to the spermatozoa, and the diseased endometrium furnishes an inefficient place for the attachment of the ovum.
Physical examination in a simple case of chronic endometritis shows a somewhat enlarged uterus, more globular in shape than normal. The fundus uteri is tender on pressure between the vaginal finger and the abdominal hand. The external os is usually patulous.
Examination with the speculum shows the discharge escaping from the external os. If there is also present cervical endometritis, the discharge presents the characteristics of both cervical and corporeal mucus. It is thick and tenacious, puriform, and often streaked with blood. After the cervical canal has been wiped out the characteristic corporeal discharge may appear unmixed with cervical mucus. This discharge is thin, purulent, and may be streaked with blood, or it may be brownish in color from mixture with altered blood.
If the uterus is examined with the uterine sound, it will be found that the internal os is patulous; the fundus is decidedly tender upon gentle pressure with the sound, and even the gentlest use of the sound may be followed by bleeding.
The patulous condition of the cervical canal and the internal os is a constant characteristic of all kinds of gross disease in the cavity of the uterus. The external os is usually patulous when the cervical mucous membrane is diseased. The external os, the cervical canal, and the internal os are open when the corporeal endometrium is diseased.
The only certain method of making the diagnosis is by the use of the sharp uterine curette, and this instrument 207 should always be employed whenever there is even the slightest suspicion of the possibility of malignant disease of the endometrium. The cervical canal is usually sufficiently open to permit the use of the curette without dilatation and without an anesthetic. Three or four strips of the endometrium should be removed from different parts of the uterine cavity, and should be submitted to microscopic examination. It is always safest to perform curetting for diagnosis at the house of the patient, and to keep her in bed for two or three days after the operation. Strict antisepsis should be observed.
The causes of chronic corporeal endometritis are various. Almost any disease of the body of the uterus or of the cervix may eventually result in this condition; therefore the different causes of chronic endometritis will be better appreciated after a discussion of diseases of the uterus. Laceration of the cervix, subinvolution, flexions and versions, fibroid tumors, etc., all produce, in time, some form of chronic endometritis.
Primary chronic endometritis may result as a later stage of the acute disease, or it may exist from the beginning in the chronic form. This is especially true of endometritis caused by gonorrhea. Here the invasion of the disease is slow and insidious, and in the majority of cases is preceded by no determinable acute stage.
Sometimes endometritis appears in old women. Bleeding from the uterus, purulent discharge, and pain may be present. The condition is due to the atrophic changes of senility occurring in the endometrium—changes that resemble those that take place in the mucous membrane of the vagina and the external genitals. Though such symptoms may be indicative merely of a benign condition, yet, as they are also characteristic of the early stages of malignant disease, they demand immediate thorough examination and careful watching.
Treatment.—As chronic endometritis is usually secondary to some disease of the cervix or body of the uterus, 208 the treatment should be directed toward the cure of this primary condition.
The operation of trachelorrhaphy will cure the subinvolution of the uterus and the resulting endometritis. Forcible dilatation of the cervix, in the case of an old anteflexion, will relieve the inflammation of the endometrium. Correction of a retroversion will likewise relieve the resulting endometritis. Therefore, though in every case the cure may be hastened by treatment applied directly to the endometrium, yet causative or complicating conditions must always also be treated if we wish the cure to be lasting.
Many cases of mild endometritis may be relieved or cured by attention to the general hygiene and habits of the woman and by applications made only to the vaginal aspect of the uterus. The dresses should be worn loose about the waist and supported from the shoulders. Prolonged standing and slow walking should be avoided. Mild purgation with salines should be maintained. Regulated exercise or general massage should be prescribed. In addition, the vaginal douche, iodine applications, and the use of the glycerin tampon, with depletion from puncture of the cervix, should be used, as has already been prescribed for the subinvolution accompanying laceration of the cervix.
If these methods fail after careful trial, direct treatment must be applied to the endometrium.
The present method of treating chronic corporeal endometritis directly is by the uterine curette. Time is wasted by the use of applications to the interior of the uterus, and a great deal of harm has resulted from such applications carelessly made.
The best curette is the Sims sharp curette (Fig. 120). The Martin curette (Fig. 121) is useful to remove the endometrium from the fundus.
The operation had best be performed in the menstrual interval, though it may safely be performed during the menstrual period. An anesthetic should always be administered. 209 The woman should be placed in the dorso-sacral position, with the feet in the supports. The vulva, vagina, vaginal cervix, and buttocks should be thoroughly sterilized.

Fig. 120.—Sims’s sharp curette.
The anterior lip of the cervix should be grasped with a double tenaculum. The cervical canal should be wiped out with a small sponge or with cotton and irrigated with bichloride, if the external os is sufficiently patulous. The cervical canal and the internal os should then be dilated to about one inch. The position of the uterus should have been previously determined by careful bimanual palpation.

Fig. 121.—Martin’s curette.
The Sims curette should be gently introduced to one cornu and then drawn methodically over the whole of the uterine surface, removing the endometrium in parallel strips, the length of each strip being equal to the distance between the internal os and the fundus. The curette may be withdrawn from the uterus and washed in distilled water as each strip is removed, or withdrawal and washing may be done after two or three strips have been removed. The Martin curette should then be introduced to one cornu and scraped over the fundus, as there is usually in this situation a narrow strip of endometrium that is not removed by the Sims curette.
The uterus should then be washed out with warm sterile water or with a 1:4000 bichloride solution. The washing may be done by holding the cervical canal open with the small dilator and introducing the long tubular syringe nozzle, or by some form of reflux tube (Fig. 122). 210 Opportunity must always be afforded for the escape of the irrigating fluid.
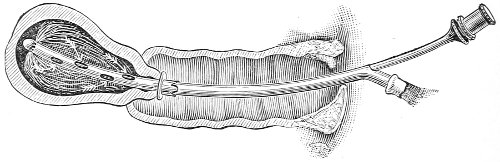
Fig. 122.—Irrigation of the uterus.
The operator should always remember the danger of perforating the uterus by the curette. This accident, which has happened in the hands of the best surgeons, occurs usually as the instrument is introduced, not as it is withdrawn. It is much more liable to occur after labor or recent abortion, when the uterine tissues are soft, than in the conditions now under consideration. If perforation should happen, the uterus should be carefully washed out with the bichloride solution, the vagina should be lightly packed with gauze, and the patient returned to bed. A hypodermic injection of ergotin should be administered, and afterward, when the woman recovers from the anesthetic, small repeated doses of fluid extract of ergot should be administered to ensure uterine contraction. If the operation has been performed aseptically, it is probable that no harm will result from the accident. If peritonitis should develop, celiotomy must immediately be performed.
After curetting the uterus some operators are in the habit of packing the uterine cavity with sterile or iodoform gauze. This procedure is liable to obstruct the escape, rather than favor the drainage, of any discharges from the cavity of the uterus. Elevation of temperature and uterine pain are often caused by it; therefore it is best, after the operation of curetting, merely to pack the vagina lightly with sterile gauze, which should be removed in forty-eight hours. Daily douches of a 1:4000 211 bichloride-of-mercury solution should then be administered as long as the woman remains in bed. The vagina should be carefully dried after the douche, as already advised.
Hemorrhage is never profuse during curetting, and usually ceases after the endometrium has been removed and the uterus has been washed out.
In cases of gonorrheal endometritis it is advisable, after the uterus has been douched and the bleeding has ceased, to apply carbolic acid thoroughly over the whole interior of the uterus, because infection may lurk in the distal ends of the utricular glands, which are not removed by the curette.
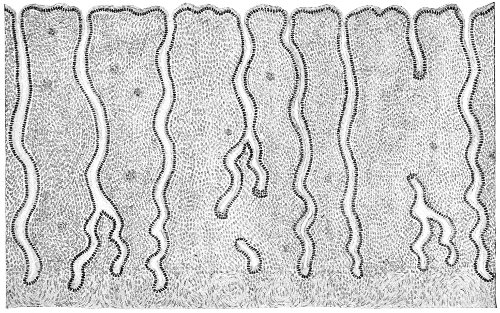
Fig. 123.—Microscopic section of the normal endometrium, showing the utricular glands extending into the muscular tissue (Beyea).
The length of time during which it is advisable to keep the woman in bed depends upon the extent and nature of the disease for which the curetting has been done. As a general rule, the longer the stay in bed the better it is for the woman. If the uterus is much enlarged or if subinvolution is present, the patient should stay in bed for two weeks. Such rest in the recumbent position 212 diminishes the congestion of the pelvic organs and is of great aid in restoring the parts to a normal condition. Careful attention should be paid to the regularity of the bowels. Mild purgation with saline purgatives should be continued during the convalescence. Daily massage, started two or three days after the operation, will facilitate the cure.
All the endometritial structures are never completely removed by the curette. The distal ends of the utricular glands, which penetrate the muscular coat of the uterus (see Fig. 123), remain after thorough and vigorous curetting.
After removing the endometrium with the curette the cavity of the uterus does not become lined with a cicatricial membrane, but a new endometrium is produced. It is probable that the new membrane is developed from the remains of the utricular glands. The new endometrium grows in a very short time. In some cases it has been sufficiently well formed to permit pregnancy five weeks after curetting.
The first menstrual period, and sometimes the second and third, after the operation of curetting may be missed. As a general rule, the menstrual bleeding is much less profuse than before the operation.
The therapeutic object of curetting for endometritis is to replace the diseased endometrium by a new membrane which has grown under conditions of rest and asepsis.
There is a disease which has been called membranous dysmenorrhea or exfoliative endometritis, in which large membranous pieces of the endometrium or a cast of the whole structure is thrown off at the menstrual period (see Fig. 124). The condition is most often found in virgins or sterile women. The membrane may be thrown off at every menstrual period, or at periods separated by intervals of various length. 213
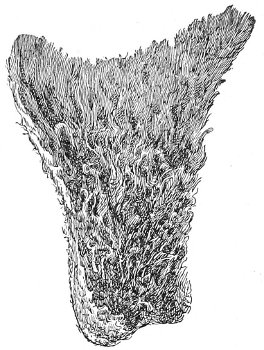
Fig. 124.—Membrane discharged in membranous dysmenorrhea.
The menstrual period is usually accompanied by intense uterine pain, which may resemble labor-pain, and which persists until the separation of the endometrium. In some cases of this disease menstruation is very irregular.
The diagnosis is made from examination of the characteristic membrane that is discharged. The condition should not be confused with abortion, in which the large irregular decidual cells will be discovered. Some women are very liable to early menstrual miscarriage, and have repeated accidents of this kind, which in some cases have led the physician to believe that the condition of exfoliative endometritis was present.
The local treatment consists of dilatation and curetting of the uterus, which operation it may be necessary to repeat several times. Careful attention should be directed toward re-establishing or maintaining the general health.
This disease, also called post-climacteric endometritis, occurs at any period after the menopause. There is a thin seropurulent discharge from the uterus, often so profuse as to soil the clothing. The quantity of the discharge may be increased with a certain monthly periodicity. The discharge is often streaked with blood, or is brown colored from the presence of altered blood. There may be occasional or even continuous slight hemorrhage from the uterus. The discharge is usually fetid, and may be exceedingly irritating to the vagina and vulva. The objective symptoms often resemble in all respects the symptoms of cancer of the body of the uterus. 214
There is usually dull pain in the lower part of the abdomen and the back; and if the disease continues for sufficient time, there may appear symptoms indicative of septic absorption—loss of appetite, emaciation, and slight elevation of temperature.
The pathologic changes which take place in the uterus in this disease have not been definitely determined. It seems probable that in some cases the condition may be produced, as in senile vaginitis, by infection of an endometrium the integrity of which had been impaired by the atrophic changes occurring after the menopause. Microscopic examination of portions of the endometrium removed by the curette shows the appearance of long-standing chronic inflammation.
These cases are often mistaken for cancer of the body of the uterus, and the diagnosis should always be immediately made by microscopic examination of the material removed by a thorough curetting of the whole of the uterine cavity.
The treatment of senile endometritis consists of applications to the endometrium of a solution of nitrate of silver, from one-half to one dram to the ounce of water, or of thorough curetting of the endometrium. 215
Subinvolution of the uterus is a condition that results from imperfect involution of the uterus after labor, abortion, or miscarriage. The muscular and fibrous structures of the uterus, which had become hypertrophied under the influence of pregnancy, fail to undergo properly the retrograde changes of fatty degeneration and absorption which normally occur after the expulsion of the product of conception, and which are essential for the restoration of the uterus to its normal size. The elements of the endometrium and the vascular system of the uterus also remain hypertrophied; consequently the uterus is larger, heavier, more congested than normal.
Similar arrest of involution may occur coincidently in the ligaments of the uterus, which are left larger, longer, and more relaxed than in the normal condition.
The pathological changes that occur in the subinvoluted uterus are similar to those found in chronic endometritis and metritis, which have already been described. In fact, chronic endometritis and metritis accompany subinvolution from the beginning.
There are many causes of subinvolution of the uterus. Too early rising from bed is a most frequent cause. This is especially true after abortion or miscarriage; for many women treat such occurrences as of but little moment, and refuse to stay in bed for more than a few days.
Imperfect evacuation of the uterus after abortion or miscarriage is a common cause. Laceration of the cervix, 216 retrodisplacement of the uterus, and laceration of the perineum are all causes of subinvolution of the uterus.
The symptoms of subinvolution are the same as those already described under Chronic Metritis—backache, headache, bearing-down pain in the pelvis, general physical debility, leucorrhea, and menorrhagia.
The treatment of subinvolution should be directed toward the relief of the primary cause of the condition. Laceration of the perineum or of the cervix, retroversion, or endometritis caused by retention of placental tissue after miscarriage, should receive appropriate treatment.
Subinvolution may often be cured by the douches, iodine applications, and depletion of the cervix spoken of under the treatment of laceration of the cervix, provided the primary cause is removed or corrected.
In any case the cure is always hastened by thorough curetting of the uterus. This operation should always be performed when the woman is etherized for the relief of any other condition, as a laceration of the cervix or of the perineum.
The cure of subinvolution depends a great deal upon the time that has elapsed from the inception of the condition to the institution of treatment. The secondary changes in the endometrium and body of the uterus resulting from chronic congestion and inflammation in time becomes so established that the disease will not yield to any treatment, even though the primary cause of the trouble may be cured.
In obstinate chronic cases of subinvolution of the uterus amputation of the cervix sometimes has a most marked effect, and this operation should always be resorted to whenever the disease has resisted the milder treatment already prescribed. Amputation of the cervix is sometimes followed by a transformation of all the tissues of the uterus similar to that occurring in normal involution after labor, and a striking diminution in the size of the uterine body takes place. The amputation of the cervix should always be accompanied by a thorough 217 curetting. Sometimes the change in the body of the uterus is so marked after amputation of the cervix, or even after trachelorrhaphy, that a condition of superinvolution, or uterine atrophy, results.
Superinvolution of the uterus is a disease the reverse of subinvolution. In this condition the uterus, after childbirth or abortion, not only undergoes the normal involution, but continues to atrophy until the length of the uterine cavity may measure but one and a half inches. The atrophy involves the neck as well as the body of the organ, the Fallopian tubes, and sometimes the ovaries.
Superinvolution of the uterus is a rare condition. The cause is difficult to determine. It has been attributed to great loss of blood at confinement, to prolonged lactation, and to pelvic peritonitis occurring during the puerperium.
Amenorrhea is the most marked symptom of superinvolution. Nervous disturbances and hysterical symptoms may also be present.
The diagnosis is easily made from the history of the case and by means of bimanual examination and the use of the sound. Congenital malformation may be excluded from the fact that a pregnancy has occurred, and senile atrophy from a consideration of the age and history of the woman. The treatment should be directed to restoring and maintaining the general health of the woman.
Iron and the remedies useful in other forms of amenorrhea may be of advantage. 218
Cancer of the body of the uterus is a rare disease in comparison with cancer of the cervix. The older statistics—those of Schroeder—appear to show that the disease begins in the body of the uterus in about 2 per cent. of all cases of cancer of this organ. This percentage, however, is probably too small. Cancer of the body of the uterus is by no means an infrequent disease; it is a disease for which the physician should always be on the watch.
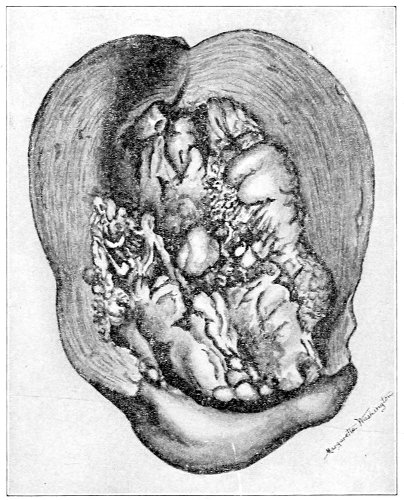
Fig. 125.—Diffuse cancer of the endometrium.] 219
Cancer of the body of the uterus originates in the epithelial structures of the endometrium. It may first appear on the surface of the endometrium or deeply in the utricular glands.
The gross appearance of the disease varies as does cancer of the cervix or of any other part of the body.
Cancer of the uterus may begin upon the surface of the endometrium as a superficial ulceration, as a uniform swelling of the mucous membrane, as a polypoid or papillary projection, or as a large cauliflower-like mass projecting into the uterine cavity.
When the disease begins in the utricular glands, it may form nodules throughout the body of the uterus. These nodules are of various sizes, from that of a pea to that of a hen’s egg. They grow rapidly. They may be submucous and project into the uterine cavity, or they may project beneath the peritoneal covering, giving the uterus an irregular nodular appearance (Fig. 126).
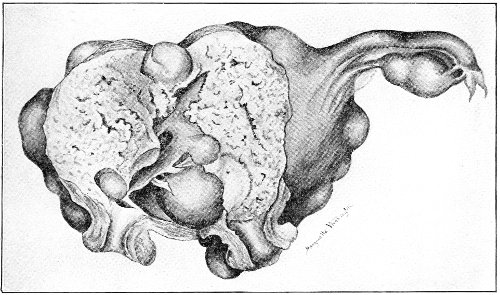
Fig. 126.—Nodular form of cancer of the body of the uterus.
In the later stages of the disease the whole body of the uterus becomes infiltrated. The endometrium is destroyed. The cancerous masses ulcerate and break down. The peritoneal covering is for a certain time a barrier to the extension of the disease. In many cases 220 the whole of the body of the uterus may be infiltrated with cancer, and yet the peritoneum will remain intact. The accompanying illustration (Fig. 127) shows this: the infiltration extends to, but does not involve, the peritoneum.
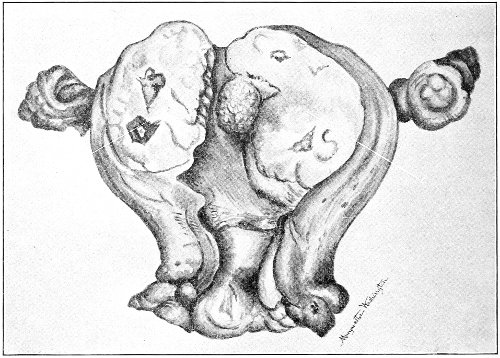
Fig. 127.—Cancer of the body of the uterus: a large single cancerous nodule (c) in the anterior wall has been divided.
Later, however, the peritoneum, the Fallopian tubes, and the ovaries become involved. Intestinal adhesions are formed, and the disease may extend throughout the abdominal cavity. The cervix and the vagina may be attacked by extension from above, though, on the other hand, the disease may progress sufficiently to destroy life, and yet the cervix may remain unaffected.
Metastasis may take place by way of the lymphatics. Extension by metastasis, however, is unusual.
Cancer of the body of the uterus occurs at a somewhat later age than cancer of the cervix. The average age is between fifty and sixty. The disease attacks both the parous and nulliparous woman, the latter perhaps more often than the former. 221
The causes of cancer of the body of the uterus are unknown. It is probable that the various forms of endometritis, by diminishing the resistance of the endometrium, predispose to the development of cancer. It has been maintained that fibroid tumors of the uterus, as a result of the accompanying alterations in the endometrium, predispose to cancer. Cancer of the endometrium is certainly not infrequently found in uteri containing fibroid tumors.
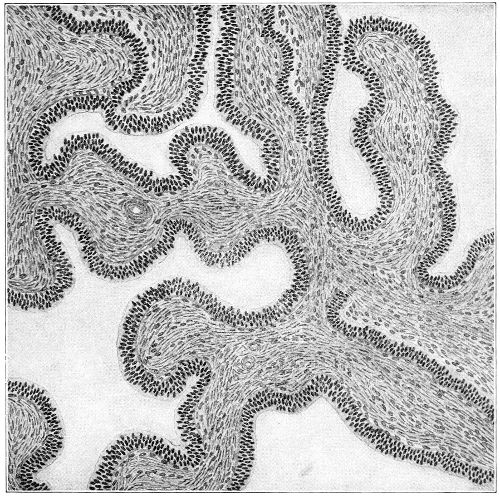
Fig. 128.—Malignant adenoma of the body of the uterus (Beyea).
Malignant adenoma is a disease of the utricular glands which has been classed by some writers as a distinct disease, by others as a form of carcinoma. In it the gland-spaces are much enlarged, irregular, and joined to other gland-spaces. The columnar epithelial cells often fill the whole of the gland-space (Fig. 128) The cells, 222 however, never infiltrate the interstitial tissue, as in cancer. The muscular wall of the uterus appears to be destroyed by atrophy or by fatty degeneration.
The disease is malignant, it extends to the neighboring structures, and it destroys life. It presents, in the later stages, all the gross appearances and phenomena of cancer.
The symptoms of cancer of the fundus are hemorrhage, leucorrheal discharge, and pain.
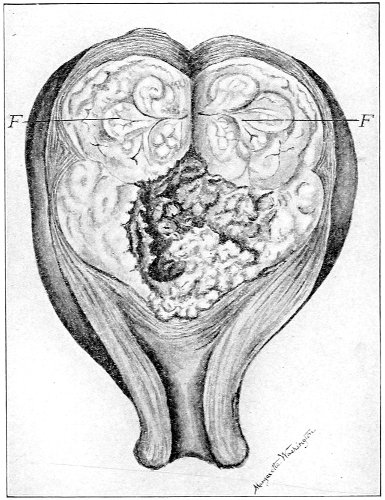
Fig. 129.—Advanced malignant adenoma of the body of the uterus. A fibroid tumor (F) is in the fundus.
In women before the time of the menopause the hemorrhage may appear as a menorrhagia or a metrorrhagia, as an increase of the normal menstrual bleeding, or as a bleeding occurring at some other time than the normal menstrual period. Such irregular bleeding may be caused by any unusual effort.
After the menopause the hemorrhage may appear as a 223 return of menstruation, occurring with more or less periodicity, and, as in cancer of the cervix, often contemplated with satisfaction by the woman. It may appear as a slight occasional discharge of blood, as a bloody streak in the leucorrheal discharge, as a spot upon the clothing, or as continuous hemorrhage. In the late stages of the disease there is a continuous discharge of blood.
The leucorrheal discharge at first resembles that of a non-malignant endometritis. It often begins as a gradual increase of a leucorrhea which the woman may have had for several years. It may be streaked with blood. In the early stages there is nothing at all characteristic about the discharge; later, however, it usually becomes very offensive, on account of the breaking down of necrotic tissue. It becomes more purulent in character, and brown in color from the presence of blood. In some cases of cancer of the fundus, however, the leucorrheal discharge remains light-colored and practically odorless throughout the whole course of the disease. It is sometimes thin and watery and exceedingly profuse, saturating many napkins during the day.
The pain of cancer of the fundus is not a marked symptom. It may be absent even though the whole body of the uterus be involved by the disease. When the peritoneum is affected, and extension takes place to other pelvic structures, the pain is much more pronounced. In other cases the pain may be present in the early stages, before the disease has extended beyond the endometrium.
The pain may be referred to the region of the uterus, to the back, or sometimes to parts of the pelvis remote from the uterus, as the crest of the ilium.
Bimanual examination shows a patulous external os, cervical canal, and internal os. As has already been said, this patulous condition is characteristic of gross disease of the endometrium.
The body of the uterus is usually somewhat enlarged, 224 tender on pressure between the vaginal finger and the abdominal hand, and, in the late stages of the nodular form of cancer, irregular in outline.
The causes of death in cancer of the fundus uteri are the same as those that have already been considered in cancer of the cervix. Extension to abdominal organs is, however, more frequent in cancer of the fundus.
Diagnosis.—It is of the greatest importance to make an early diagnosis of cancer of the fundus uteri, because, of all parts of the body that may be attacked by malignant disease, the fundus uteri offers the best prospect of cure by operation. In the early stages the disease can easily be completely removed.
Hemorrhage from the uterus is the universal symptom, and should never be disregarded. The various manifestations of hemorrhage in cancer of the fundus should always be borne in mind, and should always prompt a thorough investigation.
Leucorrheal discharge occurring at or after the menopause, in a woman previously free from such discharge, should also excite suspicion.
If a careful examination of the cervix fails to reveal any cause for the hemorrhage or the discharge, the interior of the uterus should be thoroughly examined by the curette.
A patulous cervical canal and internal os are good indications that there is some gross disease of the endometrium. In cancer of the fundus the cervical canal and the internal os are usually sufficiently open to permit thorough curetting without further dilatation.
The Sims sharp curette may be used with safety if ordinary care be observed. If the woman is nervous, an anesthetic should be administered, though in most cases diagnostic curetting gives but little pain and may be performed without ether.
The operator should not be content with the removal of a few strips or portions of the endometrium. He should remember that in the early stages the disease may be confined to a small area, and, unless the whole interior 225 of the uterus is gone over, this area may be missed by the curette, and only healthy endometrium may be removed for examination. Such thorough curetting is of especial importance in case the tissue removed should at first present no suspicious features upon gross examination. All portions of the endometrium should be saved and preserved as directed in cancer of the cervix.
The tissue should be submitted for examination to a person trained in gynecological pathology. The recognition of the early stages of cancer of the endometrium, and especially of malignant adenoma, requires the training of the expert. If a positive diagnosis cannot be given from the microscopic examination, the case should be carefully watched, and if the symptoms continue, subsequent curetting and microscopic examination should be made.
The treatment of cancer of the fundus is immediate complete hysterectomy, with removal of the tubes and ovaries. Cancer has recurred in an ovary after removal of the uterus. The hysterectomy may be performed by the vaginal, the abdominal, or the combined method.
The ultimate results of hysterectomy for cancer of the body of the uterus are exceedingly good. Statistics show about 75 per cent. of permanent cures. Recurrence may be considered exceptional. In this respect they are in marked contrast to the results after operation for cancer of the cervix.
Sarcoma of the uterus is a very rare disease. There have been but few properly authenticated cases of this disease reported in medical literature. All cases of this disease should be put on record.
There are two varieties of sarcoma of the uterus: diffuse sarcoma of the mucous membrane, and sarcoma of the uterine parenchyma.
In diffuse sarcoma of the mucous membrane the endometrium is infiltrated by round or spindle cells. 226 Soft projections or tumors, which may be villous, lobulated, or polypoid in shape, are formed upon the mucous membrane.
The polypoid sarcoma may present at the cervix uteri. The disease extends to the muscular coat of the uterus.
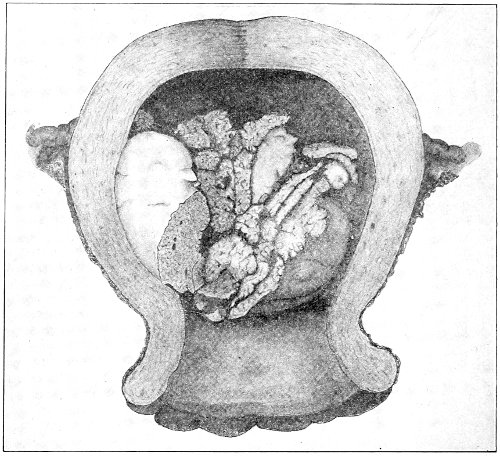
Fig. 130.—Diffuse sarcoma of the mucous membrane of the uterus.
In the later stages ulceration and disintegration of tissue occur.
The cervix is not involved by the disease.
The symptoms of this form of sarcoma resemble those of cancer of the fundus. There are hemorrhage, discharge, and pain.
The discharge is serous, and is less fetid than in cancer, as ulceration takes place later in the course of the disease.
The cervical canal is patulous, and in the polypoid form the tumor may be felt projecting into the cavity of the uterus or protruding from the external os.
The fundus uteri is enlarged and is tender upon pressure. 227 A positive diagnosis can be made only by microscopic examination of curetted or excised tissue.
Sarcoma of the uterine parenchyma, or fibro-sarcoma, or recurrent fibroid, begins in the muscular coat of the uterus. It appears as nodules of various size, which may be interstitial or confined to the muscular coat, submucous or projecting beneath the mucous membrane, or subperitoneal, projecting beneath the peritoneal coat. On section these nodules are pale in appearance and soft in consistency. They are rarely found in the cervix. The submucous form of nodule may become polypoid, project into the cavity of the uterus, and with comparative frequency produce inversion of the uterus.
The nodules of sarcoma differ from those of benign fibroid tumors in the fact that they have no capsule. They cannot be enucleated, but are intimately connected with the surrounding uterine tissue. Metastatic nodules occur in the vagina, the peritoneum, and in other parts of the body.
In the later stages of the disease the nodules disintegrate and break down.
It is probable that fibro-sarcoma usually, if not always, originates in a benign fibroid tumor. In the early stage of the disease the microscopic appearances of fibroid tumor are present, and the transition from the benign to the malignant growth may be studied.
Symptoms.—The symptoms of this form of sarcoma resemble at first those of fibroid tumor; they are—hemorrhage in the form of menorrhagia; a serous, non-odorous discharge; and a moderate degree of pain.
Later, when ulceration and disintegration take place, the hemorrhage becomes more profuse and continuous. The discharge becomes fetid, and contains broken-down sarcomatous tissue. The pain becomes more severe. The uterus is enlarged, and the nodular outline may be determined by palpation.
Before metastasis has taken place the differential diagnosis between sarcoma and benign fibroid tumor can be 228 made only by microscopic examination of the discharge or of curetted or excised portions of tissue. The duration of sarcoma of the uterus is about three years.
Sarcoma may occur at almost any age. Hysterectomy has been performed for this disease in a girl of thirteen. Several cases have been reported under twenty years of age. The most usual period is about the time of the menopause, in the decade from forty to fifty.
The treatment of sarcoma of the uterus is immediate complete hysterectomy. If in the early stage a positive diagnosis cannot be made between benign fibroid and sarcoma, the woman should not be exposed to the dangers of waiting, but the uterus should be immediately removed.
Chorio-epithelioma or syncytioma malignum is a rare and peculiar malignant growth of the uterus which occurs after pregnancy. It originates at the placental site from the epithelial cells covering the chorionic villi. It occurs during the course or after the termination of a uterine or tubal pregnancy. In typical cases the disease immediately follows labor at term, abortion, or a destroyed extra-uterine pregnancy. It may, however, remain latent for weeks or months.
The tumor may be a nodular or pedunculated outgrowth attached to the uterine wall; a fungoid growth from the endometrium; or an intramural growth covered with endometrium. The tumor varies in size from that of a cherry-stone to a mass several inches in diameter. It is composed of soft fragile spongy tissue, light or dark red in color, infiltrated with blood, and containing circumscribed hemorrhages. Histologically the tumor consists of many types of cells irregularly placed; syncytial tissue, cells derived from Langhans’ layer, and sometimes chorionic connective tissue. There are numerous cavities containing blood and connective tissue.
Metastatic growths have a similar structure. Metastasis takes place through the vascular system and may reach distant organs—the lungs, liver, and spleen. 229
Symptoms.—There is no characteristic symptom of chorio-epithelioma. The chief symptom is irregular or continuous hemorrhage from the uterus following a labor, an abortion, or an extra-uterine pregnancy. The body of the uterus is enlarged, and the cervical canal dilated as in cancer and sarcoma. A positive diagnosis can be made only by microscopic examination of tissue removed by the curet.
Treatment.—As the disease is exceedingly malignant and of rapid growth, immediate hysterectomy is indicated. 230
Fibroid tumors originate in the muscular wall of the uterus. They are composed of elements resembling, to a greater or less extent, those that compose the middle uterine wall. They consist of connective tissue and of unstriped muscular tissue in varying proportions. Uterine tumors composed exclusively of muscular fibres—true myomata—very rarely occur.
A number of names, based upon the proportion of the component elements, have been used by writers to designate these tumors. They have been called fibroma, myoma, myo-fibroma, and fibro-myoma. The natural history of all the varieties is about the same, and varies but little with the proportion of the elements. I shall therefore consider them under the general name of fibroid tumors of the uterus.
Fibroid tumors of the uterus are benign, in the sense that they do not, like cancer, infiltrate contiguous structures or infect the general system.
Fibroid tumors are loosely attached to the surrounding uterine wall. They are usually invested by loose cellular tissue, forming a capsule from which they may easily be enucleated. Blood-vessels, usually of small size, connect the tumor with its capsule. Dense adhesion between the tumor and its capsule is the result of inflammatory action. The loose connection of the fibroid tumor with the surrounding structures explains the ease with which these tumors travel and are squeezed out of the uterine 231 232 wall. It will be remembered that in this respect the fibroid differs from the nodule of cancer and of sarcoma.
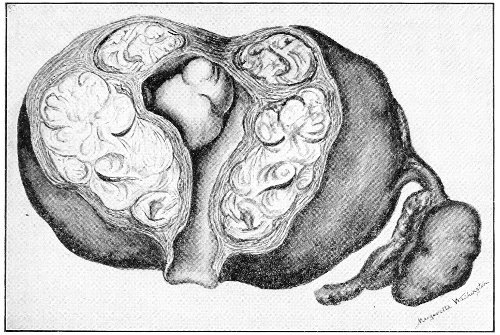
Fig. 131.—Interstitial fibroid tumor of the uterus. A small submucous fibroid appears in the uterine cavity.
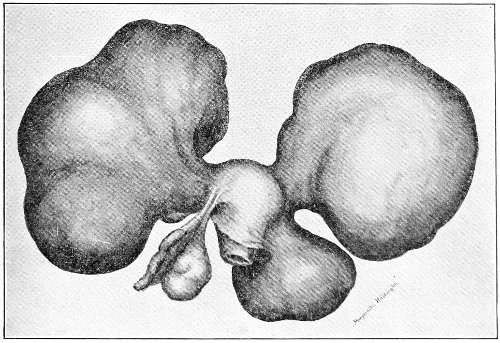
Fig. 132.—Subperitoneal fibroid tumors of the uterus.
To the naked eye fibroid tumors present a white or rosy appearance. The intensity of the red color is, as a rule, proportional to the amount of muscular tissue. On section the bundles of fibrous tissue, arranged more or less concentrically about many axes, may be apparent. The vessels in the tumor itself are usually small and few in number. The large arteries and venous sinuses are found in the capsule.
Fibroid tumors vary in hardness from the soft myoma to dense stony nodules composed almost entirely of fibroid tissue.
Fibroid tumors vary in size from the smallest nodule in the uterine wall to a solid mass weighing one hundred and forty pounds. The tumors that usually come under observation weigh from one to ten pounds.
Fibroid tumors occur most frequently in the body of the uterus. As has already been mentioned, however, they are sometimes found in the infra-vaginal portion of the cervix, and a peculiarly dangerous form of fibroid grows from the supra-vaginal cervix.
Fibroid tumors are multiple in the great majority of cases. It is unusual to find a single fibroid nodule or tumor in the uterus. Sometimes one tumor far outgrows the rest, but if the uterine wall is carefully examined other small nodules will usually be found in its substance.
Fibroid tumors originate in the muscular wall of the uterus, and extend thence in various directions. When they are situated in the muscular wall they are said to be interstitial (Fig. 131). When they grow outward, so that they project beneath the peritoneum, they are called subperitoneal (Fig. 132). When they project into the uterine cavity they are called submucous (see Fig. 131).
When they grow from the side of the uterus, and especially from the supra-vaginal portion of the cervix, and extend outward into the cellular tissue between the folds 233 of the broad ligaments, they are said to be intra-ligamentous (Fig. 133).
The subperitoneal fibroid may continue to grow, pushing the peritoneum ahead of it, until the tumor becomes altogether extruded from the body of the uterus. It is then attached to the uterus only by a pedicle of varying thickness. The pedicle may be fibro-muscular in character, or it may consist only of peritoneum, a little muscular tissue, and blood-vessels.
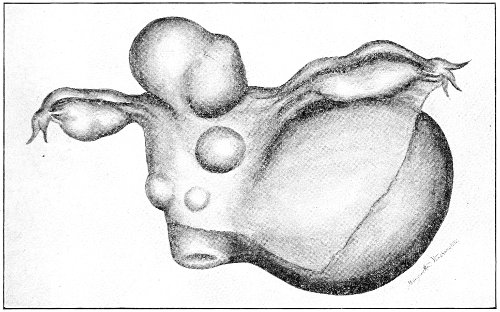
Fig. 133.—Subperitoneal fibroids and an intra-ligamentous fibroid of the uterus.
Such a hard, freely movable tumor often causes a great deal of peritoneal irritation. A serous fluid may be thrown out by the peritoneum, and a moderate degree of ascites may occur. Adhesions may be formed between the fibroid tumor and contiguous structures—the abdominal parietes, the omentum, or intestines. These adhesions are often exceedingly extensive, firm, and vascular, so that in some cases the tumor derives its chief blood-supply and mechanical support from such adventitious attachments. The uterine pedicle may, as a result of progressive atrophy, traction, or violence from a fall, become detached, and the tumor, having then lost all uterine connection, appears to be a fibroid growth of the 234 omentum, intestine, or abdominal wall. This is the origin of many so-called fibroid tumors of these structures.
Detachment from the uterus may also occur, as the result of atrophy of the pedicle or of violence, in the case of a pediculated subperitoneal fibroid that has not contracted adhesions to other structures, and the tumor will then be found free in the abdominal cavity.
The subperitoneal fibroid in its upward growth sometimes drags the body of the uterus with it, and in this way may produce great elongation and distortion of the cervix.
The submucous fibroid grows toward the uterine cavity. It presses the mucous membrane before it, and it may enter the cavity of the uterus, being altogether extruded from the uterine wall. It then forms a pediculated tumor lying in the uterus—an intra-uterine polyp. The pedicle is composed of dense fibro-muscular tissue, and is invested by a sheath of mucous membrane, unless this structure has been destroyed. The pedicle may be but slightly vascular, or it may rarely contain large arteries. As a general rule, the greater the degree of the extrusion of the polyp and the longer the pedicle, the less is the vascular supply. Rapid spontaneous hemostasis occurs after a fibroid polyp is cut from its pedicle, as a result of the thickness of the arterial walls and the contractility of the pedicle.
The intra-uterine polyp, from prolonged pressure, sometimes acquires the shape of the uterine cavity.
Uterine contractions are excited by the presence of the polyp, and the tumor may in time be expelled from the uterus, enter the vagina, and protrude at the vulva.
Submucous fibroids form the most usual variety of uterine polypi. In some cases the overlying mucous membrane becomes much stretched and attenuated, and may finally rupture or slough. The fibroid tumor may then escape through the opening in the mucous membrane, and, having been extruded altogether from the 235 uterine wall, may be expelled from the body by uterine contractions.
The fibroid polyp, being exposed to septic influences from the vagina, may become inflamed and suppurate; or sloughing and disintegration may occur because of interference with the blood-supply in the pedicle.
The intra-ligamentous fibroid grows from the side of the uterus or from the supra-vaginal cervix. It pushes apart the peritoneal folds of the broad ligament, and grows between them or beneath them. The tumor is thus outside of the peritoneum. It may fill the whole pelvis with a dense unyielding mass, pushing the uterus to the pelvic wall, destroying anatomical relations, and exerting most disastrous pressure upon blood-vessels, nerves, ureters, and other pelvic structures.
Sometimes, as these tumors enlarge in an upward direction, they carry with them overlying pelvic organs; thus the ureter may be found passing over the top of a tumor which, beginning as an intra-ligamentous pelvic growth, has become abdominal.
In some cases the fibroid grows from the posterior aspect of the supra-vaginal cervix, passes beneath the bottom of Douglas’s pouch, pushes the peritoneum above it, and becomes a retro-peritoneal tumor.
Again, it may grow from the anterior aspect of the cervix in the vesico-uterine space, and as it extends upward may push the vesico-uterine fold of peritoneum above it and drag up the bladder, so that this viscus is sometimes found spread out upon the anterior face of the tumor and extending as high as the umbilicus.
As has already been said, fibroid tumors are usually multiple, and if one of the terms designating the position of the tumor as subperitoneal or intra-ligamentous is used to describe any case, we understand that the chief tumor-mass is of this character.
The fibroid polyp is more likely to be single than any of the other varieties. In fact, the fibroid polyp is usually single; that is, no other fibroid tumor can be detected 236 in the body of the uterus. This is not always the case, however, and sometimes the repeated expulsion of successive fibroid polypi from the same woman renders it probable that several nodules were simultaneously present in the uterine wall.
As a rule, fibroid tumors of the uterus are of slow growth. In some cases five, ten, or fifteen years may elapse before the tumor attains the size of the fetal or the adult head. Sometimes the tumor appears to be of limited growth, and early attains its maximum size, or it may not increase at all in size after its first discovery by the woman; in other cases the tumor slowly but steadily grows until, after a lapse of ten or twenty years, it fills the whole of the abdominal cavity and renders the woman helpless from weight and pressure; and, finally, in some instances the tumor grows unlimitedly with the rapidity characteristic of an ovarian cyst, and in one or two years may crowd the woman out of existence. This rapid unlimited growth is characteristic of tumors of the fibro-cystic variety.
A fibroid tumor causes very marked changes in the body of the uterus—the muscular coat and the endometrium. The whole uterus becomes enlarged. The cavity is increased in length, and the muscular wall becomes often very much hypertrophied. This hypertrophy resembles that occurring in pregnancy. Even small fibroid tumors may produce this condition, which seems to depend more upon the position than upon the size of the growth. The interstitial and the submucous tumors are accompanied by a greater degree of uterine hypertrophy than accompanies the subperitoneal growths. In some cases the uterus may be of normal size if the subperitoneal growth has become pedunculated. The uterus may appear to be uniformly enlarged to the size of the fourth or fifth month of pregnancy, and when incised it will be found to contain one or more interstitial or subperitoneal tumors that have become encapsulated by it. When such a case is subjected to celiotomy the resemblance of the 237 uterus to pregnancy is very striking. Between such a smooth, uniformly enlarged uterus on the one hand, and the irregular, distorted mass of subperitoneal fibroids on the other, there are an infinite number of varieties. A great increase in the vascular supply accompanies the hypertrophy of the uterus. The ovarian and uterine arteries and their branches become very much hypertrophied, while the veins in the broad ligaments and the sinuses in the capsule of the tumor become enormous.
The endometrium shares in the changes that take place in the uterus. It is, of course, increased in area with the increase of the uterine cavity. There may be atrophic changes from pressure upon or tension of this membrane, or various forms of endometritis may be present, most usually the interstitial and the glandular. The glandular form of the disease is said to occur most frequently when the tumor is remote from the cavity of the uterus, as in the subperitoneal variety; while interstitial endometritis occurs with the submucous and the interstitial tumors.
In the Fallopian tubes and the ovaries pathological changes occur as the result of uterine fibroids. The tubes may present any of the forms of cystic change—hydrosalpinx, pyosalpinx, or hematosalpinx—that are caused by salpingitis. It is probable that these diseases are often caused by extension of endometritis. The tubes and ovaries may be much distorted and displaced from the normal position. In some cases the ovary is drawn out into a long cord five inches in length; in other cases it is spread out upon the face of the tumor.
Fibroid tumors are liable to several forms of degeneration—calcareous, fatty, myxomatous, edematous, cystic, telangiectatic, gangrenous or suppurative, necrobiotic, and malignant.
Calcareous change, from the deposit of lime-salts in the fibroid nodules, is an unusual occurrence. It appears most often in women beyond the menopause, and is part of the atrophic changes that take place at this time. (It 238 has occurred in a woman who had been subjected to oöphorectomy for the relief of a fibroid tumor.)
I have seen a fibroid tumor the size of the adult head—a solid calcareous mass which could be divided only by means of a saw.
The calcareous nodules are surrounded by uterine tissue to which they are but loosely attached. They may be forced out of the uterus and escape at the vulva. They have been called “womb-stones.”
Fatty degeneration is a very unusual condition. It has been assumed to take place, as a step preliminary to absorption, in those cases in which a fibroid tumor disappears after labor or from other cause.
Myxomatous degeneration is also rare. In it an effusion of mucous fluid takes place between the bundles of fibrous tissue. Sometimes large cavities are formed in this way.
In the edematous fibroid the whole tumor is permeated by a serous fluid. This condition is not unusual. It resembles edema in any other part of the body. It is often found in young women before the thirtieth year.
Cystic degeneration of fibroid tumors may result from any of the forms of degeneration with softening in which cystic cavities are formed.
In some cases fibro-cystic tumors are caused by dilatation of the lymphatics. They have been called “lymphangiectatic fibroids.” An endothelial lining has occasionally been found in the cystic cavities of these tumors. The fluid removed from the cyst-cavities coagulates spontaneously. Such fibroids have frequently been mistaken for ovarian cysts.
In the telangiectatic or the cavernous form of fibroid tumor there is an enormous dilatation of the vessels in the new growth. The venous spaces are sometimes as large as a walnut, and are filled with clotted or fluid blood. This change usually affects one part, and not all, of the tumor, which presents the gross appearance of a sponge soaked with blood. 239
Gangrene is most liable to occur in the fibroid polyp. During the process of expulsion from the uterus the vascular supply through the pedicle becomes impeded, so that there is not sufficient blood for nutrition. The tumor is exposed to septic infection through the vagina and the cervix, and sloughing and suppuration occur. As a result of such disintegration the tumor may be discharged piecemeal.
Inflammation, and occasionally suppuration, of fibroid tumors remote from the cavity of the uterus may occur from infection through the intestinal tract or other channel.
Necrobiosis occurs if the nutrition of the fibroid is cut off and there is no infection of the dead tissue. The tumor becomes soft, undergoes fatty degeneration, and liquefies. The necrobiotic degeneration may involve only part or all of the tumor. There is always danger of septic infection occurring in this form of degeneration.
Sarcoma may develop in a fibroid tumor of the uterus. As has already been stated, the “circumscribed fibroid sarcoma,” or sarcoma of the uterine parenchyma, is thought by some authorities always to originate from degeneration of a benign fibroid tumor. It seems probable that the fibroid tumor predisposes the woman to the development of sarcoma of the uterus.
Cancer may also occur in the endometrium of a fibroid uterus. This occurrence is by no means an unusual one. We cannot yet say positively that the fibroid favors the development of cancer, but it seems probable that the diseased endometrium that accompanies fibroids furnishes a place of diminished resistance for the development of malignant disease.
Martin has made an interesting analysis of 205 cases of fibroid tumor of the uterus that had been submitted to operation. From this analysis we may form some estimation of the frequency of the various forms of degeneration that have been described. 240
Fatty degeneration existed in 7 cases. Calcification was present in 3 cases. In 10 cases there was suppuration, and this process was found in the submucous, interstitial, and subperitoneal tumors. In 11 cases there was extensive edema of the fibroid. In 8 cases the tumors had become cystic.
The telangiectatic change was found to a marked degree in 3 cases.
Sarcomatous degeneration had occurred in 6 cases.
In 7 cases the fibroid was complicated with cancer of the fundus uteri, and in 2 cases with cancer of the neck of the womb.
The fatty and calcareous changes are not to be considered dangerous forms of degeneration.
The other changes, however, are often attended with great danger to life. The dangers of suppuration and of sarcomatous degeneration are obvious. The edematous fibroid is often of rapid and unlimited growth, and is usually accompanied by profuse hemorrhages from the uterus. The cystic fibroid may grow as rapidly and as large as an ovarian cyst. The telangiectatic tumors grow to large size and are attended by the dangers of thrombosis and embolism.
Cancer of the fundus with fibroid tumor may only be a coincidence, and we will not assume that predisposition to cancer is caused by the fibroid.
The statistics that have been given, however, show that in at least 38 cases out of 205, or in about 18 per cent. of the cases, changes took place in the fibroid that seriously endangered the life of the woman.
Sterility, abortion, and difficult or impossible labor are caused by uterine fibroids. Conception is impeded on account of the displaced, distorted uterus and the hemorrhage and discharge. Abortion is likely to occur, on account of the endometritis and the unequal expansibility and the irritability of the uterus.
Labor is sometimes rendered impossible by the presence 241 of a uterine fibroid that obstructs the pelvis, and Cesarean section has been performed for this cause.
The cause of fibroid tumor of the uterus is unknown. Some authorities consider the condition, or at least the predisposition to the condition, to be congenital. Uterine fibroids have been observed in girls near the age of puberty, and hysterectomy for fibroid has been performed at the age of eighteen.
Usually the disease begins to cause symptoms, and first comes under the observation of the physician, after the thirtieth year. It is very probable that small interstitial or subperitoneal fibroids exist in many women before this period, but, on account of the small size and the position of the growths, they produce no marked symptoms, and if the woman bears children, the tumors are very likely absorbed during the process of uterine involution.
Fibroid tumors occur in both the white and the black races—with somewhat greater frequency in the latter than in the former. Tait says that fibroid tumors of the uterus are unknown among the black women of Africa. The disease is certainly very common among their descendants in this country.
The frequency of uterine fibroids is difficult to determine, for there are many cases in which the disease is unrecognized on account of the small size of the tumor and the absence of symptoms. It is, however, one of the commonest diseases with which women suffer. In a series of 504 celiotomies performed for diseases of women at the University and Gynecean Hospitals, uterine fibroids were found in 85, or in about 17 per cent. of the cases.
Fibroid tumors are found both in multiparous and in nulliparous women—much more frequently in the latter than in the former. Single women and sterile married women are especially predisposed to this disease. There are two probable causes for this difference. The unceasing congestions of menstruation favor the development 242 of the neoplasm; and, when once started, its further growth is not checked by the retrograde changes that accompany involution of the uterus, and that sometimes cause the disappearance of even large fibroids.
Fibroid tumors are essentially growths of the menstrual life of the woman. They usually first appear after the thirtieth year, and they continue to grow until the menopause. The size of the tumor and the severity of all the symptoms progressively increase during the active sexual period of life. It is very unusual for favorable retrograde changes or permanent amelioration of symptoms to occur during this period. In a woman with fibroid tumor of the uterus the menopause is delayed for five to fifteen years beyond the normal time. This is an important fact to be remembered in connection with the prognosis and the treatment of any case.
At the menopause, in the majority of cases, the growth of the tumor is arrested, and the retrograde changes that affect the genital apparatus involve also the fibroid tumor, and atrophy of the neoplasm, with marked diminution in size, and in some cases its complete disappearance, may take place. The tumor becomes quiescent, and the woman may finish her life in comparative comfort. This, however, is by no means always the case. The fibroid sometimes continues to grow after the menopause, and the suffering is sometimes so unbearable that the woman is finally driven to operation.
In some cases the tumor has developed entirely after the menopause has been reached.
At each menstrual period there is usually a decided increase in the size of the tumor and in the severity of the symptoms. And at these periods, in the case of a submucous or an interstitial fibroid, the cervical canal becomes more patulous.
Symptoms.—The chief symptom of fibroid tumor of the uterus is hemorrhage. This symptom is present in the great majority of fibroids of all kinds. It is not, 243 however, universally present. I have removed tumors the size of the adult head, composed of interstitial and subperitoneal fibroids, from women who had never suffered with even slight menorrhagia. The hemorrhage appears in the form of menorrhagia or metrorrhagia. It may be an increase in the regular menstrual bleeding. It may appear as a periodical bleeding occurring every two weeks—a phenomenon that occurs in other diseases of the uterus and the endometrium. It may appear as a show of blood or a slight hemorrhage, after unwonted effort, between the regular menstrual periods. This may occur after straining at stool, coitus, or even emotional disturbance. And, finally, it may appear as a continuous bleeding from the uterus.
The cause of these hemorrhages is to be found in the increased area of the endometrium accompanying the uterine enlargement, and in the diseased condition of the endometrium.
The hemorrhage is not usually alarming in amount, and it may be somewhat controlled by rest in bed and the administration of ergot or other drugs. In some cases, however, it produces the most profound anemia, and in others, especially in the uterine polyp, the woman may literally bleed to death.
The symptom of hemorrhage is independent of the size of the tumor, but depends upon the position of the fibroid. As a rule, the hemorrhage is most severe with the uterine polyp, less severe with the submucous and the interstitial tumors, and least with the subperitoneal variety. In some cases, when the mucous membrane overlying a submucous tumor ruptures, the hemorrhage may come directly from venous sinuses in the capsule.
The hemorrhage also depends upon the variety of the growth. The edematous fibroid and the soft myoma appear always to be accompanied by profuse bleeding. In some cases the hemorrhage may occur periodically or continuously in old women who have passed the menopause, 244 and in whom there had been no bleeding for several years. This has been observed in the small submucous fibroids which, after a period of quiescence, have gradually become polypoid, or which have undergone suppuration and disintegration. The hemorrhage, the offensive odor of the discharge, and the age and the history of the patient are very likely to lead to the diagnosis of cancer.
The blood that escapes from the fibroid uterus may be fluid or clotted, or it may be partly decomposed from the retention of clots.
A profuse secretion from the utricular glands often occurs between the uterine hemorrhages. This secretion is usually thin and watery in character, and may be so profuse as to require the continuous wearing of a napkin. In some unusual cases there is no marked hemorrhage, but a continuous abundant watery discharge.
Pain is a more or less constant accompaniment of fibroid tumors. It varies a great deal in character and position. It is often referred to the sacrum and to the top of the head or the occiput. Pain of this character is due to the accompanying metritis and endometritis. That it is uterine in origin is shown by the fact of its complete and permanent disappearance from the day that hysterectomy is performed.
The pain is always increased at the menstrual periods, and may at first be present only at these times. It afterwards becomes continuous.
In the case of a submucous or a polypoid fibroid there may be present the pain of uterine contractions, referred to the center of the lower abdomen, and resembling labor-pains.
The pain from pressure is sometimes intense. It occurs in large tumors and in those of pelvic growth, like the intra-ligamentous fibroids. Sciatic or crural neuralgia may be thus developed.
In all these cases there is a feeling of weight and dragging 245 in the pelvis which is most marked in the erect position, and which is caused by the weight of the tumor and of the enlarged uterus.
The symptoms of pressure are very marked in the case of intra-ligamentous tumors. The capacity of the bladder may be so diminished that there may be continuous incontinence of urine; or the bladder and the urethra may be so distorted, from traction and pressure, that urine is voided with great difficulty, and it is sometimes impossible to introduce the catheter. I have seen a woman with a fibroid the size of the adult head who could urinate only when upon her hands and knees.
Pressure upon the pelvic nerves may, as has already been mentioned, produce great pain, and in some cases paralysis. Women are sometimes affected with sudden complete paralysis of one or both legs from the pressure of a fibroid. I have performed hysterectomy upon a woman who had on several occasions fallen helpless in the street from paralysis of the left leg caused by the pressure of a small intra-ligamentous fibroid tumor. All the pressure-symptoms are exaggerated at the menstrual period, on account of the swelling of the tumor that occurs at this time.
Pressure upon the rectum is often very marked, and may cause constipation and hemorrhoids. Pressure upon the ureters causes dilatation, hydronephrosis, and uremia. This is a not infrequent cause of death, both in the untreated case and after operation for the relief of fibroids.
The effect of fibroid tumors of large size upon the heart and blood-vessels has been remarked by several writers. Fatty degeneration and brown atrophy have been found associated with uterine fibroids in a number of instances. This is undoubtedly the explanation of some cases of death after operation.
Martin has called attention to the disposition to thrombosis and embolism which seems to be especially marked 246 in the telangiectatic form of tumor. This also explains some of the cases of sudden death that occur after operation. Operators have observed cases of sudden death, probably from embolism, occurring sometimes several weeks after hysterectomy for fibroid tumor.
The diagnosis of uterine fibroids is made from a study of the symptoms already described and from the physical examination.
If the tumor is large enough to be palpated through the abdominal wall, the hard consistency and the irregular bossed outline of the multinodular form of fibroid may be detected.
By bimanual examination we determine the general enlargement, and perhaps the irregular outline, of the uterus. Sometimes, when the fibroid is small and interstitial, a slight elevation, or perhaps merely a local induration, may be felt. By grasping the cervix with a tenaculum and drawing it down while the palpating finger is in the rectum the whole of the posterior face of the uterus may be explored and small fibroid nodules discovered.
The tumors are found to be continuous with the uterus and movable with it. If the tumor is sufficiently large to be grasped by an assistant, who draws it up or to either side, it will be found that the motion is communicated to the vaginal cervix. The cervix is often very hard, and may have been dragged upward to such an extent that it cannot be reached by the vaginal finger; or it may project from the rounded surface of the tumor like the nipple on the breast.
The hard, non-fluctuating character of the tumor may usually be determined by bimanual examination. A sensation resembling that of fluctuation may be elicited in the edematous fibroid, and true fluctuation is, of course, present in the cystic variety.
The uterine sound shows the increased length and the irregularity of the uterine cavity. The sound is not often 247 necessary for diagnosis. It is useful, however, in the case of small interstitial fibroids. It will be remembered that uterine enlargement is one of the most usual symptoms of fibroid tumor.
The presence in the wall of the uterus of a hard nodule or of an area of induration, with a decided increase in the length of the uterine cavity (three to four inches), is strong evidence of fibroid tumor.
Those fibroid tumors which cause symmetrical uterine hypertrophy without any irregularity of surface are sometimes difficult of diagnosis. They have been mistaken for the pregnant uterus. The reverse mistake has also very frequently been made, and the woman has been subjected to celiotomy for fibroid tumor when a normal pregnancy alone was present. The differential diagnosis between fibroid and pregnancy is usually not difficult. In making such a differential diagnosis it must be remembered that in some cases of pregnancy the menstrual periods continue during the early months or throughout the course of pregnancy, and that irregular bleeding may occur during pregnancy; also, on the other hand, that the symptoms of menorrhagia and metrorrhagia may be absent in the case of fibroid tumors. Mammary changes, nausea, and pigmentation of the skin may occur with fibroid tumors as with other diseases of the uterus or the ovaries, and resemble the similar phenomena of pregnancy. The bluish discoloration of the ostium vaginæ, the soft cervix, the pulsation of the vaginal vessels, the movements of the child, and the fetal heart-sounds are absent in fibroid tumors. The recent history of the tumor and its typical increase in size are observed in pregnancy.
In the event of doubt the case should be watched for a few months until the diagnosis becomes clear. Fibroid tumors are of slow growth, and such delay is usually not dangerous.
If the fibroid tumor is complicated with pregnancy, 248 the diagnosis becomes more difficult. This complication is not an unusual one, and should always be borne in mind.
The differential diagnosis between uterine fibroid and ovarian cyst is easy except in the case of the fibro-cystic tumor. Such tumors have very often been mistaken for ovarian cysts. The mistake is not at all serious, as celiotomy is indicated in either case. The operator, however, should always determine the nature of the tumor before proceeding with the operation after the abdomen has been opened, as puncture of a fibro-cystic tumor may be attended by alarming hemorrhage.
A small fibroid in the posterior wall of the uterus has often been mistaken for retroflexion, and the woman has been treated with a pessary. This mistake may be avoided by feeling, with the abdominal hand, the fundus uteri in its normal forward position, or by determining the true direction of the uterus with the uterine sound.
The prognosis of uterine fibroids may be determined from a consideration of the natural history, the degenerations, and the complications of these neoplasms, which have already been described.
Fibroid tumors are benign growths, in contradistinction to cancer and sarcoma. They do not infiltrate contiguous structures or invade the general system; but they are not benign in the sense that they are not dangerous to life.
As has been said, the disease may terminate as a uterine polyp, which may be discharged from the body. But during this process the woman may die from hemorrhage or from septic absorption from the sloughing, disintegrating tumor.
Some unusual fibroids give no trouble whatever, never attain a large size, and are discovered only accidentally during the life of the woman or at the autopsy.
In very exceptional cases—so rare that they are to be looked upon as medical curiosities—the fibroid disappears 249 spontaneously even after it has reached a large size. This has occurred as the result of an accident, exploratory celiotomy, and pregnancy.
We have no right in any case, however, to look for such favorable termination.
The accidents that may happen to the tumor itself, and which imperil the life of the woman, are various and occur frequently. The dangerous forms of degeneration—the edematous, the cystic, the telangiectatic, and the sarcomatous—occur with sufficient frequency always to be dreaded; and, even though these dangers be avoided, the anemia from the continual hemorrhage exposes the woman to fatal results from the diseases and accidents of daily life. The most favorable course that we have a right to expect, in any case of fibroid tumor of the uterus that is not discharged as a uterine polyp, is that it will grow slowly, that it will produce symptoms not unendurable, and that at the menopause it will cease to grow and will atrophy or disappear.
This comparatively favorable course condemns the woman to a life of invalidism, more or less marked, during the years that should be the most useful and active of her existence. The menopause may be delayed for five, ten, or fifteen years, or it may be indefinitely postponed; and even after the menopause has occurred, in a certain number of cases the fibroid, contrary to the usual rule, continues to grow, and may ultimately cause death.
Treatment of Fibroid Tumors of the Uterus.—Operative treatment is usually demanded in the case of fibroid tumors. A few years ago the treatment usually advised was palliative and expectant. The imperfect technique rendered operations for this disease so fatal that it was considered safest for the woman to allow the tumor to pursue its natural course, hoping that, if small and single, it would be discharged as a polyp, or that it would grow slowly and would atrophy at the menopause, the physician meanwhile relieving as much as possible, 250 by palliative treatment, the symptoms that presented before this favorable termination.
Many women, following this advice, have suffered through the years of active life, and have finally found relief and cure when the menopause was reached; others have started upon this dreary course, and have died from some of the accidents incident to these tumors; still others have passed through these years of suffering, and then have found the hoped-for goal vanished, the menopause indefinitely postponed, or the tumor continuing to grow after this period had been reached.
Many of these women are driven to the operating-table to-day, after lives that have been wasted by this expectant plan of treatment.
The great majority of fibroid tumors of the uterus demand immediate operation. The operative technique has been so perfected that the mortality after operation is very small. The danger of operation is much less than the dangers to which the woman is exposed from the various accidents that are liable in this disease.
There are some cases, however, in which immediate operation is not demanded. In a young woman with a fibroid tumor of small size that is not causing serious symptoms operation may be deferred and the case may be watched. This plan is especially desirable if the woman is anxious to have children. She should be told, however, that conception is less likely to occur than in the well woman, that she is liable to abort, and that the tumor will grow more rapidly during her pregnancy. On the other hand, there is the possibility of its disappearance after labor.
If the tumor, even though small, is intra-ligamentous and of pelvic growth, the expectant plan of treatment is not justifiable. Dangerous pressure-symptoms are too imminent, and if pregnancy occurs labor will be obstructed. If the woman has reached the menopause, if menstruation has ceased, and the tumor is causing no 251 serious symptoms from its size and position, the case may be watched with the hope that the disease will shortly become quiescent. Such cases are exceptional. Usually the tumor produces symptoms that render the woman more or less of an invalid, and she should not be condemned to this suffering and to the dangers of waiting. In these cases we must not rely altogether upon the statement of the woman in regard to the suffering caused by the tumor. A woman, dreading operation, will often underrate her suffering, or she will consider as normal the disturbances to which she has, through a long period of years, gradually become accustomed.
No drug has been discovered that has any influence upon the growth of the fibroid tumor.
The most serious symptom, hemorrhage, may be alleviated in a variety of ways. Rest in the recumbent posture, to relieve congestion, is most important. Such rest is especially demanded at the menstrual period. Pressure-symptoms and pain are likewise relieved by rest. Careful attention to the regularity of the bowels is desirable. The administration of saline purgatives to the extent of mild purgation depletes the pelvic circulation, and is especially useful immediately before a menstrual period. Coitus should be avoided immediately before and during the menstrual period.
Ergot, gallic acid, hydrastis, bromide of potash, and erigeron are useful to control the bleeding. They should be administered in frequently repeated doses for a long period.
Thorough curetting of the cavity of the uterus is the most certain method of controlling the hemorrhage. By this procedure the diseased endometrium is removed, and the bleeding is usually very decidedly diminished for several months afterwards.
The treatment by electricity, once popular with some physicians, has not stood the test of time and experience. It does not stop the growth of the tumor. It has caused 252 many deaths. It may produce peritoneal adhesions, which render subsequent operation most difficult.
Ligature of the arteries supplying the uterus has been performed with the object of arresting the growth of a uterine fibroid. The results of this operation, however, have not been satisfactory.
Salpingo-oöphorectomy has been practised for a number of years, and a large number of fibroid tumors have been cured by it. Before the present perfected technique of hysterectomy had been developed salpingo-oöphorectomy was much the safer operation, and was always practised whenever possible.
The object of the operation is to cause arrest of growth and atrophy of the tumor by stopping menstruation and producing a premature menopause.
According to the statistics of Tait, the operation results in cure of the fibroid in 95 per cent. of the cases.
In some cases the bleeding stops immediately and never recurs; in other cases the bleeding continues, in steadily diminishing amount, for several weeks or a few months after the operation; and finally, in a small proportion of the cases, the bleeding is not arrested at all.
The atrophy of the tumor after this operation is also variable. Sometimes the atrophy begins immediately, and in a few weeks after the operation has proceeded to a very marked degree, the tumor disappearing or being so small as to give no trouble; in other cases the atrophy is much slower; sometimes there is no arrest of growth whatever.
The operation seems to produce most benefit in cases of the hard fibroid. The edematous fibroid is often unaffected by it; and it is not applicable in the case of fibro-cystic tumors, which continue in unabated growth.
In performing the operation it is important that every portion of ovarian tissue should be removed, and that the Fallopian tube should be amputated as closely as possible to the uterine cornu. Many cases of failure of this operation are due to neglect of these precautions. 253
A very small portion of ovarian tissue may be sufficient to continue menstruation.
A good many women who had derived no benefit from the first operation have been subjected to a second operation, a small remaining portion of the ovary being removed or the stump of the Fallopian tube being excised, complete cure resulting.
The nature of the influence of the Fallopian tube in this matter is not understood. Tait lays especial stress upon the necessity of its complete removal.
The importance of the removal of the tubes may be realized from Tait’s statement that “removal of the ovaries alone is followed by immediate and complete arrest of menstruation in about 50 per cent. of the cases. Removal of both tubes, with or without the ovaries, is followed by the same arrest in about 90 per cent. of the cases.” From this statement it appears that if one wishes to stop menstruation, removal of the tubes is of even more importance than removal of the ovaries.
The operation of salpingo-oöphorectomy is not advisable in some cases, and in some others it is impossible to perform it.
As has already been said, the operation is likely to fail in the soft edematous fibroids. It should not be advised in the fibro-cystic tumors. It is not advisable in the case of large fibroid tumors of abdominal growth, because, even though atrophy occur, it will be slow, and the symptoms referable to the large hard tumor in the abdomen will be but slowly relieved.
The operation is not applicable to the intra-ligamentous fibroid of pelvic growth, producing urgent pressure-symptoms that demand certain and immediate relief. In the case of profuse exhausting hemorrhage, when the anemia is so great that immediate and certain arrest of bleeding is required, salpingo-oöphorectomy should not be practised.
If the woman has reached the menopause, and, notwithstanding 254 the cessation of menstruation, the tumor continues to grow, salpingo-oöphorectomy will do no good.
In some cases the tubes and ovaries cannot be removed. They often occupy a position behind or under the tumor, so that they cannot be removed without first taking the tumor away. The tube and ovary may be so distorted that only partial excision is possible, and this will result in no benefit; or the tube and ovary may be spread out upon the face of the tumor, incorporated with its capsule, so that removal is impossible, and any attempt at removal may result in rupture or penetration of large venous sinuses—a most dangerous accident.
The operator should therefore never undertake the operation of salpingo-oöphorectomy for uterine fibroid unless he is prepared to perform hysterectomy if this operation is found necessary.
Hysterectomy is deservedly the favorite operation for uterine fibroids at the present day.
The danger of the operation is small, being but little, if any, greater than that attending salpingo-oöphorectomy for fibroids, if we compare only those cases in which either operation may be performed.
The operation is applicable to every kind of fibroid tumor. The relief of symptoms is immediate and certain.
The reflex symptoms, such as backache and headache, which are directly due to the pathological condition of the uterus, often disappear immediately and permanently. This cannot be said of salpingo-oöphorectomy, after which operation these symptoms often continue for an indefinite period.
The treatment of uterine fibroids has followed in development the growth of abdominal and pelvic surgery. In the days when celiotomy was a dangerous operation the palliative treatment was advisable. When salpingo-oöphorectomy could be safely performed this treatment 255 was practised; and now that hysterectomy is equally safe, it has become the operation of election.
The details of the operation of hysterectomy for uterine fibroids will be considered in a subsequent chapter.
Myomectomy (Abdominal).—In some cases of uterine fibroid it is possible to remove the tumor without taking away the uterus. This operation, when performed through an abdominal incision, is called abdominal myomectomy. From a surgical standpoint it is the ideal plan of treatment, as the woman is cured of the disease without suffering mutilation.
Myomectomy is especially adapted to the treatment of single fibroid tumors which may be excised or shelled out of the body of the uterus. It is indicated in the case of young women who are anxious for children.
The field of myomectomy is at present a limited one. Single subperitoneal and interstitial fibroid tumors are rare. Even though the secondary nodules may be small at the time of operation, they will grow after the removal of the chief mass. Hysterectomy has been required at a second operation in a woman on whom myomectomy had been first performed.
The operation is still on trial: its limitations and remote results have not yet been determined. It should be performed only by the experienced abdominal surgeon. Many fatal cases of post-operative hemorrhage and of sepsis have occurred. Though successful cases have been reported by men of unusual skill and experience, in which large numbers of uterine fibroids have been removed from the uterus at one operation, yet these cases must be looked upon as rare surgical triumphs which it is to be hoped will become more frequent in the future.
On the ground of safety, hysterectomy is to be preferred to myomectomy.
The details of the operation of myomectomy are described in a subsequent chapter. 256
When the fibroid tumor is complicated by pregnancy it may be necessary to perform Cesarean section, followed by hysterectomy. This is not justifiable, however, unless the fibroid is so situated that the passage of the child by the natural way is impossible. The fibroid usually increases more rapidly in size during pregnancy, but may diminish a good deal with the involution of the uterus.
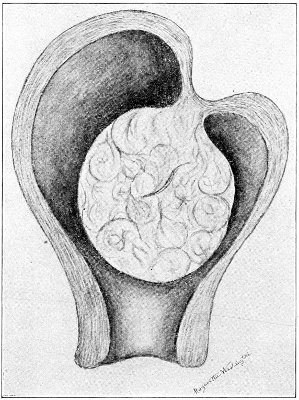
Fig. 134.—Fibroid polyp producing partial inversion of the uterus.
Treatment of the Fibroid Polyp.—When the fibroid tumor is polypoid, and projects into the uterine cavity, or the cervix, or beyond the external os, none of the operations that have just been described are required. The tumor should then be attacked by way of the vagina. If the fibroid polyp projects from the external os, the pedicle may very easily be divided with curved scissors. If the tumor is still within the cavity of the uterus, it will be necessary to dilate the cervix, or to enlarge the canal by lateral incisions, so that the pedicle may be 257 reached. It should always be remembered that the polyp may, by traction, produce partial or complete inversion of the uterus (Fig. 134), and in dividing the pedicle, therefore, the operator should cut close to the tumor, leaving, if necessary, a portion of the surface of the tumor. In case the polyp is so large that the vagina is filled to such an extent that the pedicle is not accessible, it is advisable to remove the tumor piecemeal, grasping portions with a tenaculum and cutting away with scissors until the pedicle is reached. The fibroid polyp is not vascular, and hemorrhage is not alarming. The pedicle usually contains no large vessel. It retracts after the tumor has been cut away, and spontaneous hemostasis is secured. It was formerly the custom to ligate the pedicle or to remove the polyp with the écraseur, but these methods are unnecessary. If any hemorrhage should follow the operation, the cavity of the uterus should be packed with sterile gauze.
Adenomyoma is a rare form of myoma of the uterus, which contains epithelial canals of the glandular type. Unlike the common fibromyoma, this tumor has no connective-tissue capsule and its structure cannot be well differentiated from the tissue of the surrounding uterine wall.
Adenomyomata are of two varieties: in one variety the epithelial canals seem to be derived from the utricular glands; in the other from the embryonal remains of the Wolffian body.
In the first variety the tumor is situated in the posterior, anterior, or lateral uterine wall, and has the usual characteristics of a fibromyoma, except for the presence of glandular structures and the absence of a capsule.
Adenomyomata, which are derived from the Wolffian body, develop in the posterior portion of a uterine horn, or less often in the tube, and when small, in the peripheral layers of the muscular wall. The tumor may afterward become interstitial or submucous. 258
These tumors are of various degrees of hardness. They may be dense in consistence, in case the muscular tissue is in excess of the glandular, or they may be soft cystic tumors containing numerous distinct macroscopic cavities. Telangiectatic adenomyomata also occur.
The treatment of adenomyoma of the uterus is hysterectomy. 259
If there exists in the genital tract any obstruction that prevents the escape of menstrual blood, the uterus will become distended and the condition of hematometra will be present. If the retained fluid consists chiefly of the mucous secretion of the utricular glands, the condition is described as hydrometra; or if suppuration has taken place, so that the uterus becomes distended with pus, the condition is called pyometra.
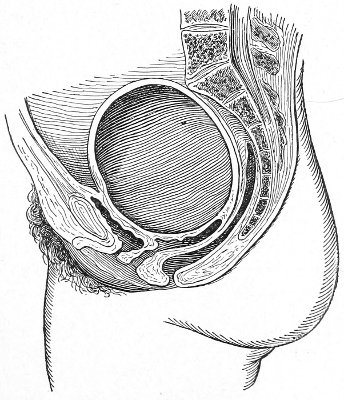
Fig. 135.—Hematometra.
The uterine walls may be very much attenuated by the distention, or the muscular coat may hypertrophy as the accumulation progresses. 260
The cause of these conditions may be congenital or acquired atresia of any part of the genital tract. The symptoms usually appear after puberty. The menstrual period is accompanied by intense bearing-down pain in the region of the uterus. There is no appearance of menstrual blood. A round tumor may be felt in the hypogastrium. Examination will reveal the obstruction in the cervical canal. Sometimes the chief accumulation and distention occur in the cervix; in other cases the body of the uterus is chiefly affected.
Distention of the Fallopian tubes, with the formation of hematosalpinx, hydrosalpinx, or pyosalpinx, often accompanies old cases of hematometra.
The treatment consists in relieving the obstruction and in maintaining the patulous condition of the genital tract. If the cervix is the seat of the obstruction, it should be punctured with a trocar and thoroughly dilated. It may be necessary to practise repeated dilatation in order to keep the canal open.
The accompanying disease of the Fallopian tubes may persist after drainage of the uterus, and salpingo-oöphorectomy or hysterectomy may be ultimately required. 261
Tuberculosis of the uterus is not a very rare disease. In this respect it differs from tuberculosis of the cervix, which, as has already been said, is a most unusual site for the appearance of tuberculosis. Even in advanced cases of tuberculosis of the body of the uterus it is very rare that the condition extends below the internal os.
Tuberculosis of the uterus is often found post-mortem in women who have died of phthisis or other form of tubercular disease. It has also been recognized during life, and operation has been performed for its relief.
Tuberculosis of the uterus seems most frequently to be secondary to a tubercular lesion in some other part of the body. It often begins in the Fallopian tubes, and extends thence to the endometrium; or it may be primary in the endometrium, caused by infection through the genital tract.
The disease first attacks the endometrium, and in the late stages extends to the muscular coat.
Tuberculosis of the endometrium may occur in three forms—miliary tuberculosis, chronic diffuse tuberculosis (caseous endometritis), and chronic fibroid tuberculosis.
Miliary tuberculosis of the uterus may be part of a general miliary tuberculosis. Typical miliary tubercles are found scattered throughout the endometrium, usually situated immediately beneath the epithelium (Fig. 136).
Chronic diffuse tuberculosis is the most frequent form. The uterine cavity is filled with cheesy material. The mucous membrane is the seat of irregularly shaped ulcers and tubercles in various stages of development. When the disease has extended to the muscular coat of the 262 uterus, the whole organ becomes considerably enlarged. Degeneration and softening of the uterine wall may be so extensive as to cause rupture. The internal os may become closed, and a pyometra may be produced.
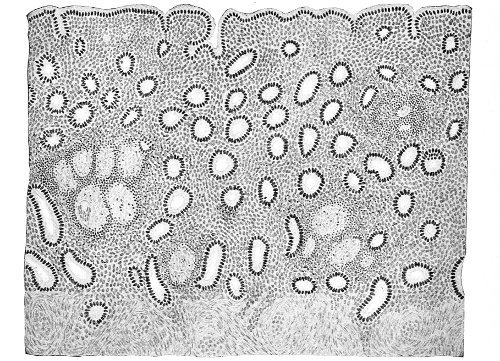
Fig. 136.—Miliary tuberculosis of the endometrium and glandular endometritis (Beyea).
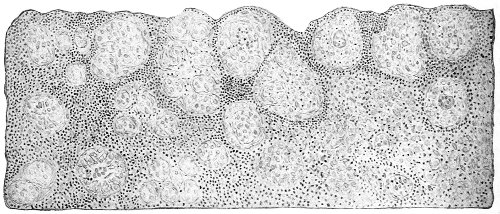
Fig. 137.—Advanced fibroid tuberculosis of the endometrium (Beyea).
Chronic fibroid tuberculosis of the endometrium seems to be the rarest form of the disease. A microscopic section of this form of tuberculosis is shown in Fig. 137. The endometrial tissue was almost entirely destroyed, 263 and was replaced by a mass of typical miliary tubercles. There were no traces of glandular tissue. The tubercles were separated from each other by a very extensive small round-cell infiltration and a small amount of remaining stroma tissue. To the naked eye the endometrium did not appear to be diseased.
Tuberculosis of the uterus may occur at any period of life. It is most often found between the twentieth and fortieth years.
The symptoms of tuberculosis of the uterus are not at all characteristic. In the early stages they resemble those of non-tubercular endometritis. There is sometimes a very profuse leucorrhea, which may contain the characteristic cheesy material. The body of the uterus may be considerably hypertrophied. If the condition follows tuberculosis elsewhere, or if any form of genital tuberculosis exists in the husband, the physician would be led to suspect tuberculosis of the uterus.
The diagnosis can be made only by thorough curetting of the uterine cavity and the microscopic examination of the tissue removed. The tubercle bacillus has not often been found, but the other microscopic appearances are frequently characteristic. In the case from which the section shown in Fig. 137 was taken the diagnosis of tuberculosis of the endometrium was made by such curetting and examination.
The treatment of tuberculosis of the uterus is hysterectomy. The operation is indicated in every case except those in which there is present in some other part of the body an incurable tubercular lesion. 264
In inversion of the uterus this organ is turned partly or completely inside out. The condition usually results from childbirth or from the growth of an interstitial or polypoid tumor.
There seem to be two factors that result in the production of inversion: a degeneration or atrophy of part of the uterine wall, and traction, as from the drag of a uterine polyp or of the umbilical cord. These causes may act together or independently.
If a portion of the uterine wall has lost its strength or tonicity, it may be depressed toward the uterine cavity. The depression is increased by the traction of a tumor or of the umbilical cord. The inversion having been started in this way, may be rapidly increased by uterine contractions. Emmet says that inversion usually takes place between the birth of the child and the delivery of the placenta. A consideration of the subject of acute inversion following labor belongs to obstetrics. It is very important that reduction should be accomplished immediately. The delay of a few hours greatly increases the difficulty of replacement. Emmet says: “The uterus is generally well contracted in twelve hours, and with many cases it would be then quite as difficult to effect a reduction as if a year had elapsed.”
If the placenta is still attached to the inverted uterus, it should be removed before reduction is attempted. Inversion of the uterus when seen by the gynecologist is usually of the chronic form. It has existed for a few weeks or for several years.
Various degrees of inversion are met with. Rarely 265 inversion of one horn of the uterus is seen. In the case of fibroid polyp there may be a slight depression of part of the uterine wall, resulting from local atrophy and traction. In other cases inversion of the fundus as far as the internal os exists. The most usual condition is one of complete inversion, in which the body of the uterus protrudes from the external os into the vagina (Fig. 138). The cervix may or may not be inverted. Sometimes the inversion is complicated by vaginal prolapse—or, rather, by inversion of the vagina—so that the whole genital tract becomes turned inside out and protrudes from the vulva. The exposed endometrium becomes congested and bleeds easily. Ulceration or gangrene may result.
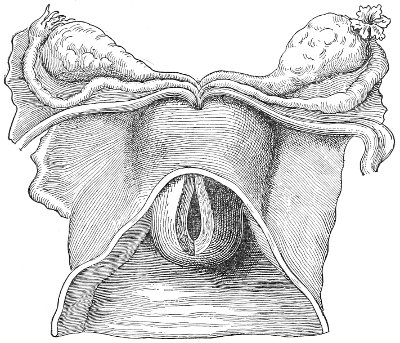
Fig. 138.—Complete inversion of the uterus.
If the inversion is extensive, the Fallopian tubes and the ovaries are drawn in the cup formed on the upper aspect of the uterus. Intestines or omentum may also lie in this cup. In cases of long standing the rim of the cup formed by the muscular cervix becomes very much contracted, and adhesions may take place between the peritoneal surfaces. These complications offer great, sometimes insurmountable, difficulty to reduction in old cases. 266
Inversion of the uterus is not a common disease. It is very rarely seen at the present day.
By far the most frequent form is that which follows labor; it is much less often caused by fibroid polyp. It seems especially likely to occur in sarcoma of the uterus.
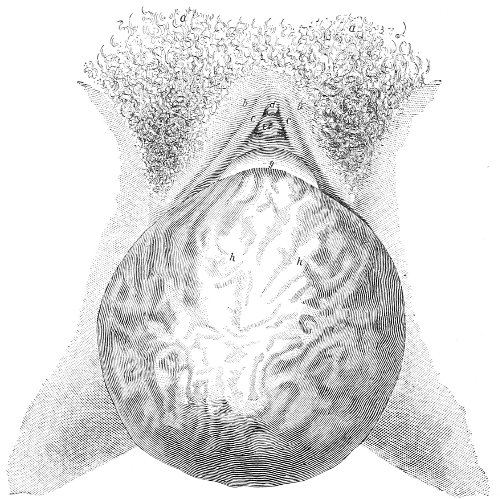
Fig. 139.—Inversion of the uterus (Jeançons): a, mons veneris; c, c, nymphæ; d, clitoris; e, external meatus; g, anterior lip of cervix; h, h, the internal surface of the uterus.
The symptoms of chronic inversion are hemorrhage, discharge, backache, bearing-down pains in the pelvis, vesical disturbance, very pronounced anemia, and general physical weakness. Menstruation is very much increased in amount, and intermenstrual bleeding may occur after standing or on any physical effort.
Inversion of the uterus very rarely exists without causing serious symptoms. The majority of unrelieved cases end fatally from anemia, septicemia, or peritonitis. A 267 few cases of spontaneous reduction and cure have been recorded.
The diagnosis of recent inversion is very easy. The body of the uterus usually projects into the vagina, and the placenta may be found attached to it. The abdominal hand fails to feel the rounded body of the uterus in the normal position, but in its place is a cup-shaped hollow.
Chronic inversion if uncomplicated by other lesion—e. g. a uterine tumor—may also be readily recognized by careful examination. There are, however, a number of cases on record in which the inverted fundus uteri was amputated in mistake for a fibroid polyp.
The diagnosis may be made by inspection, bimanual examination, and the uterine sound.
In complete inversion, inspection shows a round tumor filling the vagina or protruding from the vulva. The tumor is covered with mucous membrane, perhaps ulcerated in places, and sometimes partly covered with stratified squamous epithelium, which has, as a result of irritation, replaced the normal epithelium of the endometrium. It is of a deeper red color than a pedunculated fibroid. The tumor bleeds easily. In the only case of inversion seen by the writer the orifices of the Fallopian tubes could be determined.
Digital examination reveals the rounded shape of the tumor and its soft character—softer than a fibroid polyp. The tumor may be so soft that it becomes flattened against the posterior vaginal wall.
The tumor is found to be free on all sides except at its upper extremity, where there is a pedunculated attachment around which may be felt the more or less attenuated cervix.
If the cervical canal be not obliterated by adhesion to the neck of the tumor, the finger may be passed upward, and will determine that the mucous membrane is reflected symmetrically all around on to the neck of the tumor.
Unless the woman be fat, the abdominal hand will determine that the uterine body is not in its normal position. 268 In its place may be felt the cup-shaped portion of the inverted uterus.
If the woman be fat, the rim of the cup may be felt by palpation through the rectum, the uterus being drawn down, if necessary, by a tape passed around the upper portion of the tumor.
The sound passed around the neck of the tumor will show the diminished depth of the uterine cavity and the symmetrical reflection of the cervix on to the neck of the tumor.
If the inversion be partial, the fundus lying still above the internal os, the difficulty of diagnosis becomes much greater. Examination under anesthesia may be necessary, when the cup-shaped depression on the top of the uterus may be detected, and dilatation of the cervix will enable the examiner to palpate the intra-uterine tumor.
The differential diagnosis between inversion and uterine polyp is made by determining, in the latter condition, that the body of the uterus lies in its normal relationship to the cervix, and that the upper surface is not cupped.
The sound usually passes to unequal distances around the neck of a fibroid polyp, unless it be situated symmetrically in the centre of the fundus. The depth of the uterus in the case of uterine polyp is usually greater than two and a half inches, as a result of the hypertrophy that accompanies polypi.
It is said that if the sound passes to a less depth than two and a half inches in the case of uterine polyp, accompanying partial inversion of the uterus should be suspected.
Treatment.—As I have already said, an inverted uterus should be reduced immediately after the accident occurs. If this is not done, the difficulties of reduction become very great. Until about fifty years ago, reduction in chronic cases was considered to be impossible. A considerable variety of methods of reduction have been recommended. Some operators advocate reduction by the hands alone; others advise the assistance of instruments; 269 and others, again, the employment of continuous elastic pressure.
The woman should be kept in bed for a few days before the operation. Saline laxatives should be administered. The parts should be prepared by vaginal injections of hot water in large quantity, administered three times a day. A large Barnes bag or colpeurynter filled with air or water should be placed in the vagina for two or three days before the operation, in order to distend the genital tract sufficiently to admit the hand. In some cases the pressure of such a bag, applied for from one to eleven days, has itself effected reduction. At the time of operation an anesthetic should be administered and the woman should be placed in the lithotomy position. The bladder should be emptied.
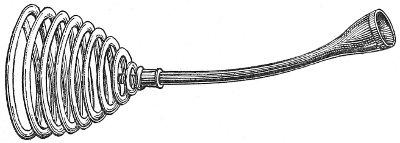
Fig. 140.—White’s repositor for inversion of the uterus.
The hand should be greased before introduction into the vagina. Emmet describes the method of reduction as follows: “My hand was passed into the vagina, and, with the fingers and thumb encircling the portion of the body close to the seat of inversion, the fundus was allowed to rest in the palm of the hand. This portion of the body was firmly grasped, pushed upward, and the fingers were then immediately separated to their utmost; at the same time the other hand was employed over the abdomen in the attempt to roll out the parts forming the ring, by sliding the abdominal parietes over its edge. This manœuver was repeated and continued. At length, as the diameter of the uterine cervix and os was increased by lateral dilatation with the outspread fingers, the long diameter of the body of the uterus became shortened, and the degree of inversion proportionally lessened. 270 After the body had advanced well within the cervix, steady upward pressure upon the fundus was applied by the tips of all the fingers brought together.”
The reduction may be aided by the use of White’s repositor (Fig. 140). This instrument consists of an india-rubber cup set on a curved iron staff which has at its other end a stout spiral spring. The cup is placed against the inverted fundus, and the spring against the body of the operator, who is thus enabled to maintain continuous pressure during the manipulations of his fingers.
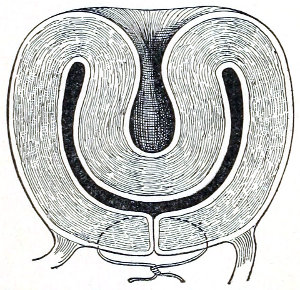
Fig. 141.—Emmet’s method of retaining partially reduced inversion.
Reduction of chronic inversion by manual methods is a long and exhausting process, requiring sometimes three or four hours for its accomplishment. It is advisable to have several assistants for mutual relief. It may be necessary to desist, and to repeat the operation when the condition of the patient permits it. In case the reduction can be but partially accomplished, or when, from any cause, the attempt at reduction has to be temporarily abandoned, the result of the work done may be preserved by a method of Emmet’s of temporarily closing the cervix by suture (Fig. 141). This procedure not only prevents the complete inversion from returning, but the traction produced by stretching the cervix over the fundus itself favors reduction.
Reduction by Continuous Elastic Pressure.—This method is employed after the manual method has failed, or it may be used primarily. As has been said, the gradual pressure of a colpeurynter has in several instances accomplished reduction. 271
The most efficient instrument for maintaining continuous pressure consists of a wooden cup set on a stem that extends out of the vagina. Pressure is made by firm elastic bands attached to the stem; these bands pass, two in front and two behind, to a broad abdominal bandage. The elastic pressure is maintained for from one to three weeks.
The parts must be carefully watched for sloughing. The rim of the cup of the repositor should be covered with lint saturated with carbolized oil. The instrument should be removed and reapplied every day.
The direction of pressure may be regulated by the tension of the elastic bands.
Splitting the posterior lip of the cervix is sometimes a useful procedure in cases that have resisted other treatment. The cervix is split in the median line posteriorly; the body and fundus are replaced by taxis, and the incision is then closed by suture.
If inversion accompany a uterine polyp, the tumor should be removed; and if the inversion is not spontaneously corrected, it must be reduced.
If, after careful trial of conservative methods, reduction of an inverted uterus is found to be impossible, the physician may be compelled to amputate the inverted portion or perform hysterectomy. 272
The review of a few facts about the anatomy of the Fallopian tubes will assist in the study of the diseases that affect these structures.
The average length of the normal Fallopian tube is 4 inches (10 centimeters). The tubes are often of unequal length, the difference sometimes being equal to 1 centimeter. The length of the Fallopian tube is subject to considerable variation, and in some forms of ovarian disease the length of the tube may be very much increased.
The uterine end of the tube varies in thickness from 2 to 4 millimeters. The outer end varies from 7 to 10 millimeters in thickness.
The narrow uterine end of the tube is called the isthmus. The outer end, of trumpet-shape, is called the ampulla. The canal of the tube is small. At the uterine end, or ostium internum, it will barely admit a bristle. Beyond the middle of the tube the canal gradually widens to the outer opening—the ostium abdominale.
The ostium abdominale is surrounded by peculiar luxuriant folds of mucous membrane called fimbriæ. The fimbriæ are formed by the outward bulging of the exuberant mucous membrane.
The Fallopian tube consists of three coats, the peritoneal, the muscular, and the mucous.
The peritoneal coat, which invests the tube for two-thirds of its circumference, is formed by the free border of the broad ligament, between the folds of which the Fallopian tube lies. Loose connective tissue attaches the peritoneal to the middle or muscular coat. 273
The muscular coat consists of unstriped muscular fiber which is continuous with that of the uterus. The muscular fibers are arranged in two layers, an outer longitudinal and an inner circular layer.
The inner or mucous coat, which is continuous with the mucous membrane of the uterus, is covered with columnar ciliated epithelium.
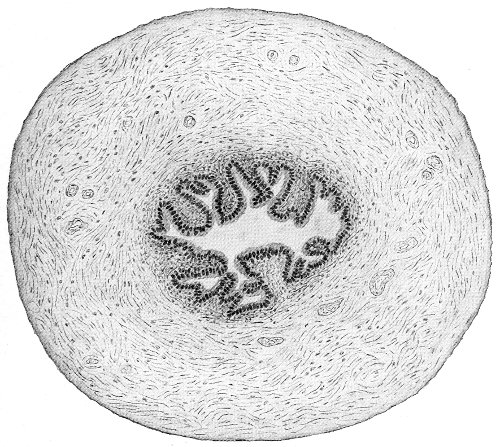
Fig. 142.—Section of the normal Fallopian tube near the uterine cornu (Beyea).
In the outer portion of the tube the mucous membrane is thrown into longitudinal folds or plicæ. These folds increase in thickness and in number as the ostium abdominale is approached. The difference in the degree of plication at the two ends of the tube is shown by Figs. 142, 143. The folds of mucous membrane project beyond the ostium to form the fimbriæ. Like the rest of the mucous membrane, the fimbriæ are covered by columnar ciliated epithelium.
The peritoneal covering does not, as a rule, extend on 274 to the fimbriæ. It terminates by a sharp line which marks also the termination of the circular muscular fibers of the middle coat of the tube. The fimbriæ are subject to great variation in number and in distribution. Sometimes the Fallopian tube has one or two accessory ostia in the vicinity of the usual opening. These accessory ostia are situated on the upper aspect of the tube and are surrounded by more or less luxuriant fimbriæ. Occasionally a small pedunculated tuft of fimbriæ is found on the outer portion of the tube (Fig. 144, B). In some cases 275 there is an accessory tubal end supplied with an ostium (Fig. 144, A).
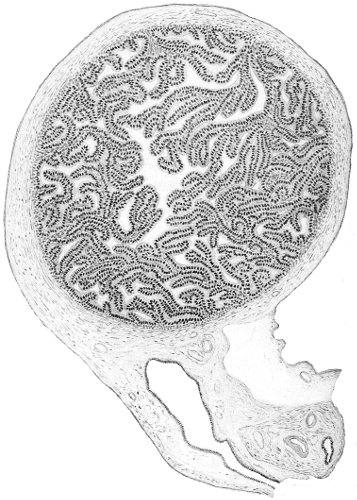
Fig. 143.—Section of the normal Fallopian tube near the abdominal ostium (Beyea).
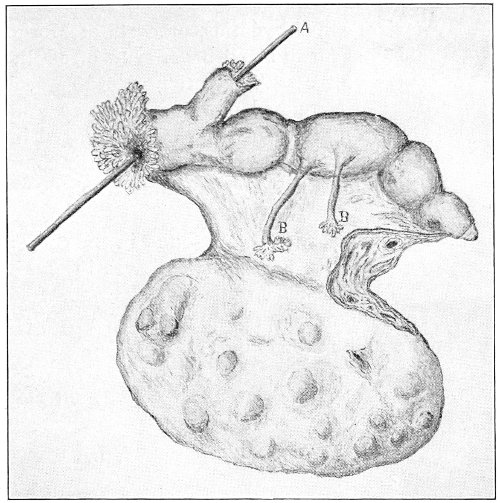
Fig. 144.—Fallopian tube and ovary: A, accessory tubal end with an ostium; B, pedunculated tuft of fimbriæ.
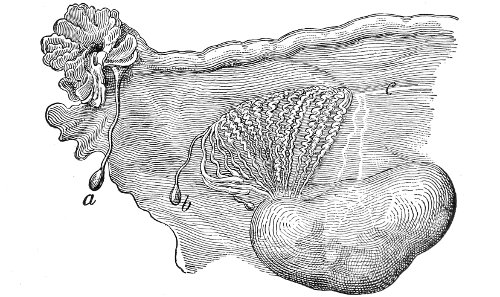
Fig. 145.—Fallopian tube, ovary, and parovarium: a, hydatid of Morgagni; b, cyst of Kobelt’s tube; c, Gärtner’s duct.
Very often a small pedunculated cyst, about the size of a pea, is found attached to the fimbriæ or to the outer aspect of the tube. 276
These cysts are called hydatids, or cysts of Morgagni. They are said to occur in about 8 per cent. of adults and in 20 per cent. of fetuses. They are not pathological.
The cyst wall is composed of three coats: an external peritoneal coat; a middle muscular coat, arranged in two layers; and an inner mucous coat covered with columnar ciliated epithelium. The cyst contains a clear watery fluid.
No distinct glands, such as are found in the cervix and the body of the uterus, have been observed in the Fallopian tubes. The mucous crypts formed by the folds of the mucous membrane are probably glandular in character and secrete an albuminous fluid.
Inflammation is the disease that most usually affects the Fallopian tubes. The condition is, as a rule, secondary to endometritis, the mucous membrane of the tubes becoming inflamed by direct extension from the mucous membrane of the uterus.
The causes of salpingitis are as numerous as those of endometritis. The most common causes of salpingitis are sepsis and gonorrhea.
Any form of inflammation of the endometrium may extend to the Fallopian tubes, but the septic and the gonorrheal forms of endometritis are especially virulent, and it is the rule in these diseases that the tubes are affected.
The various forms of glandular and interstitial endometritis that have already been described, and which are due to subinvolution, laceration of the cervix, uterine displacements, fibroid tumors, etc., may exist for a long time without producing any perceptible disease of the tubes. In sepsis and gonorrhea, however, the tubes become very quickly affected after the uterine cavity has been invaded, and for this reason these forms of endometritis excite the greatest apprehension. 277
Like inflammation of other structures, salpingitis may be either acute or chronic.
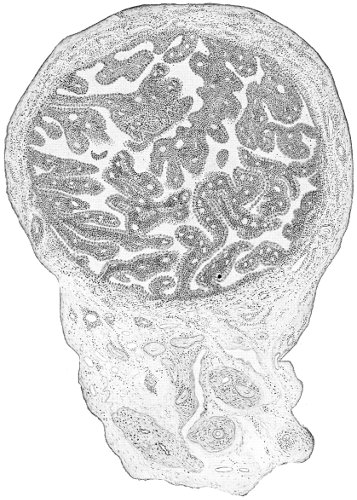
Fig. 146.—Acute septic salpingitis: section about the middle of the tube (Beyea).
Acute Salpingitis.—In the first stages of acute salpingitis the disease is confined to the mucous membrane of the tube. It very quickly extends thence, however, to the muscular and peritoneal coats, which become infiltrated with embryonic cells characteristic of the early stages of inflammation (Fig. 146).
If the tube is laid open, the mucous membrane is found 278 covered with a muco-purulent secretion. The whole tube is soft, succulent, and friable. The friability is such that the tube may readily be ruptured by bending. The fimbriæ are swollen and congested. A drop of pus is often seen exuding from the ostium abdominale.
In acute salpingitis the tube may become very quickly (in a week or ten days) enlarged to the size of the index finger or the thumb.
The condition that has been described is that found in the severe cases of acute salpingitis, the result of gonorrhea or of sepsis after labor. Opportunity is afforded to examine such cases when the woman has been subjected to celiotomy, or at the post-mortem when the woman has died of acute peritonitis or sepsis.
It is probable that a good many cases of acute salpingitis undergo resolution, and that the tube is restored to its normal condition.
It is also probable that milder forms of acute salpingitis occur—cases in which the disease is limited to the mucous membrane and is merely catarrhal in character, there being no pus, but a hypersecretion of mucus from the tube-lining. Such cases, however, recover or pass into a chronic form of simple catarrhal salpingitis; and the diagnosis made by a study of the subjective and objective symptoms cannot be confirmed by operation or autopsy.
Resolution with perfect restoration of the Fallopian tube to its normal condition is, of course, always to be hoped for. In some cases a few fine peritoneal adhesions between the tube and neighboring structures—such as the ovary, the uterus, the anterior or the posterior surfaces of the broad ligament, or a loop of intestine—may result before resolution takes place, and persist after all other traces of inflammation have disappeared. In other cases cure may result, after a greater or less degree of permanent damage has been done to the abdominal ostium of the tube, by the shrinking and distortion or crumpling of the fimbriæ. Such indications of an old, cured attack 279 of salpingitis are not infrequently seen during celiotomy for other conditions.
When resolution and cure do not occur, a speedy fatal result may take place by direct extension of the infection from the tube to the general peritoneum, with the production of general peritonitis. Between this extreme and the mild forms of very localized peritonitis, marked by a few harmless adhesions, all degrees may exist. Sometimes a local accumulation of pus occurs in the pelvis, walled off from the general peritoneum by rapidly formed adhesions. In other cases a tubal abscess is quickly formed by inflammatory closure of the abdominal ostium and distention of the tube with pus; or the cellular tissue of the broad ligament may become infected, and the abscess may originate there. And, finally, if the woman escape these dangers, one or other of the various forms of chronic salpingitis may result, and render her a lifelong invalid.
Chronic Salpingitis.—Salpingitis is usually seen in the chronic form. An acute primary salpingitis must not be confounded with an acute attack of inflammation or with an acute exacerbation in an old chronic case. It is rare that acute gonorrheal salpingitis is seen. The disease is usually subacute or chronic from the beginning, as are many of the other manifestations of gonorrhea in woman, like gonorrheal cervicitis and endometritis. The most frequent form of acute salpingitis met with is the septic variety, which occurs as a result of septic infection after a criminal abortion, a miscarriage, or a labor. It is usually complicated by severe septic endometritis, peritonitis, or general sepsis.
The lesions found in chronic salpingitis are numerous. The simplest form of the disease is the chronic catarrhal salpingitis, in which the pathological changes are confined to the mucous membrane of the tube. The muscular and peritoneal coats are not affected. The ostium abdominale remains open and is of the normal shape. The mucous membrane is congested. The folds of 280 mucous membrane, or the plicæ, are hypertrophied from gradual infiltration of inflammatory products. The tube may become somewhat enlarged and more tortuous than normal. If the inflammatory condition extends to the middle or muscular coat of the tube, the interstitial form of salpingitis is produced. The wall of the tube becomes thicker and harder. The microscope shows an increased amount of connective tissue in the tube-wall.
As chronic salpingitis progresses the ciliæ of the lining cells disappear.
If the disease extends through the peritoneal coat, inflammatory adhesions take place between the tube and neighboring structures. The tube is often found adherent to the posterior aspect of the uterus, the broad ligament, or the ovary.
The most usual seat of adhesions is about the abdominal ostium. Adhesions here are caused by leakage or escape of septic material into the peritoneal cavity. The leakage is slow, and the gradually formed adhesions in time close the ostium by gluing it to adjacent structures, so that further escape of tubal contents by this opening is stopped.
If, in such a case, the tube is freed from its adhesions, the fimbriæ will be found in the normal position with the ostium abdominale open.
The usual method of closure of the distal end of the Fallopian tube is by another process. It takes place as follows: When the inflammation reaches the muscular coat of the tube, this coat becomes lengthened and extends beyond the fimbriæ, which apparently retract and become invaginated in the tube. The opening of the tube, instead of being flaring with protruding, diverging fimbriæ, becomes rounded and narrow (Fig. 147). The fimbriæ become drawn farther into the tube until they appear to be directed inward instead of outward. The ostium becomes narrower, and more rounded, until the edges finally meet and unite by peritoneal adhesions. 281
Tubes representing all stages of this process of closure are often found in operating for inflammatory disease.
Closure of the abdominal ostium by any method is to be viewed as a conservative process. It prevents leakage, through this channel, of septic material, and consequently diminishes the danger of peritonitis.
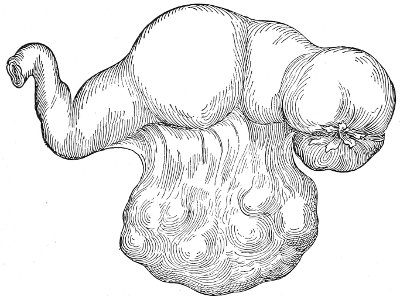
Fig. 147.—Salpingitis with partial inversion of the fimbriæ.
When the abdominal ostium has become closed, the tubal contents and secretions may have a sufficient passage for escape by the isthmus into the uterus, and no further changes take place beyond slow infiltration and degeneration of the tube-walls. The tube may become much hypertrophied, not from distention of the lumen, but as the result of simple inflammatory infiltration of the mucous and muscular coats, and may attain the size of the thumb. The walls may become much degenerated, soft, and friable, so that the tube may easily be cut through by a ligature or may be broken by bending.
The whole tube may become much elongated and very tortuous, reaching a length of six or eight inches. The isthmus of the tube, or the portion in immediate relation to the uterus, is usually least affected. The whole tube may become much hypertrophied, and yet the isthmus will remain approximately of its normal size. In other 282 cases, however, the disease extends throughout the whole length of the tube into the uterine horn, and the degeneration of the tube may be such that it may readily be broken off at its junction with the uterus.
If, after the ostium abdominale has been closed, anything occurs to obstruct the escape of the tubal contents into the uterus, cystic distention of the tube will take place. Such obstruction may be produced by swelling of the mucous membrane in the narrow isthmus; by cicatricial contraction; or by a sharp flexure in any part of the tortuous tube. Sometimes there are two or more distended portions of the same tube.
When the tube is distended with pus, the condition is called a pyosalpinx; when distended with a watery fluid, a hydrosalpinx; and when distended with blood, a hematosalpinx.
Tubal cysts of this kind may attain large size, in some cases equal to that of the fetal head.
The shape of the tube becomes much altered. The greatest distention is at the distal portion, so that the tube assumes a pear-shape. The lower portion of the tube is restrained by the mesosalpinx and the tubo-ovarian ligament, so that as the tube increases in length the upper portion appears to outgrow the lower, and a retort-shaped tumor results, or the tube may become tortuous and folded upon itself.
As the tube enlarges the layers of the mesosalpinx may become separated, and the tube burrows between them until it is brought into immediate contact with the ovary, and the retort-shaped tumor appears with the ovary lying in the concave portion.
In some cases the ovary and the tube become adherent by peritoneal adhesions, and the mesosalpinx, which is wrinkled and folded between them, may be restored by separation of the adhesions.
In other cases the mesosalpinx itself becomes much thickened by inflammatory infiltration, and keeps the tube and ovary separated. 283
In chronic salpingitis the inflammatory process usually in time extends to the ovary, and some of the forms of chronic ovaritis are produced.
The capsule of the ovary becomes thickened, and rupture of the ripe ovarian follicles is prevented. Small cysts throughout the ovary are formed in this way. Two or more cysts may become converted into one cavity by absorption of the intervening walls, so that cystic spaces of larger size, equal to that of a duck-egg, may result. Such cysts may become infected by pyogenic organisms from the tube, and an ovarian abscess is produced.
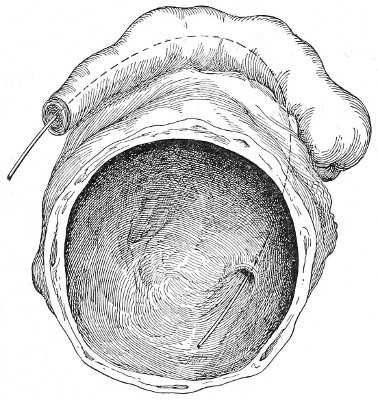
Fig. 148.—Tubo-ovarian abscess.
Tubo-ovarian Abscess.—If the tube is brought into immediate contact with the ovary, either by agglutination of the fimbriated end to the surface of the ovary, or by adhesion of the side of the tube to the ovary, or by burrowing between the layers of the broad ligament, the tissue intervening between the cavity of the tube and the cyst of the ovary may be absorbed or perforated, and the two cavities will be thrown into one, forming a tubo-ovarian abscess or a tubo-ovarian cyst (Fig. 148). The opening between the tubal and ovarian portions of the cyst does not usually correspond to the abdominal 284 ostium of the tube, but may be an adventitious opening in the side of the tube (Fig. 148).
Pyosalpinx.—When the Fallopian tube is distended with pus or with other fluid, its walls gradually become thinned. In this respect the Fallopian tube differs from the body of the uterus, in which a hypertrophy of the muscular coat usually takes place, under the influence of distention from the presence of retained fluid within it.
This gradual thinning of the tube-wall predisposes to rupture or leakage and the escape of the contents into the abdominal cavity. A pyosalpinx often becomes adherent to the rectum, the small intestine, or the bladder. The wall of the intestine or the bladder becomes perforated, and the pus is discharged in this way. It seems probable that in some unusual cases the obstruction in the lumen of the tube is temporarily overcome, and that evacuation takes place through the uterus, followed by refilling of the tube. This, however, is a very unusual occurrence, and is not frequent, as is assumed by some writers. The evidence of such discharge is based only on clinical observation. There is no good pathological evidence of such an occurrence. It is probable that in most of the reported cases the purulent or watery discharge which escaped in a sudden gush was derived from, and had been retained in, the body of the uterus.
The pus of pyosalpinx varies greatly in character. In the early stages of the disease it is actively septic and contains a variety of micro-organisms.
These organisms are the gonococcus, streptococcus, staphylococcus, the bacillus coli communis, the tubercle bacillus, and the pneumococcus.
In the later stages, however, these organisms become inert, die, and disappear, so that in the majority of cases of chronic pyosalpinx the pus is found to be bacteriologically sterile. Observation on this subject made by a number of investigators shows that out of 133 cases of acute and chronic suppuration of the uterine appendages in which the pus was examined bacteriologically, 285 no organisms whatever were found in 82 cases; in other words, the pus was sterile in about 61 per cent. of the cases. The pyosalpinx in time, therefore, becomes inert so far as any active inflammatory action is concerned, and resembles a chronic abscess in other parts of the body. Active inflammatory action may, however, be excited at any time, as in other chronic abscess, by a new infection, septic organisms entering the abscess by way of the uterine cavity, an adherent loop of intestine, or the bladder. The woman will then have an attack of acute septic inflammation in the old pyosalpinx, and will be exposed to the various dangers that were imminent during the primary acute stages of the disease.

Fig. 149.—Hydrosalpinx, showing complete inversion of the fimbriæ.
It seems probable that if the woman survive the dangers to which she is exposed from a pyosalpinx, the tumor may in time become converted into a hydrosalpinx. The solid constituents of the fluid become absorbed or deposited upon the cyst-walls, and a clear watery fluid remains. In hydrosalpinx the recesses of the tube are often found to contain cheesy material and cholesterin—remnants of the old purulent accumulation. The tubo-ovarian cyst is formed in this way from a former tubo-ovarian abscess.
Hydrosalpinx.—The fluid in a hydrosalpinx may be 286 colorless, slightly yellow, or brownish or chocolate colored from the presence of blood. As the accumulation increases, the walls of the cyst atrophy and become very thin. The epithelium and the mucous membrane atrophy and in time disappear, until nothing but a thin-walled transparent cyst remains (Fig. 149). The cyst-wall in hydrosalpinx is always thinner and more transparent than that in pyosalpinx. On the inner wall of the cyst delicate ridges corresponding to the plicæ or folds of mucous membrane may be traced. There may often be discovered, at the distal end of the retort-shaped tumor, a slight depression that marks the position of the abdominal ostium, while upon the inner aspect of this depression may be found the remains of the invaginated fimbriæ. The size of the tube in hydrosalpinx varies from that of the little finger to a tumor as large as the fetal head. Large hydrosalpinx tumors are very unusual, because the fluid probably leaks slowly through the thin cyst-wall, and because the secreting surface of the cyst becomes destroyed by pressure. The fluid from a hydrosalpinx is sterile, unirritating to the peritoneum, and is readily absorbed. The cyst may rupture spontaneously or as the result of some slight accident; the fluid will be absorbed by the peritoneum, and only the shrivelled, atrophied sac will remain. In old cases of this kind the Fallopian tube is represented by an impervious cord. Such specimens have often been found in old prostitutes who have survived the dangers of their calling.
Hematosalpinx.—True hematosalpinx, a closed Fallopian tube distended with blood, is a rare condition. Tubal pregnancy is the usual cause of an accumulation of blood in the Fallopian tube, but the term hematosalpinx should not be applied to this condition. True hematosalpinx occurs when, from any cause, hemorrhage takes place into a tube that had previously been closed by inflammatory action. Such an accident may be caused by traumatism or by torsion of the pedicle of a tubal cyst. Slight hemorrhages of this kind occur in pyosalpinx and 287 in hydrosalpinx, and cause the brownish discoloration that is sometimes seen in the contents of these tumors.
The various forms of inflammatory disease of the tubes that have been described under names which designate the gross appearance of the disease are all really but different manifestations of the same primary condition. Gonorrheal or septic infection may produce any of the forms of tubal disease that have been mentioned. Interstitial salpingitis without closure of the ostium, pyosalpinx, hydrosalpinx, hematosalpinx, tubo-ovarian abscess, etc. are not distinct diseases, but are different manifestations of the same disease, representing different stages of progress or different methods of development. Several of these different forms are often found in the same woman. On one side there may be a hydrosalpinx, on the other a pyosalpinx, both caused by a primary chronic gonorrhea; the distal end of one tube may be distended by a clear watery fluid, forming a hydrosalpinx, while the isthmus may be distended with pus, forming a pyosalpinx; a hematosalpinx may be formed on one side, while a tubo-ovarian abscess exists on the other; and so through a great variety of combinations.
Pyosalpinx with active septic contents represents the early stages of tubal disease, or it represents a chronic condition in which reinfection has occurred. Pyosalpinx with sterile pus is like a chronic abscess anywhere else, and represents a chronic form of salpingitis that had been active and purulent in the beginning. Hydrosalpinx represents the disease less violent and septic in the beginning, and slow in progress; or it represents the last stages of an old pyosalpinx; while, finally, hematosalpinx represents a condition of salpingitis in which some accident has befallen the cystic tube and caused hemorrhage into its cavity.
The description given shows the progress, the dangers, and the terminations of salpingitis.
The disease is caused by extension of inflammation from the endometrium. The usual causes of this inflammation 288 are gonorrhea, or infection after a criminal abortion, a labor, or a miscarriage. The gonorrheal salpingitis is usually slow or insidious from the beginning. The symptoms of the disease are often not troublesome until many months after the primary gonorrheal infection. The closure of the tube is slow, and it is sometimes not until the tube becomes distended with pus that the woman experiences much suffering and is placed in imminent danger. There are cases, however, of acute gonorrheal salpingitis in which the disease is virulent and active from the beginning. Infection may traverse the tube, reach the peritoneum through the open ostium, and produce general peritonitis within a few days of the primary attack of gonorrhea. In such cases it is probable that the infection is a mixed one, other organisms accompanying the gonococcus. In other cases the abdominal ostium becomes quickly closed and a gonorrheal tubal abscess is rapidly formed.
The septic variety of salpingitis, as has already been said, is more frequently acute from the beginning. Within ten days or two weeks after a criminal abortion, or after a miscarriage or labor, a large tubal abscess may be formed; or the septic organisms may pass through the tube before the ostium has been closed, and produce within a few days a general fatal peritonitis.
On the other hand, septic salpingitis is often slow, a mild attack of puerperal sepsis being the beginning of years of invalidism, of gradually increasing suffering, until gross tubal disease is produced.
The slowest forms of salpingitis are those that result from chronic endometritis, such as accompanies subinvolution, laceration of the cervix, retro-displacements, or uterine fibroid. Simple catarrhal salpingitis is often found in these diseases; or the abdominal ostium may be closed, and a small hydrosalpinx will be present; or the isthmus may be sufficiently open for drainage, and no tubal distention result. Hydrosalpinx is very often found with uterine fibroids. 289
Cancer of the cervix or the body of the uterus is a frequent cause of salpingitis, of hydrosalpinx, and of pyosalpinx. The endometrial inflammation secondary to the cancer extends into the tubes.
The progress of salpingitis is beset with danger.
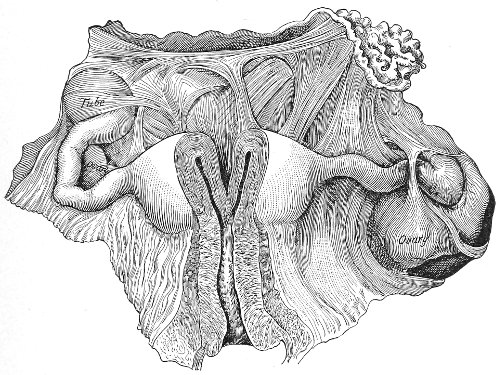
Fig. 150.—Chronic salpingitis with general adhesions of tubes, ovaries, and uterus (Bandl).
At any time a pyosalpinx may rupture and a rapid fatal peritonitis result. Unusual effort, vaginal examination, or slight operations upon the cervix or body of the uterus may cause this accident. Not infrequently, such rupture has been produced by even gentle bimanual examination. I have seen a fatal peritonitis occur from rupture of a pyosalpinx during the replacement of a prolapsed uterus.
For this reason the operator should always determine by careful examination the presence or absence of tubal disease in every case before performing any of the minor gynecological operations or manipulations, such as trachelorrhaphy or the replacement of a retroverted uterus. 290 Purulent disease of the tubes is a contraindication to all such procedures, unless an immediate subsequent celiotomy is to be performed. Great care must be exercised in any of the less dangerous forms of salpingitis. In any case of salpingitis, however mild, an acute attack may be excited by reinfection or by rough manipulation.

Fig. 151.—Chronic salpingitis: both Fallopian tubes are closed and adherent.
Rupture into the peritoneum is not the only danger to which the woman is exposed in salpingitis. The gradually formed adhesions in the pelvis impede the motion of the pelvic intestines and may cause intestinal obstruction. Obstruction of the ureters has occurred from pelvic inflammation. The Fallopian tube may discharge its contents through the bladder and produce violent cystitis, or it may discharge through the rectum or intestine, or adhere to the side of the vagina and discharge through this channel; or it may be evacuated through the abdominal parietes. Such fistulous openings rarely, if ever, close spontaneously and permanently. Temporary closure may occur, but the tube will refill and discharge as before.
Fistulæ of this kind persist for many years, becoming 291 seats of tuberculosis or exhausting the woman by the continuous suppuration.
If the patient escape these dangers, the disease may become quiescent. Some of the less dangerous forms of salpingitis are produced, until finally, when the woman has reached middle life, a hydrosalpinx remains, or an adherent, atrophied, cord-like remnant of the tube. Though then freed from the various dangers that had threatened her life, she is not restored to health, but remains a suffering invalid.
Salpingitis may be unilateral or bilateral. It is more likely to be unilateral in the acute cases than in the chronic, for, as the primary focus of the disease exists in the body of the uterus, it will extend in time to the second tube in case only one had at first been involved. If the endometrial disease is cured before the second tube has been attacked, the salpingitis may remain unilateral. Double salpingitis is especially likely to occur in those diseases of the endometrium that are difficult or impossible to eradicate—diseases like chronic gonorrhea, where the infection lurks in the distal ends of the utricular glands and defies our methods of treatment. Operators have repeatedly removed a unilateral pyosalpinx, leaving the second tube apparently perfectly healthy, and yet, after the lapse of a few months, a second operation has been necessary for the relief of a similar pyosalpinx on the other side.
Symptoms of Acute and Chronic Salpingitis.—The symptoms of acute salpingitis are usually obscured by the accompanying symptoms of endometritis, ovarian congestion and inflammation, and localized peritonitis. The woman complains of pelvic pain and tenderness, which are most severe in one or both ovarian regions. There are elevation of temperature and rapid pulse. The knees are often drawn up as in peritonitis.
Bimanual examination reveals marked tenderness upon pressure in the vaginal fornices. There is an indistinct sense of fulness in the region of the tubes. If the pelvic 292 peritoneum and cellular tissue are involved, the whole vaginal vault will feel full and resistant. The tissues lying to the sides and behind the uterus are thickened and resistant. If the woman is thin and there is not much surrounding inflammation, it is sometimes possible to palpate the enlarged tender tube between the vaginal finger and the abdominal hand. Usually, however, the tenderness is too great to permit this. The tube, from its increase in weight, may fall below its normal level, and may be felt lying behind the uterus in Douglas’s pouch.
Usually, in cases of acute salpingitis, the examiner is obliged to content himself with the determination of an indistinct fulness and marked tenderness in the region of the Fallopian tubes.
Before the true pathology of salpingitis was known these cases were described as pelvic peritonitis or pelvic cellulitis. It was supposed that the inflammation involved the peritoneum of the pelvis or the cellular tissue of the broad ligaments. It is true that this is often the case, and that inflammation of these structures accompanies the salpingitis, but it is the tubal inflammation which is the primary disease.
The most pronounced symptom of chronic salpingitis is pain. The pain is referred to one or to both ovarian regions as the disease is unilateral or bilateral. It is due not only to the salpingitis, but to the accompanying ovaritis. The pain is continuous. It is relieved by the recumbent posture, and is increased whenever the woman is upon her feet or is performing any work. The pain is increased by a jolt or sudden movement, by defecation, often by urination and by coitus. The pain during coitus, from direct pressure, is often so great that marital relations are abolished. I have seen a woman with salpingitis who was obliged to take a dose of morphine before every act of defecation. The pain from the jolting of a carriage often renders riding impossible.
The pain is dull and aching in character or sharp and 293 lancinating. It may extend down the anterior aspect of the thighs.
The pain is very much worse at each menstrual period. All the genital structures become congested and swollen at this time, and such phenomena, occurring in the adherent inflamed tubes and ovaries, often cause unbearable pain. The dysmenorrhea in salpingitis is usually very characteristic. It begins several days—sometimes a week—before the bleeding appears. It starts in one or both ovarian regions, and radiates thence throughout the pelvis and down the thighs. It will be remembered that the dysmenorrhea of anteflexion begins only a few hours before the bleeding—that the pain is usually situated in the center of the lower abdomen, in the region of the uterus, is expulsive in character, and is relieved when the bleeding has become well established.
The dysmenorrhea of salpingitis usually lasts throughout the whole of the period.
The pain of salpingitis persists throughout the whole course of the disease. It is common to all forms of salpingitis, and seems to bear no relation to the gross character of the lesions of the tubes. The pain and the dysmenorrhea are often as marked in a case of salpingitis without cystic distention as in a case of large pyosalpinx.
The pain persists after the dangerous stages of the disease have been passed. Relief begins only with the cessation of menstruation, when general atrophy takes place in the genital organs.
The pain of salpingitis is often obvious from the expression and the posture of the woman. She walks with the body slightly flexed forward; she sits down gently upon a chair; she protects herself, by support with the hand, from the jolting of a carriage or a car.
The woman frequently suffers with marked exacerbations of the pain, which occur independently of the menstrual periods, and are caused by leakage from the tube and the resulting local peritonitis. The woman often describes such attacks as attacks of “inflammation of the 294 bowels.” They occur usually during the early stages of the disease. Each attack, if survived, results in a more perfect closure of the ostium abdominale, and diminishes the risk of subsequent attacks. At these times all the symptoms of local peritonitis are present: elevated temperature, rapid pulse, local or general distention, and tenderness. In any case of pyosalpinx or of old chronic salpingitis close questioning of the patient will elicit a history of this kind.
Acute attacks of pain, fever, and other disturbance also occur in cases of chronic salpingitis from acute reinfection of the diseased tube. The disease may have been quiescent for a long time, and yet active reinfection may take place by way of the uterine cavity or by the passage of the colon bacillus through an adherent intestinal wall; or infection may occur through an adherent bladder.
Salpingitis is usually accompanied by menorrhagia. It is impossible to determine how much of this is to be attributed to the tubal disease. There is always an accompanying endometritis which is sufficient to account for it.
Sterility is the rule in cases of salpingitis. The disease of the mucous membrane and the destruction of the ciliæ render the passage of the ovum into the uterus difficult. For this reason tubal pregnancy may occur in salpingitis, impregnation and attachment of the ovum taking place within the tube. Inflammation of the ovary, which prevents the rupture of the ripened ovarian follicles, is another cause of the sterility. When the abdominal ostia are closed absolute sterility is present.
In chronic salpingitis the condition of the Fallopian tubes is revealed by bimanual examination. The tube usually falls below its normal level, and may be felt by the vaginal finger lying beside the uterus, or behind it, in Douglas’s pouch. By careful palpation the connection of the tubal tumor with the uterus may be traced. Bimanual examination is most satisfactory in the quiescent 295 stages of the disease. During an exacerbation or during one of the acute attacks of inflammation the tenderness prohibits thorough palpation, and the surrounding inflammatory infiltration masks the condition of the tube. The tube may be felt as a hard cord, or as a cystic tumor with the ovary lying in its concavity, or as a tortuous, sausage-shaped mass.
In old chronic cases the tube and ovary may be felt as a hard, knot-like mass adherent to the side of the uterus or coiled about the cornu (Fig. 151).
In nearly every case the isthmus is rendered hard and cord-like by inflammatory infiltration. This indurated condition of the isthmus is a feature of tubal disease that is usually readily determined, and it is of decided diagnostic value. The connection, by such a cord, of the mass felt in the pelvis with the uterine cornu is the most valuable proof that the tumor is tubal in character.
Diagnosis.—The diagnosis of chronic disease of the Fallopian tubes must be made from a study of the history, the symptoms, and by physical examination.
The history is always of value. Careful questioning will usually show that the ovarian pain dates from a criminal abortion, from an attack of fever after a miscarriage or labor, or from a suspicious coitus. Women who have been infected with chronic gonorrhea by their husbands attribute the origin of the disease to their marriage. The woman will often say that for some days after marriage she suffered with irritation and burning of the external genitals, with dysuria, perhaps with a slight vaginal discharge, and that after this, very gradually, the ovarian pain developed. She may have had one child or a miscarriage, but with this exception is usually sterile.
The history of attacks of local peritonitis, confining the women to bed for several days or weeks, can also usually be obtained.
The character and the situation of the pain and the character of the dysmenorrhea usually point strongly to 296 salpingitis. The physical examination is not by any means always satisfactory. The small flaccid tubal tumors are often difficult to palpate, especially in fat women, and the gross forms of the disease may be obscured by surrounding adhesions and inflammation. The examination, however, when taken in connection with the history and the symptoms, will usually enable one to make the diagnosis. Inflammatory tumors in the female pelvis are very generally tubal in origin.
It is difficult to estimate the mortality of salpingitis. It is certainly a frequent cause of death—not only immediately, by some of the acute accidents that may occur, but as a result of gradual exhaustion from prolonged suppuration. Acute salpingitis, and the purulent forms of the disease, should always be viewed with anxiety. As appendicitis is the usual cause of peritonitis in man, so is salpingitis the usual cause of this disease in the woman. In every case of peritonitis in a woman, therefore, careful examination of the pelvic organs should be made.
Salpingitis is an exceedingly common disease. It occurs in all classes of society, but most frequently in the lower walks of life. Salpingitis is the rule in prostitutes, and in them is caused by gonorrhea or by septic infection at criminal abortion.
Treatment.—The treatment of acute salpingitis in its early stage should be expectant: absolute rest in the recumbent position, vaginal douches of a gallon of hot sterile water (100°-110° F.) two or three times a day, small doses of saline purgatives (Rochelle salts, ʒss-ʒj every one or two hours) until mild purgation is produced, should be prescribed, and should be continued as required. Relief of pain is afforded by hot fomentations over the lower abdomen. It is best to administer no opium, as it is very important to watch these cases closely, and the symptoms that demand operation might be masked by the administration of an anodyne. Examinations should be made with great care and gentleness, and no oftener than is necessary to determine the progress of 297 the disease. If the patient is progressing satisfactorily, repeated examinations are contraindicated.
A chill followed by a rapid high elevation of temperature (105°-106° F.) is often caused by even gentle manipulation of the upper organs of generation in cases of acute inflammation.
The case must be watched carefully and continuously. In the gonorrheal and septic forms of the disease there is great danger of extension to the peritoneum, or of the formation of a tubal or other form of pelvic abscess that will imperil the life of the woman.
As a general rule, it may be said that, unless there are well-marked symptoms of extensive pelvic peritonitis, or unless a distinct tumor can be felt in the pelvis, operation is not indicated. As resolution undoubtedly takes place even after severe acute attacks of salpingitis, it is right to treat the woman with this end in view rather than to resort to an immediate mutilating operation.
If, under the expectant plan of treatment, the patient does not improve; if the area of pelvic tenderness increases; if the local tympany (which may at first be present only on one or both sides of the pelvis, and which indicates merely local peritoneal irritation or inflammation) extends upward; if the temperature and pulse-rate increase; if constipation appears; if, in fact, indications of extension of the peritonitis are present,—celiotomy should be immediately performed. The diseased tube or tubes should be removed, and, if necessary, the abdomen should be drained.
Fatal peritonitis sometimes results within three or four days after the onset of acute salpingitis. As soon, therefore, as the physician realizes the imminence of this complication in any case, he should not delay in removing the source of infection.
The other acute termination of salpingitis, the formation of an abscess in the pelvis, likewise demands operative interference. This condition is readily recognized. The woman has one or more chills. The temperature 298 becomes more elevated and the pulse more rapid. The pelvic tenderness and pain may become more distinctly localized to one or both ovarian regions. Defecation and urination increase the pain. Bimanual examination reveals an exceedingly tender mass, either indurated or perhaps soft and fluctuating, lying to either side of, or behind the uterus. The character, upon palpation, of the mass depends upon the nature and extent of the peritoneal adhesions that surround it. The diagnosis of a pelvic abscess resulting from acute salpingitis is usually easy.
There is some difference of opinion among operators in regard to the best treatment for this condition. Some advise evacuation of the abscess by way of the vagina; others advise celiotomy, with removal of the abscess and the Fallopian tube that caused it, followed, if necessary, by abdominal or vaginal drainage. I prefer the latter method of treatment, for reasons that will appear under the consideration of the technique of operation.
Treatment of Chronic Salpingitis.—Cases of simple chronic catarrhal salpingitis undoubtedly recover after the cure of the endometrial disease of which the salpingitis forms a part. The tube may be restored perfectly to its normal condition; or there may remain an atrophic condition of the mucous membrane; or the fimbriæ may be left somewhat distorted, crumpled, or slightly drawn within the tube; or there may be a few fine peritoneal adhesions, like cobwebs, between the distal end of the tube, the broad ligament, and the ovary. Such slight lesions may cause no trouble beyond interfering a little with the fecundity of the woman.
When, however, the adhesions are more extensive, treatment for their relief may be demanded, even though all inflammatory action has disappeared from the body of the uterus and the tubes. Treatment in such cases is demanded, not to cure the salpingitis or on account of any danger that threatens the woman’s life, but to relieve the pain caused by the results of the inflammation. 299
It may be necessary to perform celiotomy in order to free or break up adhesions that bind down the ovary in an abnormal position, or to liberate an adherent intestine, or to replace a uterus that has been displaced by the traction of adhesions.
The degree of suffering experienced by the woman is the guide in advising such operative interference.
Pelvic massage has been used for the relief of pelvic adhesions of this kind, the uterus, tubes, and ovaries being manipulated between the fingers in the vagina and a hand upon the abdomen. The results of this treatment have not been encouraging.
In discussing the treatment of chronic salpingitis the cases may be divided into two classes: those in which palliative treatment may be followed, and those in which operation is demanded.
There are a great number of cases of chronic salpingitis in which there is no gross disease of the tubes, and in which operation upon the tubes is not immediately indicated. It is proper in such cases to try milder palliative treatment first.
Salpingitis is always preceded, and usually accompanied, by inflammation of the endometrium, and in every chronic case attention should first be directed to the cure of the endometritis.
If there is no tubal and ovarian displacement—that is, if the ovary is not prolapsed; if the uterus has not been retroverted; if there are no extensive tubal adhesions; and if there is no gross disease of the tube, such as pyosalpinx, hydrosalpinx, hematosalpinx, a thorough curetting of the uterus, or, if necessary, a trachelorrhaphy or an amputation of the cervix, will often relieve the woman of her suffering, and it may not be necessary to operate for the damaged tubes.
In all such cases, however, the operator must be very careful to exclude active or purulent tubal disease. If he overlooks a pyosalpinx, the curettage or the trachelorrhaphy may be followed by an active peritoneal inflammation that will destroy the woman. 300
If there is ovarian or uterine displacement, we cannot expect relief until these conditions have been treated, and such treatment usually requires celiotomy.
The pain and dysmenorrhea of chronic tubal disease may be relieved by rest in the recumbent position during the menstrual period; by the administration of saline laxatives (the pain is always increased by constipation); by vaginal douches of large quantities of hot water (one gallon at 110° F.) administered two or three times a day in the recumbent posture; and by applications of Churchill’s tincture of iodine to the vaginal vault, and the use of the glycerin tampon. The directions for this treatment have been given under the preparatory treatment of laceration of the cervix.
Such treatment is only palliative: it relieves the pain, but it will not cure well-established chronic salpingitis.
In many cases the woman experiences little, if any, relief from this treatment. In other cases, though the pain may be very much relieved while she is taking treatment, yet it returns as soon as the treatment is stopped, and she becomes unwilling to lead the life of an invalid under constant medical care, with but little prospect of relief until the menopause is reached. It is then necessary to consider operation.
The second class of cases referred to—those in which immediate operation is demanded, and in which it is dangerous to delay and useless to try the palliative treatment—includes a great variety. Such cases are—the gross forms of tubal disease, hydrosalpinx, hematosalpinx, and pyosalpinx; salpingitis with prolapsed and adherent tube and ovary; salpingitis with retrodisplacement of the uterus; all the milder forms of salpingitis which have resisted palliative treatment.
The operative treatment of salpingitis usually demands celiotomy. Some operators, however, prefer to reach the uterine appendages by way of the vagina.
The details of the operative technique of salpingo-oöphorectomy will be given in a subsequent chapter. As 301 a rule, the operation of celiotomy for salpingitis should always be immediately preceded by thorough curetting of the uterus and, if necessary, by trachelorrhaphy or an amputation of the cervix.
After the abdomen has been opened the operation consists in freeing adhesions, rendering patulous the abdominal ostium of the tube, replacing the uterus, and, if necessary, removing the tube and ovary on one or on both sides.
Removal of the tubes and ovaries—salpingo-oöphorectomy—is usually necessary. In pyosalpinx this operation should always be performed. If the woman is young and is very anxious to have children, every attempt should be made to save, at any rate, one tube and ovary. Remarkable cases of conception have occurred after conservative operations upon badly diseased tubes.
The adhesions about the abdominal ostium may be broken and the imprisoned fimbriæ freed; or if the ostium is firmly closed, an incision may be made in the wall of the tube, the peritoneum stitched to the mucous coat, and a new ostium produced. In one case conception followed such an operation in which the ovary was sutured in the artificial opening made in the tube. Conception has occurred after both tubes had been amputated at the uterine cornua.
In all such conservative operations, however, the woman should be told of the probability of failure and the probable necessity for a subsequent radical operation. The successful cases show the possibilities of surgery, but, unfortunately, they are exceptional. Sterility usually continues, the pain is usually unrelieved, and a second radical operation becomes necessary.
Such conservative operations upon badly diseased tubes should be performed, therefore, only when the woman is young and anxious for children. Whenever the abdominal ostium is closed and the ovary is adherent, it is safest to perform a complete salpingo-oöphorectomy. This is always indicated when the woman is near the 302 menopause or when immediate certain relief is demanded from prolonged suffering.
In some cases the question arises as to whether both tubes should be removed when only one is grossly diseased. In the early stages of chronic pyosalpinx it often happens that but one tube is found diseased, while the other is apparently perfectly healthy or is only slightly adherent. Experience has shown that in a great many cases of tubal disease in which only one tube was removed, the second tube has become similarly affected, often within a short time, and a second operation has been required. This disaster is not likely to occur if the endometrial disease is eradicated by thorough curetting at the time of the first operation. But in some forms of salpingitis, as the gonorrheal, the infection is so deeply seated in the distal ends of the utricular glands that the most vigorous curetting fails to remove it, and the second tube will become infected from the original focus in the uterus.
So common is such occurrence that many women, profiting by the experience of their friends, request the operator to remove both tubes, even though he finds but one diseased. The advice already given in regard to conservative operation applies here also. It is safest in all forms of pyosalpinx to remove both appendages. In the less serious forms of salpingitis—hydrosalpinx and adherent tubes without cystic distention—there is less danger of recurrence, and the unilateral operation may be more safely performed. The importance of thorough treatment of the endometritis at the same time is emphasized by these considerations.
In many cases in which double salpingo-oöphorectomy is performed it is often advisable to remove the uterus at the same time. The uterus may be amputated at any convenient point of the cervix, or it may be completely removed at the vaginal junction. This operation ensures more certain and speedy relief from suffering, and is attended by but little, if any, greater mortality than the 303 simple salpingo-oöphorectomy. The uterus without the tubes and ovaries is a useless structure. The operation is advisable if the uterus is retroverted and adherent, when the uterus is large and subinvoluted, when the disease of the endometrium is severe and is likely to persist—in any case, in fact, in which the physician fears that the uterus may be a subsequent source of trouble.
Pus in the female pelvis, to which condition the vague term of pelvic abscess has been applied, is usually the result of salpingitis producing a pyosalpinx, of ovarian abscess, or of suppuration of an ovarian cyst, very often a dermoid. The disease may also occur from infection of a broad-ligament hematoma or from a pelvic hematocele caused by a ruptured tubal pregnancy.
Following these conditions the cellular tissue of the pelvis may become affected, so that the purulent accumulation may make its way between the layers of the broad ligament or in some other part of the pelvis.
Before the days of modern abdominal surgery these accumulations of pus were evacuated through the vagina, the rectum, or the abdominal wall, according to the direction in which the abscess seemed to point or in which it seemed to be most accessible. The sinuses thus formed often persisted for years or during the remaining life of the woman. There were many theories in regard to the origin of the suppuration, it being impossible to determine its true nature without opening the abdomen. Now we know that the great majority of such pelvic abscesses originated in septic infection of the Fallopian tubes, and that infection of the pelvic cellular tissue was secondary.
There are, however, rare cases in which the suppuration occurs primarily in the cellular tissue of the pelvis, without any involvement whatever of the tubes or ovaries. Such an accumulation of pus is usually found in the cellular tissue of the broad ligaments; it sometimes 304 occurs in the utero-vesical tissue, and rarely in the tissue back of the cervical neck.
The cause of such suppuration is usually infection, by way of the lymphatics, from the uterus, or by the passage of septic organisms directly through the uterine wall. The condition is most frequently the result of puerperal sepsis. I have on one occasion seen it occur in connection with extensive venereal ulceration of the external genitals. It seems probable that a pelvic lymphatic gland, becoming infected, may break down and suppurate, forming the starting-point of the abscess.
The symptoms of this form of pelvic abscess are those characteristic of any other kind of suppuration in the pelvis.
The purulent accumulation may be detected by bimanual examination. It usually bulges into the vagina at the lateral fornices or before or behind the cervix. The abscess-mass is in close relationship with the uterus. In this respect it differs from a simple tubal or an ovarian abscess, in which cases a distinct separation of the tubal or ovarian tumor from the uterus may be determined, at any rate, before the pelvic cellular tissue has become involved.
If the abscess bulge in the anterior vaginal fornix, it is very probably of neither tubal nor ovarian origin, as tubal and ovarian abscesses lie to the side of, or behind, the uterus.
The sense of fluctuation is often difficult or impossible to determine. The infiltration of the surrounding structures gives to the mass a dense hard feeling that obscures fluctuation. To the experienced finger, however, this indurated condition of the tissues is characteristic of pelvic suppuration, as is the sense of fluctuation elsewhere.
The treatment of pelvic suppuration of this nature is evacuation by way of the vagina. The incision should be made into the most prominent part of the mass. When made into the lateral fornices, the operator should 305 remember the position of the ureters and the uterine arteries. The ureters lie a little over half an inch from the cervix. In every case it is safest to make the incision close to the cervix and to work carefully into the abscess-cavity. The pus should be evacuated, and a double drainage-tube should be introduced for subsequent washing.
In most cases, however, the physician cannot determine with any certainty that the abscess is simply confined to the pelvic cellular tissue and did not originate in the Fallopian tube. If there is any doubt of this kind, celiotomy should be performed and the true nature of the condition determined. If a pyosalpinx or an ovarian abscess is present, as is usually the case, the condition may be dealt with as has already been advised. If the uterine adnexa are healthy, the abdomen may be closed and a subsequent vaginal incision may be made.
Indiscriminate evacuation of collections of pus in the pelvis by way of the vagina has resulted in a great deal of harm. The abscess, being usually of tubal origin, often persists indefinitely. Intestine, ureters, bladder, and blood-vessels have often been injured; and when subsequent celiotomy is performed the operation is attended with great danger from the presence of the fistulous opening. 306
Tuberculosis attacks the Fallopian tubes much more frequently than any other part of the genital apparatus. The disease may be associated with tuberculosis of the peritoneum or with tuberculosis of the ovaries and the uterus. As has already been said, tuberculosis of the uterus often originates in the tubes and extends thence to the endometrium.
The tubercular Fallopian tube varies much in appearance according to the nature and stage of the disease. The strictly tubercular lesions may be masked by those of ordinary inflammation. There may be peritoneal adhesions, often very dense and widespread, between the tube and adjacent organs, and the ostium abdominale may be closed, as in non-tubercular salpingitis.
In some cases these simple inflammatory adhesions probably existed before the tubercular infection took place, the tuberculosis occurring in an old diseased tube. In other cases it is probable that the inflammatory adhesions and products occurred as a result of the tuberculosis, which attacked a tube previously healthy. In the latter case such adhesions may be viewed as a conservative process.
The tubercular tube is often very much enlarged from infiltration of its walls and dilatation of its lumen. It may be filled with typical caseous material, and when this is removed the mucous membrane will be found the seat of deep, jagged, ulcerated areas.
If the abdominal ostium is not entirely closed, the cheesy material may project into the abdominal cavity. 307 If the disease has extended to the peritoneal coat, the covering of the tube will be found studded with typical tubercles (Fig. 152). Such tuberculosis of the peritoneum may be confined to that covering the tube, or it may extend to the uterus and throughout the abdominal cavity.
In peritoneal tuberculosis that has originated in the tube the lesions are found to be most widespread in the pelvic peritoneum.
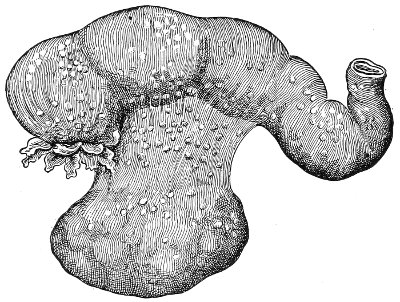
Fig. 152.—Tuberculosis of the Fallopian tubes. The disease has extended to the peritoneum, which is covered with tubercles.
In some cases the ostium becomes closed, and the tubes are found distended with pus, forming tubercular pyosalpinx. Such tubes sometimes attain enormous size, containing a quart or more of purulent material.
In less extreme cases than those just described the tubercular area may be limited to a portion of the tube, and gives rise to one or more nodular enlargements (Fig. 153). In other cases there is no gross change in the shape or size of the tube, and only a few miliary tubercles are found scattered throughout the mucous membrane.
In a very large number of the cases of tuberculosis of the Fallopian tubes, the lesions resemble in all respects those of ordinary salpingitis, and are not in any way recognizable by the naked eye as characteristic of tuberculosis. 308 There are no cheesy contents; there are no tubercles upon the peritoneum; the mucous membrane shows no macroscopical changes that would lead to the suspicion of tuberculosis. In these cases the tubes are usually closed at the abdominal ostium; there may or may not be cystic distention; and the adhesions, which are usually very firm, distort the shape of the tube and bind it to the posterior aspect of the broad ligament, the uterus, or other pelvic structure. Until recent years such cases were supposed to be simple cases of salpingitis. Careful microscopic examination, however, has shown that this forms one variety of tubal tuberculosis, and that a certain proportion of such cases of salpingitis are tubercular. The term “unsuspected tuberculosis” has been applied by Williams to such cases.
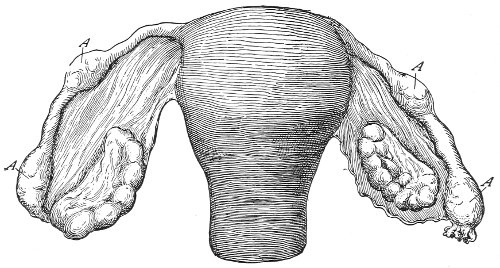
Fig. 153.—Tuberculosis of the Fallopian tubes: A, tubercular nodules.
Cases of tuberculosis of the Fallopian tubes may be divided into three classes: Miliary tuberculosis; chronic diffuse tuberculosis (cheesy tubes); and chronic fibroid tuberculosis.
Miliary tuberculosis of the tubes may be a part of a general miliary tuberculosis, or it may occur primarily in the tube. Microscopic examination shows giant epithelioid cell-tubercles scattered throughout the mucous membrane. 309
Miliary tuberculosis is the first stage of tuberculosis of the tubes. The process may progress no farther, or it may become converted into one of the other varieties.
In chronic diffuse tuberculosis the mucous membrane is infiltrated with epithelioid cells, miliary tubercles, and areas of caseation. The tube may be filled with cheesy material or with pus, and in time the mucous membrane becomes completely destroyed. In this form of tuberculosis the gross appearances are usually characteristic, and are those which have already been described.
In chronic fibroid tuberculosis there is a great increase of connective tissue between the tubercles. The lumen of the tube is distorted, and a few miliary tubercles are found scattered through the mucous membrane. This form of the disease is very slow and chronic, and represents a usual method of spontaneous cure.
Since the discovery of so-called unsuspected tuberculosis of the Fallopian tubes the disease has been found to be much more frequent than was formerly supposed.
Williams found tuberculosis of the tubes in one out of every twelve operations for the removal of tubes and ovaries that were the seat of past or present inflammatory disease.
Dr. Beyea and I have found tuberculosis of the tubes present in 18 per cent. of the cases that were subjected to the operation of salpingo-oöphorectomy for inflammatory disease of the tubes.
It may be said, therefore, that tuberculosis is present in from 8 to 18 per cent. of all cases of inflammatory disease of the uterine appendages. It is impossible, however, to say whether or not tuberculosis is the cause of the disease in all cases, or whether tuberculosis has been grafted upon a previous non-tubercular affection. Other organisms, along with the tubercle bacillus, are frequently found in the Fallopian tube.
Tuberculosis of the Fallopian tubes may be primary or secondary.
In primary tuberculosis the tubes are the primary seat 310 of the disease, being affected before other structures of the body.
In secondary tuberculosis the tubes are affected from a tubercular focus in some other part of the body.
Tuberculosis of the tubes is usually secondary.
Infection takes place in a variety of ways. Infection through the blood is the most usual way.
Infection may take place from a tubercular ulcer of the intestine or bladder becoming adherent to the tube. The tube may become involved by extension of tuberculosis of the peritoneum to it. In many cases the reverse order happens: the tube is first involved by the tuberculosis, and the disease extends thence to the peritoneum. In other cases it is the peritoneum that is primarily affected. It seems probable that tubercle bacilli, having gained entrance to the peritoneum from a tuberculous mesenteric gland or from an intestinal ulceration, fall to the pelvis and are drawn into the Fallopian tubes, there producing tuberculous lesions without first affecting the peritoneum.
It seems probable that in a good many cases of tuberculosis of the tubes the infection takes place from without by way of the genital tract. Dirty instruments, syringes, or the examining finger may cause it in this way. Infection may also occur from clothing or bed-sheets soiled by sputum or other tubercular discharge. Coitus with men affected with genito-urinary tuberculosis or any other form of tuberculosis may be an occasional cause. It has been shown that tubercle bacilli may be present in the testes and prostate glands of consumptives without any evidence of genito-urinary tuberculosis being present.
Tubal tuberculosis may occur by way of the genital tract from infection from the discharges from some other tubercular focus in the woman, as in the lungs, bladder, or intestinal tract.
The symptoms of tuberculosis of the Fallopian tubes are not at all characteristic. Most cases of tubal tuberculosis 311 have been discovered at the autopsy or have been unexpectedly found at operation.
The symptoms resemble those of non-tubercular salpingitis. There is the same ovarian pain and dysmenorrhea. Bimanual examination reveals the enlarged or nodular and distorted condition of the tube. The adhesions are often very firm and dense, and the tubal tumor is often of stony hardness.
The diagnosis of uncomplicated tubal tuberculosis is difficult, and in many cases impossible. If the peritoneal covering of the tube is involved, the small tubercles may sometimes be felt by vaginal or rectal palpation. Or, if the condition has extended to the posterior aspect of the uterus, the tubercles may be felt here, by dragging the cervix down with a tenaculum and palpating the posterior uterine surface with a finger in the vagina or the rectum. The association of salpingitis with pulmonary tuberculosis would lead the physician to suspect that the salpingitis might be tubercular. If the woman has tuberculosis of the peritoneum, and the tubes are found enlarged, it is most probable that they are tubercular. A knowledge of a genito-urinary lesion of tubercular nature in the husband should lead us to fear tubal tuberculosis in the wife.
Prognosis.—Tubal tuberculosis is a dangerous disease. There are several methods of termination. It very often leads to tuberculosis of the peritoneum. For this reason peritoneal tuberculosis is more common in women than in men.
A tubercular abscess may be formed in the pelvis, and the woman may die as the result of prolonged discharge and suppuration, as in the case of non-tubercular pyosalpinx. General tubercular infection may arise from the tubercular focus in the tubes.
Tuberculosis of the tubes may, and probably often does, undergo spontaneous cure. The fibroid changes that have been described lead to this end. In some cases calcification occurs, as in tuberculosis elsewhere, and the 312 disease is cured in this way. Fig. 154 represents an old tubercular pyosalpinx that was filled with calcified plates.
Even though these conservative changes take place and all danger from the tuberculosis has disappeared, the woman will continue to suffer pain and dysmenorrhea from the tubal and ovarian adhesions.
Treatment.—The treatment of tubal tuberculosis is celiotomy, with removal of the tubes and ovaries. If the uterus is involved, it should also be removed. Removal of the tubes, however, is the important feature of the operation. I have seen perfect and permanent recovery occur after removing the tubes, even though the disease had extended into the uterine cornua. As the disease very rarely extends below the internal os, the uterus may be amputated at any convenient point of the cervix.
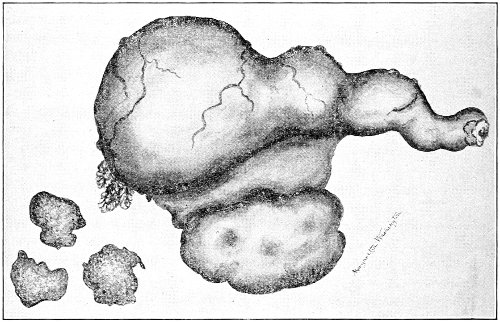
Fig. 154.—A tubercular pyosalpinx. To the left are three calcified plates that were found in the tube.
Tuberculosis of the peritoneum is an indication for, rather than a contraindication to, the operation. The most extensive cases of peritoneal tuberculosis have been cured by opening and draining the abdomen. If the tubes are rendered inaccessible from the involvement of surrounding structures, the operator must content himself with opening and draining the abdomen. 313
Adenoma of the Fallopian tube is a rare disease; but a few cases have been described in medical records. The presence of primary adenoma in the Fallopian tube is strong proof of the glandular character of the mucous membrane—an anatomical point which, as has already been said, has been denied by some writers. In adenoma the tube becomes distended with the typical adenomatous mass, which may protrude from the abdominal ostium.
In some of the reported cases there has been found a considerable quantity of free fluid in the peritoneum, though the peritoneum itself was not diseased. It seems probable that this secretion originated in the tube and escaped at the ostium.
Myoma.—Notwithstanding the frequency of myomatous tumors of the uterus, the condition is exceedingly rare in the Fallopian tubes. The tumors originate in the muscular coat, and are usually so small as to create no disturbance.
Cancer.—Primary cancer of the Fallopian tubes is an extremely rare disease. A very few isolated cases have been reported.
Cancer of the tubes secondary to cancer of the body of the uterus occurs more frequently.
Sarcoma of the tube is a very rare disease.
Actinomycosis of the Fallopian tubes has been described.
Syphilitic gummata occasionally attack the Fallopian tube in women who are the victims of constitutional syphilis.
The diagnosis of these unusual lesions of the Fallopian tubes is impossible with our present knowledge. The conditions have usually been found post-mortem or have been unexpectedly discovered at operation. The subjective symptoms throw no light upon the subject of differential diagnosis. Examination reveals merely a tubal tumor.
As the rule is to operate in all cases of tubal tumor, the proper treatment will probably be applied, notwithstanding the uncertainty or mistake of diagnosis. 314
Tubal pregnancy occurs when a fecundated ovum is developed in the Fallopian tube.
Fecundation may take place in the Fallopian tube, because spermatozoa may pass through the uterus and the tube into the pelvic cavity; but unless something occurs to arrest the passage of the fertilized ovum into the uterus, a normal uterine pregnancy will result. It is said by Webster that predisposition to tubal pregnancy is due to a “developmental fault, whereby there is reversion, either of structure or reaction tendency, in the tubal mucosa to an earlier type in mammalian evolution.”
In other words, decidual changes, following the fertilization of the ovum, may in some women occur in the mucous membrane of the Fallopian tubes as well as in that of the uterus. If this condition is present in any case, and at the same time something occurs to impede the passage of the ovum into the uterus, a tubal pregnancy may take place.
Interference with the passage of the ovum along the tube has been attributed to a variety of causes. Chronic salpingitis is a frequent cause. It destroys the cilia of the epithelial cells of the tubal mucosa. It produces thickening of the tubal walls, and causes peritoneal adhesions that impede the normal peristaltic action of the tube.
Obstruction to the passage of the ovum may also be caused by polypi or tumors of the tube; by tumors external to the tube pressing upon it; by displacement and hernia of the tube; by diverticula of the tube; or by abnormal foldings of the tubal wall. Tubal pregnancy has 315 occurred in tubes in which no lesions whatever could be discovered by the most careful examination.
It seems probable that practically all pregnancies that occur outside of the uterus originate in the Fallopian tube.
Pregnancy may occur in any part of the tube from the abdominal ostium to the uterus.
Tubal pregnancy is said to be infundibular when gestation begins in the infundibulum or in an accessory tube-ending. This variety has also been called tubo-ovarian, because in time the gestation-sac may become adherent to the ovary and be bounded by both tube and ovary.
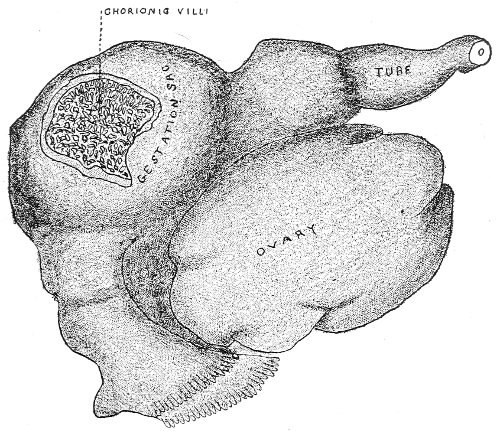
Fig. 155.—Tubal pregnancy, removed before rupture. The opening that has been cut in the tube shows the chorionic villi.
The pregnancy is said to be ampullar when gestation begins in the ampulla of the tube. This is the most usual seat of tubal pregnancy. It is called interstitial when gestation begins in the interstitial portion, or that part of the tube in immediate relationship with the uterus.
Changes in the Fallopian Tube.—During the early stages of tubal pregnancy—the first two or three months—it 316 seems probable that a certain amount of hypertrophy and hyperplasia of the muscular wall of the tube takes place. The general form of the tube is spindle-shaped (Fig. 155). There is a marked increase in the vascularity of the tube, most pronounced in the neighborhood of the ovum. The whole tube becomes turgid and swollen. The peritoneal margin or ring surrounding the ostium abdominale becomes prominent, and gradually, as has already been described under Salpingitis, projects beyond the fimbriæ, contracts, and ultimately hermetically closes the ostium.
Inflammation of the peritoneal covering of the tube may be present. Such inflammation may have preceded the tubal pregnancy or may have occurred as the result of the pregnancy. It produces various tubal adhesions and distortions, and may still more firmly close the abdominal ostium. The changes that take place in the mucous membrane of the tube and in the developing ovum are similar to those that occur in the uterus in a normal pregnancy.
A variety of terminations occur in tubal pregnancy:
I. In very exceptional cases the pregnancy may continue until full term, without rupture of the tube taking place.
II. The tube may rupture. This is by far the most usual occurrence. The rupture may take place into the broad ligament, into the peritoneal cavity, or, in the case of interstitial tubal pregnancy, into the uterus.
III. Tubal abortion may occur, the ovum being discharged through the abdominal ostium into the peritoneal cavity.
IV. The ovum may be destroyed in the tube, gestation being stopped before rupture takes place.
Rupture of the tube is the rule in tubal pregnancy. The time of rupture depends upon the position of the ovum in the tube. It occurs somewhat later in the interstitial variety than when the ovum is situated in the free portion of the tube. Rupture in interstitial pregnancy 317 commonly occurs before the fifth month. In the other forms of tubal pregnancy it occurs most usually before the end of the third month. In the latter class of cases the greatest number of ruptures occur during the second month.
Rupture is caused by the gradual thinning of the tube from distention. Rupture may take place suddenly, a large hole, through which the ovum escapes, being produced; or the rupture and discharge of the ovum may take place gradually without causing any acute symptoms.
When the rupture takes place between the layers of the broad ligament, the hemorrhage is usually not very profuse, as it is controlled by pressure of the structures that surround the blood. A broad-ligament hematoma is formed. The ovum may be destroyed as a result of the rupture, and no further lesions due to the development of gestation will arise. The hematoma, with the ovum, may in time be absorbed; or suppuration may occur, with the production of a pelvic abscess; or mummification, adipoceration, or lithopedion formation may take place in the fetus.
If the ovum is not destroyed by the rupture, it may continue to develop in the cavity formed by the tube and the broad ligament. The placenta may remain attached to the inner surface of the tube, or it may contract adventitious attachments to any of the surrounding structures—the surface of the uterus and the pelvic floor. The cavity occupied by the ovum may continue to enlarge, by the pushing aside of pelvic and abdominal organs, until full term is reached and spurious labor comes on.
In some cases a secondary rupture of the gestation-sac occurs, and the fetus is discharged into the peritoneal cavity.
When rupture of the tube into the peritoneal cavity occurs, the danger of fatal hemorrhage is very great. The majority of women die within forty-eight hours after this accident, unless relieved by immediate laparotomy. 318 There is no surrounding pressure to control the hemorrhage, as in the case of rupture into the broad ligament. Sometimes the escaping ovum plugs the rent in the tube, and bleeding is checked in this way.
If the woman survive the effects of hemorrhage, she may die from peritonitis or from suppuration of the hematocele in the peritoneal cavity.
In exceptional cases, if the pregnancy be early, the blood and the ovum may be absorbed by the peritoneum, and spontaneous recovery occurs.
If the woman is not destroyed by the first effects of the rupture, the fetus, surrounded by its membranes, may escape into the peritoneal cavity, while the placenta may remain attached to the tube and gestation may continue. It is very doubtful whether the fetus will continue to live if it escapes into the peritoneum free of the membranes. There is no evidence that an early ovum may escape into the cavity of the abdomen and develop on the peritoneum.
If the fetus does not survive, it may be absorbed by the peritoneum or mummification may occur.
Tubal abortion means the separation of the ovum from the tube-wall, and its partial or complete discharge through the ostium abdominale into the peritoneal cavity. The accident is accompanied by hemorrhage into the tube and thence into the peritoneal cavity.
Tubal abortion is most likely to occur during the early weeks of pregnancy (the first and the second months), before the abdominal ostium has become closed.
It is probable that tubal abortion is much more frequent than is generally supposed. According to Sutton, tubal abortion was probably the cause of the peritoneal hematocele in many cases in which the bleeding was attributed to other origin, as reflux of menstrual blood from the uterus and simple hemorrhage from the tube.
In tubal abortion the loss of blood into the peritoneum may be so great that the woman is destroyed. In other cases death results from peritonitis and suppuration of 319 320 the hematocele. And, finally, in a good many cases the blood and ovum may be absorbed, and recovery takes place. Sometimes, at operation, the ovum is found in the peritoneal cavity without any blood. The blood had either been small in amount and quickly absorbed, or there had been no escape of blood into the peritoneum. Blood-clot is usually found in the Fallopian tube after tubal abortion. The ostium may become closed and a hematosalpinx may result.
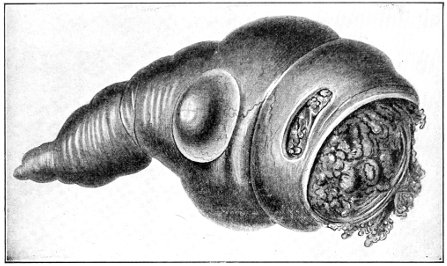
Fig. 156.—Extra-uterine pregnancy; tubal abortion. The bleeding is checked by a large coagulum distending and thinning out the tube; the fimbriated opening is greatly distended, but the greater diameter of the clot in the ampulla prevents its escape. Wall of tube averaging 1 millimeter in thickness. Operation. Recovery, July 7, 1896. Natural size. (Kelly. Copyright, 1898, by D. Appleton & Co.)
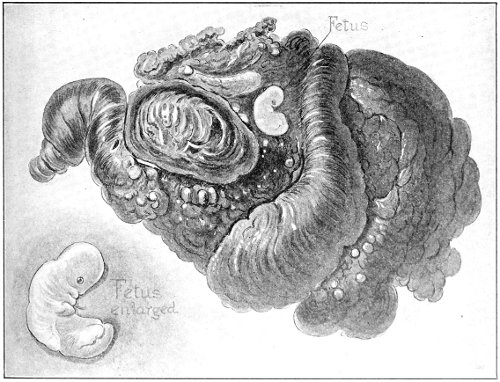
Fig. 157.—Coagulum turned out, showing a cast of the tube extending up into the isthmus. On its surface lies the fetus. Natural size. (Kelly. Copyright. 1808, by D. Appleton & Co.)
When the ovum is destroyed in the tube before rupture takes place, the fetus and the blood may be absorbed; or mummification, adipoceration, or lithopedion-formation may result; or suppuration may occur, with the formation of a pyosalpinx; or, if death of the fetus happens in the early weeks, the tube may be found closed at the ostium abdominale, and filled with blood in which no fetus may be detected. Such cases have been repeatedly described as hematosalpinx, the real origin of the condition in pregnancy not being known. The fetus had been absorbed or broken up and scattered through the blood-mass. Careful microscopic examination of the tube reveals the true condition—a destroyed tubal pregnancy with hemorrhage into the tube. As has already been said, hematosalpinx not caused by tubal pregnancy is very rare.
Coincidently with the development of the tubal pregnancy there occur enlargement of the body of the uterus and decidual transformation of the endometrium. The decidual membrane separates, entire or in fragments, and is discharged from the uterus, after the death of the embryo or during its development, from the eighth to the tenth week. The decidua again forms only when gestation continues undisturbed.
The enlargement of the uterus varies a great deal according to the position of the tubal pregnancy and the course of its development. The interstitial variety is accompanied by the greatest uterine enlargement. When 321 the tubal gestation has reached full time the uterus may measure from 4 to 7½ inches in length.
The increased size of the uterus is most marked in the long diameter. The change of shape does not resemble that which occurs in normal pregnancy.
The uterus also becomes softer in tubal pregnancy, and the cervix softens somewhat, though not so much as in a uterine pregnancy.
If the woman and the fetus survive the many dangers that accompany the progress of tubal gestation, the development of the fetus will go on to full term, and then the phenomenon of spurious labor will come on.
In spurious labor there are a series of periodical pains that resemble those of normal labor. The pains may last from a few hours to several days. They may cease, and reappear after varying intervals.
Hemorrhage usually takes place from the uterus. After the spurious labor the uterine discharge may be of the same character as that seen after normal labor.
It is probable that the fetus always dies after spurious labor. The liquor amnii is absorbed, the gestation-sac shrinks, and changes take place in the fetus similar to those already referred to. It may become mummified or converted into adipocere or a lithopedion. In this condition it may remain in the abdomen for many years. A mummified fetus that had been carried for fifty years has been removed post-mortem from a woman aged eighty-two.
Rarely, after spurious labor the gestation-sac ruptures and the fetus is discharged into the peritoneum, the vagina, or the large intestine, whence it is born through the anus.
The symptoms of tubal pregnancy are in some cases similar in all respects to those of normal uterine pregnancy. In extremely rare cases the woman has reached full term in ignorance of any unusual condition. Usually, however, the early occurrence of some of the accidents of tubal gestation attracts her attention. Before such 322 accidents or complications arise there are most frequently no subjective symptoms to excite any suspicion of the peculiar form of pregnancy. Changes in the skin, in the nipples, in the nervous and circulatory systems, and in the gastro-intestinal tract may resemble those of normal pregnancy, and are subject to the same variations.
Mammary changes accompanied by the secretion of milk occur in tubal pregnancy. These changes are, however, less pronounced than in uterine gestation. The vagina may undergo changes similar to those of normal pregnancy; it becomes soft, relaxed, and altered in color, and pulsation of vessels may be felt in the walls.
It should always be remembered, however, that tubal pregnancy may occur without the presence of any of the signs of pregnancy. Women in perfect health, thoughtless of pregnancy, have died of acute hemorrhage from a ruptured tubal gestation—the first symptom of this condition.
The changes in menstruation vary a great deal. Menstruation usually ceases when tubal pregnancy begins, though not with the same regularity as in normal pregnancy.
Sometimes menstruation continues for a few months and then ceases. In other cases menstruation is arrested for the first few months, and occurs with greater or less regularity during the latter months of pregnancy. There may be an irregular discharge of blood throughout the whole course of gestation.
In the blood discharged from the uterus there may often be found pieces of decidual tissue of various size. Sometimes the whole decidual membrane of the uterus may be expelled in one mass. In any suspected case the blood should always be carefully examined for such decidual membrane. All shreds of tissue should be submitted to careful microscopic examination. The woman should be questioned in regard to the passage of such tissue before she came under medical supervision.
The woman often complains of periodical pains occurring 323 in the hypogastrium and in the pregnant tube. They usually appear after the second month, though they may begin earlier. These pains are thought to be caused by the contractions of the uterus and the gestation-sac.
The abdominal enlargement in extra-uterine pregnancy differs in several respects from that of normal pregnancy. It is usually most marked on one side of the abdomen, especially during the first five or six months.
Toward the end of gestation the enlargement becomes more symmetrical in the abdomen, and resembles closely that of normal pregnancy.
In tubal gestation, on account of the higher position of the tube, bulging of the abdominal wall is likely to appear somewhat earlier than in normal pregnancy. The abdominal enlargement in tubal pregnancy does not follow the same uniform progress that is characteristic of uterine pregnancy.
Fetal movements take place, and fetal heart-sounds are heard as in normal pregnancy.
Bimanual examination made before rupture of the tube will reveal the tubal enlargement, the shape of the tube depending, of course, upon the position of the tubal pregnancy. The tubal enlargement is said by Veit to have a characteristic soft feel, distinct from the hard or fluctuating enlargements of other forms of tubal disease.
After rupture the distinct tubal tumor disappears, and the examiner feels a mass lying to one side of or behind the uterus. The enlarged tube may be felt merged in this mass.
If pregnancy continues after rupture, the fetal movements may be felt and ballottement may be obtained. The cervix is found to be somewhat softened; the os may be patulous; the uterus is soft and enlarged. The uterine enlargement, however, is not of the same rounded shape as the pregnant uterus, and the size is much less than that of corresponding periods of normal pregnancy.
It is of great importance to study the symptoms of the accidents of tubal pregnancy. As has already been said, 324 it is usually the accident of rupture that first directs the woman’s attention to the abnormal condition.
The symptoms depend upon the seat of rupture. Rupture of the tube into the broad ligament is a much less serious accident than rupture into the peritoneal cavity.
If the rupture into the broad ligament is sudden, the woman complains of sudden acute pain in the affected side. The pain may extend to the back and throughout the pelvis. The intensity and extent of the pain depend on the amount of blood that escapes. Sometimes only a small hematoma is found in the broad ligament; at other times the blood burrows around the rectum, and symptoms of pressure may arise. Difficult defecation may follow. Retention of urine may occur.
The woman suffers from shock, and may become somewhat anemic.
Bimanual examination reveals the condition. The broad ligament will be found filled with a tense mass that bulges into the vagina. The uterus is pushed to one side. The mass may extend behind the uterus and surround the rectum. The upper outlines felt by the abdominal hand are ill defined.
The loss of blood from simple rupture into the broad ligament is not often sufficient to cause death. The fetus may continue to develop, however, and secondary rupture into the peritoneal cavity may occur.
Rupture of the tube or of the gestation-sac into the peritoneal cavity is a very fatal occurrence. In the majority of cases death from hemorrhage occurs within twenty-four hours.
Unless the ovum plugs the rent in the tube, there is nothing to arrest the hemorrhage.
The woman is seized with sudden pain in the side, often described as the sensation of “something giving away.” She suffers from faintness, acute anemia, nausea, vomiting, and collapse. As in other cases of acute anemia, there may be delirium and convulsions.
Bimanual examination made after intraperitoneal rupture 325 reveals an indefinite fulness or a yielding mass in the pelvis behind the uterus. The blood free in the peritoneal cavity coagulates slowly, and the fluid blood or soft unrestrained clots are often very difficult to palpate. For this reason, at first the examiner can feel only an ill-defined fulness in the pelvis. If the woman survives and the mass of blood becomes more solid, it may then be distinctly palpated as a solid mass behind the uterus, bulging into the vagina, and extending up into the abdomen. Though the hematocele may at first be difficult to define, yet the enlarged tube may usually be palpated, and the ovum may sometimes be felt in the midst of the ill-defined mass of blood.
As has already been said, in rare cases rupture may occur intraperitoneally or into the broad ligament without producing any of the severe symptoms just described. The fetus continues to develop, and the woman will be ignorant that rupture has ever occurred. Between the two extremes there are all degrees of severity.
In tubal abortion the symptoms resemble those of intraperitoneal rupture.
If the fetus dies within the tube, the symptoms become those of hematosalpinx or other form of tubal disease.
Diagnosis.—The diagnosis of tubal pregnancy is not often made before rupture, because there are usually no symptoms that direct the woman’s attention to the abnormality of her condition. Very often she thinks that she is normally pregnant.
If opportunity is given for examination before rupture, the diagnosis may sometimes be made. The woman presents the signs of pregnancy. The uterus may be slightly enlarged, though not of the size or shape normal for the stage of pregnancy. There is a soft tubal tumor.
Immediately after rupture the diagnosis of the condition must be made from a study of the previous history, 326 from the present subjective symptoms, and by bimanual examination.
If a woman who had thought herself pregnant is suddenly seized with pain in the side, followed by anemia and shock, the suspicion of extra-uterine pregnancy should be aroused. If bimanual examination reveals the hematoma or hematocele in the pelvis, with tubal enlargement, the diagnosis may be made. Pelvic hematoma and hematocele are in nearly all cases caused by tubal pregnancy.
If the woman survives the rupture and the fetus continues to develop, the diagnosis becomes easier the more advanced is the case.
It must be remembered that amenorrhea is not as general in tubal as in uterine pregnancy. The woman often gives the history of irregular bleeding, or of arrest for a few periods and then recurrence of menstruation. Such experience may lead her to seek medical advice even before rupture.
The intermitting attacks of pain that are sometimes felt in the affected tube may also cause her to seek medical advice.
A history of the discharge of membrane or of shreds of membrane is of great value. If opportunity is afforded for examination of such shreds, and decidual cells are found, and if uterine pregnancy may be excluded, there is very strong evidence that any mass in the pelvis is an extra-uterine gestation.
It has been advised to curette the uterus for diagnosis in order to determine the decidual character of the lining membrane. This is good advice if the operation is performed with great care and if we can with certainty exclude the possibility of uterine pregnancy. If followed indiscriminately, numbers of abortions would be produced. Uterine pregnancy has often been mistaken for tubal pregnancy. The mistake is likely to occur when the fundus is drawn to one side or is retroflexed. Uterine 327 pregnancy may occur with tubal enlargement from other cause than tubal pregnancy.
In conclusion, the diagnosis of tubal pregnancy before the presence of a fetus can be ascertained is based on the following considerations: The symptoms of pregnancy; a tubal or pelvic tumor; a slightly enlarged though not pregnant uterus; discharge of decidual tissue from the uterus; the history of the woman pointing to menstrual irregularity, uterine discharge of shreds, history of previous tubal rupture.
Treatment.—The treatment of tubal pregnancy is operative. It may be considered under the following heads: Before primary rupture; At the time of rupture; After rupture.
Before Primary Rupture.—If the physician is so fortunate as to recognize a tubal pregnancy before primary rupture, he should without delay remove the affected tube and the contained ovum. The operation is simple, is attended by no more danger than that accompanying an ordinary salpingo-oöphorectomy, and the woman is saved the imminent dangers associated with a developing tubal pregnancy. There are no circumstances under which it is proper to follow an expectant treatment.
Most of the cases of unruptured tubal pregnancy that have been operated upon were not recognized until the abdomen had been opened. The operation was performed under the diagnosis of pyosalpinx, hematosalpinx, or some other tubal disease. The cases show the value of the general rule to operate without delay for all gross diseases of the tubes.
At the Time of Rupture.—Many cases of tubal pregnancy are first seen at the time of rupture. In such cases celiotomy should be performed without delay. The condition is most urgent in intraperitoneal rupture, but it is the safest rule to operate immediately, whether the rupture be intraperitoneal or extraperitoneal. It is unwise to wait for reaction. The physical depression in such cases is due more to hemorrhage than to shock, and it is 328 in accord with general surgical principles to arrest hemorrhage at once.
Rupture usually takes place before the twelfth week, and the whole product of conception, with the tube, may readily be removed. Hemorrhage usually ceases as soon as the proximal and distal ends of the ovarian artery are ligated. The ligatures may be placed about the ovarian artery, at the pelvic wall, and at the uterine cornu, as the first steps of the operation, before any attempt is made to remove the mass. It may be necessary to close the rent in the broad ligament by a series of sutures.
After Rupture.—If the woman survive, and is first seen after primary rupture, one of two conditions will be present—a destroyed or a developing extra-uterine pregnancy. If the fetus has died and gestation has ceased, the woman is exposed to the various dangers that attend the presence of such a foreign body in the abdomen. If the fetus has died during the earlier months, it may have been absorbed and spontaneous cure may take place. Even a dead full-term fetus has been carried in the abdomen for years without producing a fatal result to the mother. It seems safest, however, in all such cases to operate as soon as the condition is recognized. The rules of abdominal and pelvic surgery apply to such cases. The placenta of a dead fetus may be removed without fear of uncontrollable hemorrhage.
If the woman is seen after primary rupture, with a developing gestation, the case presents much more serious dangers. These dangers lie in the placenta. If the pregnancy has not advanced beyond the fourth month, it is usually possible to remove the whole of the gestation-sac, the embryo, and the placenta without uncontrollable hemorrhage. The ovarian, and if necessary the uterine, arteries may be ligated, and the placenta may be removed in one mass. The cavity of the broad ligament may be obliterated by buried sutures.
If the gestation has advanced beyond the fourth month, it is often impossible to remove the placenta without fatal 329 hemorrhage. Many women have bled to death from the attempt. The operator sometimes incises the placenta as he enters the gestation-sac, and is obliged to proceed with its removal. In other cases he starts to remove it, and finds, too late, that the hemorrhage is beyond his control. In the advanced months of pregnancy the sac and the placenta may become adherent to any of the abdominal or pelvic viscera and to the large vessels. Hemorrhage cannot be controlled, as in the earlier months, by ligation of the ovarian and uterine arteries. The result in these cases is determined by the ability of the operator. A full-term living child, the whole sac, and the placenta have been successfully removed. If the attachments are such that the surgeon considers it unsafe to attempt the removal of the sac and the placenta, the sac should be incised and the fetus should be removed, the cord being divided between two ligatures; the sac should be sutured to the abdominal incision; the cord should be drawn through the opening, and the sac packed with gauze. At the end of four or five days the gauze pack may be removed, under anesthesia if necessary, and the placenta may be taken away. There is very much less risk of hemorrhage after the lapse of a few days. Some operators prefer to allow the placenta to come away spontaneously. This is sometimes necessary.
It will be seen, from this consideration, that the treatment of all varieties of ectopic gestation is operative, and that the sooner the operation is performed the better for the patient. Consideration for the life of the child should have no influence in determining the time of operation.
Ovarian Pregnancy.—The possibility of the implantation and development of the fertilized ovum in the Graafian follicle has been denied by many authorities. It seems probable, however, that such a form of pregnancy does very rarely occur. The cause of ovarian pregnancy is thought to be due to some disturbance of the normal process of ovulation, whereby the ovum fails to leave the ruptured follicle and is there fertilized and developed. 330
Anatomy.—The ovaries vary a good deal in size, within the limits of health, in different individuals. It is unusual to find the two ovaries in the same person exactly alike in size, shape, and appearance.
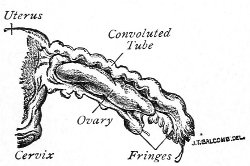
Fig. 158.—Uterus, tube, and ovary of a child one month old (Sutton).
The size, shape, and appearance of the ovary change at the different periods of life. In the new-born child the ovary is elongated and lies parallel to the Fallopian tube (Fig. 158). In rare cases this infantile shape of the ovary may persist throughout life.
The general shape of the mature ovary is oval. The average measurements are—long axis, 3 to 5 centimeters; breadth, 2 to 3 centimeters; thickness, 12 millimeters; weight, 100 grains. These measurements are subject to great variations. Henning’s table of measurements shows that the ovary of the multipara is no larger than that of the virgin.
After the menopause the ovaries shrink a great deal in size, sharing in the general atrophy of all the reproductive organs. The ovary of an old woman may weigh but 15 grains.
The healthy ovary is of a pinkish pearly color. On its surface are seen small bluish areas that mark the position of unruptured or of recently ruptured ovarian follicles. The ripening follicles project somewhat from the surface of the ovary, and the old ruptured follicles are marked by 331 scars which in time cover and render irregular the whole surface of the ovary (Fig. 159).
The surface of the ovary becomes more irregular and wrinkled after the menopause. The follicles disappear, until finally nothing is left but a mass of fibrous tissue and a few blood-vessels.
The ovary lies in the posterior layer of the broad ligament. It is attached by this connection with the broad ligament and by the ovarian and infundibulo-pelvic ligaments.
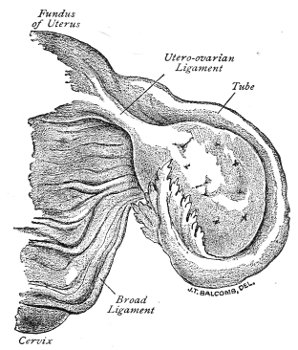
Fig. 159.—Ovary (natural size), with the Fallopian tube in relative position (Sutton).
The ovarian ligament extends from the inner end of the ovary to the angle of the uterus immediately below the origin of the Fallopian tube. This ligament varies in length from 3 to 5 centimeters. It is shortest in the virgin, and longest in the multiparous woman. The ligament consists of a fold of peritoneum containing unstriped muscular fiber from the uterus.
The infundibulo-pelvic ligament is that part of the 332 upper margin of the broad ligament lying between the distal end of the Fallopian tube and the pelvic wall. It is about 2 centimeters in length. The length is greatest in the multiparous woman.
The position of the ovary is maintained by its attachments and by its own specific gravity. The considerations that have been discussed in regard to the position of the uterus also apply here.
The blood-vessels are the utero-ovarian arteries and the ovarian arteries and veins. The ovarian artery is homologous to the spermatic artery in the male. The course of the ovarian veins has an important influence upon some pathological conditions of the ovaries.
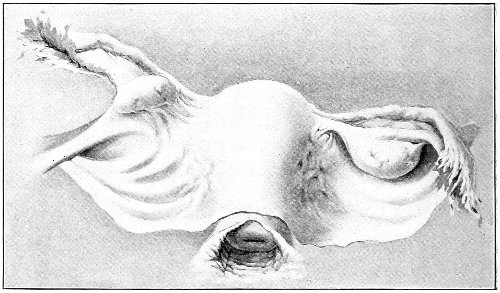
Fig. 160.—View of the posterior surface of the uterus, Fallopian tubes, ovaries, and broad ligaments. The infundibulo-pelvic ligament is shown on the left (Dickinson).
The right ovarian vein enters the inferior vena cava at an acute angle, and at the junction of the two there is a very perfect valve.
The left ovarian vein enters the left renal vein at a right angle: there is no valve on this side. This anatomical difference affords a probable explanation of the greater tendency to congestion and prolapse of the left ovary. 333
The ovary is composed of connective tissue which surrounds the Graafian follicles, blood-vessels, lymphatics, nerves, and unstriped muscular fibers. The posterior portion, or the free portion of the ovary, is covered with the germinal epithelium, or modified peritoneum, which is continuous with the peritoneum of the broad ligament.
The ovary is divided into two portions, which present distinct anatomical, physiological, and pathological differences.
The oöphoron is the egg-bearing portion of the ovary. It corresponds to the free border of the gland.
The paroöphoron corresponds to the hilum of the ovary—that portion in relation with the broad ligament.
The paroöphoron contains no ovarian follicles. It is composed of connective tissue and numerous blood-vessels. In the paroöphoron of young ovaries remnants of gland-tubules—vestiges of the Wolffian body—may be found.
Accessory ovaries have been described by several writers, and their existence has often been assumed to account for the persistence of menstruation after a supposed complete salpingo-oöphorectomy. It is very doubtful if a true accessory ovary has ever been found. Bland Sutton says: “As the evidence at present stands, an accessory ovary quite separate from the main gland, so as to form a distinct organ, has yet to be described by a competent observer.” It is probable that the bodies that have been described as accessory ovaries have been more or less detached portions of a lobulated ovary, or small fibro-myomatous tumors of the ovarian ligament. Abdominal surgeons have had opportunity of examining thousands of ovaries at operation, and yet I know of no one who has come across a third ovary. 334
Hernia of the ovary may take place through the inguinal ring. Congenital hernia of the ovary is extremely rare. Bland Sutton says that there is no properly authenticated case. Notwithstanding the frequency of congenital hernia in infants, the ovary has not been found in the hernial sac at birth.
In cases that have been reported as congenital hernia of the ovaries the structures have, on microscopical examination, been found to be testicles, the individual being hermaphroditic.
Acquired hernia of the ovary is of not infrequent occurrence. The ovary may occupy the hernial sac alone or along with other structures.
Ovulation may occur normally, and conception may take place. A true corpus luteum has been found in an ovary contained in a hernial sac.
The ovary may remain in the inguinal ring or may pass into the labium majus. In some cases no trouble whatever arises from this displacement. Hernia of the ovary has been found accidentally at autopsy, having been entirely overlooked during life. In other cases swelling and severe pain may be experienced at the menstrual periods.
The ovary is exposed to the dangers of congestion and inflammation. Adhesions may result, and suppuration has occurred. In such cases the symptoms of ovaritis are present.
The diagnosis of hernia of the ovary is made from palpation of the gland; from the determination, by bimanual 335 examination, of its connection with the uterus; from the characteristic sickening pain experienced upon pressure; and from the swelling and increased pain at the menstrual period.
The treatment is the same as that applied to hernia of any other structure. The hernia should be reduced if possible, and retained by a truss; or the ring may be closed by radical operation for hernia. If the ovary is adherent, operation is necessary before reduction can be accomplished. If the ovary is itself grossly diseased, its removal may be necessary.
Prolapse of the ovary is a downward displacement of this organ behind the uterus. Various degrees of prolapse occur, from a slight descent to complete prolapse in the bottom of Douglas’s pouch.
There are two general kinds of ovarian prolapse. In one the uterus is primarily the displaced organ, and when prolapsed, retroverted, or retroflexed, it drags the ovaries out of place with it. Such cases have been referred to in discussing uterine displacement. If the ovaries are not adherent, they usually return to the normal position when the uterus is replaced. Similar to this kind of displacement of the ovary is that which occurs in disease of the Fallopian tubes, which, when enlarged, descend and drag the ovaries with them. In the other variety the displacement is primary in the ovary, and occurs independently of any displacement of the uterus or other structure to which it is attached. It is such prolapse that will be considered here.
There are various causes of ovarian prolapse. In some cases it is probable that the position of the ovaries in the bottom of Douglas’s pouch is congenital.
A sudden strain or effort is said to have produced acute prolapse of the ovary.
Anything that increases the weight of the ovary may 336 cause its descent. Prolonged congestion, inflammation, or small ovarian tumors may result in ovarian prolapse.
Subinvolution is the most frequent cause of ovarian prolapse. In pregnancy the ovaries become very much enlarged, especially the left one. The ovarian ligament and the infundibulo-pelvic ligament become much increased in length. If, after labor, involution is arrested or is incomplete for any reason, the conditions favorable for prolapse of the ovary will be present—increased weight of the ovary and relaxation and lengthening of its attachments. Sometimes the cause of the prolapse is in the ligaments alone. The ovary may have returned to its normal size, while the ligaments may have remained subinvoluted, permitting undue freedom of movement.
The left ovary is more frequently prolapsed than the right. There are two reasons for this difference. As has just been said, the left ovary becomes more enlarged during pregnancy, and therefore suffers more from subinvolution, and the arrangement of the veins on the left side is such that venous congestion is very liable to occur.
When prolapse has existed for a long time, secondary changes take place in the ovary as the result of hyperemia, and the condition becomes further aggravated.
Symptoms.—Slight descent of the ovary very often causes no suffering whatever. When, however, the ovary is completely prolapsed, lying in the bottom of Douglas’s pouch, between the posterior wall of the vagina and the rectum, well-marked symptoms usually arise.
The woman suffers pain whenever she is in the erect position. The pain is increased by walking, probably because the ovary is squeezed between the cervix and the sacrum. Coitus sometimes causes intense pain. Defecation causes pain. The pain begins with the movements of the bowels, and often lasts for one or two hours afterward. It is dull and aching in character, and is situated in the normal position of the ovary, radiating thence 337 throughout the pelvis and extending down the thighs. It frequently produces faintness and nausea.
The ovarian pain is markedly increased at the menstrual periods.
The general and reflex disturbances produced by prolapse of the ovary are often very pronounced. There may be headache, indigestion, hysteria, and great mental depression. A reflex pain is often felt in the breast on the same side with the affected ovary.
Bimanual examination usually reveals the condition. The prolapsed ovary may readily be felt by the vaginal finger. If the finger is introduced high up behind the cervix, and is then turned with the palmar surface backward, the ovary may be caught between the finger and the sacrum. The irregular surface of the ovary, due to the prominent vesicles and the old scars, may often be felt. When the ovary is pressed upon there is a characteristic sickening feeling experienced by the woman. Sometimes she cries out with intense pain even upon the gentlest pressure on the ovary. After witnessing such pain the physician realizes the extent of the suffering experienced in walking, at coitus, and at defecation. If the ovary is not adherent, it may slip from the examining finger, and perhaps may not be felt again until a subsequent examination, after it has returned to its prolapsed position.
A large prolapsed ovary has often been mistaken for the fundus uteri, and has caused the diagnosis of retroflexion to be made. This mistake will not occur if the examiner determines the real position of the uterus by palpation or by the sound. The uterus may usually be moved independently of the prolapsed ovary.
Treatment.—The treatment of ovarian prolapse depends upon the cause of the condition. Prolapse of the ovary caused by uterine displacement is usually cured by the treatment that restores the uterus to its normal position.
Prolapse of the ovary accompanying tubal disease and 338 prolapse caused by small ovarian tumors demand operation and removal of the tube and ovary.
When the ovary is not adherent, it may sometimes be restored to its normal position, or at least be considerably elevated, so that the suffering is much relieved, by placing the woman in the knee-chest position and opening the vagina. In this position all the pelvic structures are carried upward.
A pledget of cotton or wool placed back of the cervix, in the posterior vaginal fornix, will often give great temporary relief. The cotton may stay in the vagina for twenty-four to forty-eight hours.
The woman should be advised to assume the knee-chest position, allowing air to enter the vagina by introducing the nozzle-piece of the vaginal syringe, once or twice daily. The best time is immediately before retiring at night, and she should afterwards sleep as much as possible on the side, in the Sims position. She should remain in the knee-chest position for several minutes—until tired.
In addition to this treatment, the pelvic congestion should be relieved by continuous use of saline laxatives, by hot-water vaginal douches, and by occasional applications of Churchill’s tincture of iodine to the vaginal vault, and the use of the glycerine tampon. If the prolapse has been caused by subinvolution of the ovary and its attachments, such treatment may ultimately result in cure. The enlarged ovary diminishes in size and weight, and its ligaments contract and regain tonicity.
Subinvolution of the uterus is often also present. This condition should be treated as has already been advised.
In many cases of ovarian prolapse there have taken place in the ovary secondary changes that resist such treatment even when most conscientiously applied. The physician is then driven to the operation of oöphorectomy as the only method of relieving the intolerable suffering. This operation should never be performed, however, until other milder treatment has been carefully tried, and unless 339 the suffering of the woman incapacitates her for the duties of life.
In some cases in which the ovary is not itself grossly diseased it may be possible to avoid oöphorectomy, and to correct the displacement by attaching the ovary by suture to the upper margin of the broad ligament, or by shortening the infundibulo-pelvic ligament by suture. If the ovary has become adherent in Douglas’s pouch, the condition can be relieved only by operation—celiotomy, and usually oöphorectomy.
A variety of pessaries have been invented for the relief of ovarian prolapse. They are of but little, if any, use. In many cases the pressure of the pessary upon the ovary renders its employment impossible. No pessary will cure a simple prolapse of the ovary. The cases in which the pessary does good are those in which there is a primary uterine displacement.
Acute Oöphoritis.—In acute oöphoritis the inflammation may begin on the surface of the ovary (perioöphoritis) and extend inward, or it may begin in the ovary itself. When the disease is caused by extension of the inflammation from the tubes, it usually begins as a perioöphoritis. Both the follicular and interstitial portions of the ovary may be affected. When the inflammation is confined chiefly to the ovarian follicles, it is said to be parenchymatous; when the connective tissue is chiefly affected, it is called interstitial oöphoritis. In acute inflammations all portions of the ovary are usually involved at one time.
The changes are those that characterize inflammation of other glandular structures. The whole organ becomes swollen, hyperemic, and edematous. The liquor folliculi becomes turbid; the membrana granulosa becomes softened and disintegrated. The surface of the ovary may be covered with an inflammatory exudate. In severe septic cases the whole ovary may become destroyed, or 340 one or more ovarian abscesses may be formed. In less severe cases the inflammation subsides before suppuration takes place, or goes on to chronic oöphoritis.
The usual cause of acute oöphoritis is extension of inflammation from the Fallopian tube.
Acute oöphoritis may also occur as the result of septic infection carried by the lymphatics of the uterus. The disease is not uncommon in puerperal sepsis. Here it often forms but a minor part of a general fatal infection.
Gonorrhea may cause oöphoritis in a similar way.
Acute suppression of menstruation is said to result in inflammation of the ovaries.
Acute rheumatism and the eruptive fevers may produce oöphoritis. The disease of the ovaries is often overlooked during the acute attack, while the attention of the physician is engaged by the general affection. These diseases, occurring in childhood, are the probable causes of some of the damaged and chronically inflamed ovaries with which women suffer in later life. To these diseases also are to be attributed many cases of arrested development of the sexual apparatus, the phenomena of which appear only after menstruation has begun. The ovarian disease in these cases may be very insidious. Decided microscopic changes have been found in the ovarian follicles in scarlet fever, though to the naked eye the gland was unchanged.
The symptoms of acute oöphoritis are very often masked by those of accompanying affections, such as salpingitis and puerperal sepsis.
There may be a chill, followed by fever, nausea, and vomiting.
The pain is that which characterizes any local pelvic inflammation. It is most intense in the ovarian regions.
Bimanual examination may reveal the enlarged, tender ovaries, which are very often prolapsed behind the uterus.
The greatest gentleness should always be observed in making a vaginal examination in any case of inflammation of the pelvic structures, not only to avoid inflicting 341 unnecessary pain, but because a much more satisfactory examination can be made if the woman does not fear and resist the examiner.
Treatment.—The treatment of acute oöphoritis is expectant. It is similar to that already advised for acute salpingitis. The physician should prescribe absolute rest in bed; hot fomentations over the abdomen; saline laxatives; and warm vaginal douches of sterile water if the pain is not increased by them.
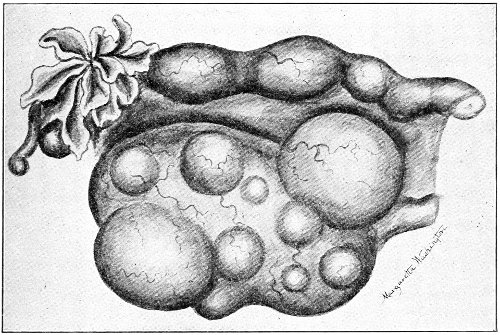
Fig. 161.—Cystic ovary.
If suppuration occurs, immediate laparotomy with removal of the diseased structures should be practised. If the acute inflammation subside, subsequent operation may be necessary for the chronic inflammation.
Chronic Oöphoritis.—Chronic oöphoritis, like the acute form, may be either parenchymatous or interstitial. Usually both the connective tissue and the ovarian follicles are involved. The disease is usually bilateral. The tunica albuginea may become much thickened, and adhesions may form between the ovary and the adjacent structures.
In practice we find chronic oöphoritis in two forms: 342 The ovary may be cystic, filled with a number of cysts of varying size up to that of a marble (Fig. 161). These cysts are transformed ovarian follicles. The walls are thickened, and the ova and the membrana granulosa have undergone fatty degeneration and absorption. The fluid in the cysts may be clear, cloudy, bloody, or gelatinous. Sometimes the septa are absorbed, and several cysts are thrown into one cavity. The connective tissue of the ovary is increased in amount.
The ovary becomes enlarged, though it rarely exceeds the size of a hen’s egg.
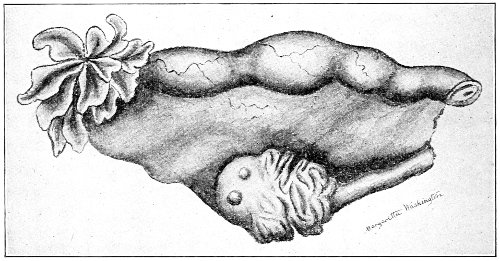
Fig. 162.—Cirrhotic ovary from an old maid forty years of age.
It is probable that this form of inflammatory change is the origin of some kinds of small ovarian cystic tumors.
In the other form of chronic oöphoritis the interstitial changes are most marked. There is a decided increase of the connective tissue, and a diminution of the parenchymatous or follicular structures. The ovary is hard and cirrhotic, and is of a lighter or paler color than normal; the visible ovarian follicles are few; the greater part of the ovary appears to be a mass of wrinkled connective tissue; in some cases the follicular structure is confined to but one-quarter of the ovary. The changes resemble and are similar to those that take place physiologically in the ovaries of old women (see Fig. 162). 343 Between these two types of cystic and cirrhotic ovaries various forms, combinations of the two, may occur. The ovary upon one side may be cystic, upon the other cirrhotic.
The causes of chronic oöphoritis are various. The condition may persist after the subsidence of acute oöphoritis. It is usually secondary to salpingitis. There are very few cases of chronic salpingitis that are not accompanied by some form of oöphoritis. The disease may be chronic from the beginning. It may develop slowly from septic or gonorrheal infection from the uterus. It may result from subinvolution or prolapse of the ovary.
It may result from immoderate sexual irritation, and from unnatural gratification of the sexual impulse.
It seems probable also that chronic ovaritis may occur as the result of celibacy or sterility. The unceasing menstrual congestions of the virgin or the sterile woman, which, as has already been pointed out, seem to predispose the woman to fibroid changes in the uterus, seem likewise to develop the growth of connective tissue in the ovary. Virgins between the ages of thirty and forty often present hard cirrhotic ovaries with decided diminution of the follicular elements. The condition is often associated with a fibroid state of the uterus, this organ being indurated from interstitial fibroid deposit, or presenting one or more subperitoneal nodules.
Symptoms.—The most prominent symptom of chronic oöphoritis is pain. The disease is usually bilateral, and the pain affects both ovarian regions; it is, however, usually more marked upon the left side. The pain is increased by the erect position and by exercise, defecation, and coitus. Pain at defecation and coitus is most marked when ovarian prolapse accompanies the inflammation.
The pain is increased at the menstrual period. It is most intense immediately before and at the beginning of the flow. If the bleeding is profuse, the pain is often relieved. 344
Menorrhagia often accompanies chronic oöphoritis, and seems to occur chiefly with the cystic variety of the disease. As most cases of oöphoritis are accompanied by endometritis and salpingitis, it is difficult to determine how important a part in the production of the menorrhagia is played by the ovarian disease. Reflex pain in the region of one or both breasts, usually the left, is often complained of.
The reflex disturbances caused by chronic oöphoritis form a very important part of the woman’s suffering. Loss of appetite, digestive disturbances, nausea, and vomiting occur. Hysteria, profound mental depression, and various cerebral derangements take place. Sterility may be caused by chronic oöphoritis if the ovarian capsule becomes so thickened that rupture of ovarian follicles cannot take place.
Bimanual examination should be performed with great gentleness. The condition of the ovary may be most satisfactorily determined in those cases in which the ovarian lesion is the chief trouble and in which the tubes and other pelvic structures are not coincidently inflamed. If the ovary is felt, it is found to be very tender and usually enlarged. In cases of long-standing interstitial inflammation the ovary may be below the usual size. Palpation is very easy if the ovary is prolapsed in Douglas’s pouch.
Chronic oöphoritis rarely recovers spontaneously. The woman may have periods of relief, but the symptoms may all recur after some indiscretion or unusual exercise. Suffering usually diminishes, and may in time cease, after the menopause, when atrophy takes place and menstrual congestions have stopped.
Treatment.—Chronic oöphoritis usually requires operative treatment (salpingo-oöphorectomy), because it is associated with disease of the tubes. In other cases a great deal may be accomplished without operation, and the woman may be tided over the period of menstrual life until permanent relief is secured at the menopause. 345
This palliative treatment is usually applicable, however, only to those women who are not dependent for a living upon their own labor. It is best to begin the treatment by putting the woman to bed for one or two months; to administer daily massage; to maintain mild purgation with saline purgatives; to make, once a week, applications of Churchill’s tincture of iodine to the vaginal vault, followed by the glycerin tampon; and to give hot-water vaginal injections twice a day.
If there is any disease of the uterus, such as laceration of the cervix or endometritis, this should be treated first.
After the woman leaves her bed the douches, saline laxatives, and vaginal applications should be continued. Absolute rest in the recumbent posture should be prescribed at the menstrual periods, and at other times if the ovarian pain becomes severe. Coitus should be forbidden during the treatment. If the woman is unable to begin the treatment by prolonged rest, the subsequent part of the treatment advised here may be followed.
This treatment always does good for a time. Unfortunately, its results are not often permanent. The old pain and suffering return as soon as the woman ceases to be under medical care. If the inflammatory changes have become well established, no permanent good results from any medical treatment. This is especially true in those cases in which the original causative state of things continues after treatment is given up. If the cirrhotic ovaries are the result of celibacy, medicine can be but palliative.
Working-women are unable to obtain the proper medical treatment, especially when the prospect of cure is doubtful, and therefore, if their suffering incapacitates them, must be subjected to the operation of oöphorectomy.
In any case oöphorectomy should be advised if the suffering persists after carefully tried medical treatment. 346
Hemorrhage may take place either into an ovarian follicle, in which case it is called follicular hemorrhage; or it may take place into the ovarian stroma; to this condition the term ovarian apoplexy is applied.
Hemorrhage into the follicles is usually small in amount, the distended follicle rarely exceeding the size of a hickory-nut. In case of cystic degeneration of the ovary small blood-filled cysts may be present, formed by the fusion of several follicular cysts. Occasionally the amount of blood in the follicle is enough to cause its rupture. If the follicle should rupture into the peritoneum, a small hematocele would result. If the follicle ruptures into the ovarian stroma, ovarian apoplexy occurs.
Follicular hemorrhage and ovarian apoplexy are most liable to occur during the congestion of a menstrual period.
Such hemorrhages are not infrequent in the acute fevers and in scurvy. The symptoms of the condition are in no way characteristic. If the exact state of the ovary were known from previous examination, follicular hemorrhage or apoplexy might be suspected from the detection of a sudden ovarian enlargement and pain unaccompanied by symptoms of inflammation.
The blood is usually absorbed, and unless some accompanying disease of the ovary is present, spontaneous recovery will result.
Ovarian hydrocele is a rare disease, the true nature of which has been explained by Bland Sutton. Most of the cases that have been reported have been mistaken for tubo-ovarian cysts. The tubo-ovarian cyst has already been described. It is a cyst that results from inflammatory disease of the tube, and is formed by the union of the cavities of a closed Fallopian tube and a follicular cyst in the ovary. 347
Ovarian hydrocele has a different origin. To understand it a brief reference to the relation between the ovary and the broad ligament is necessary. I quote from Bland Sutton: “The ovary projects from, and is invested by the posterior layer of the broad ligament. When the parts are examined in situ, the ovary will be found to lie in or upon the edge of a shallow recess in the mesosalpinx. This recess is the ovarian sac (Fig. 163). It varies in depth; in many it is small and inconspicuous, whilst in others it is sufficiently deep to accommodate the entire ovary. In the virgin the ampulla of the tube falls over the mouth of this recess and conceals the ovary. This relation of parts is usually disturbed in the first pregnancy.”
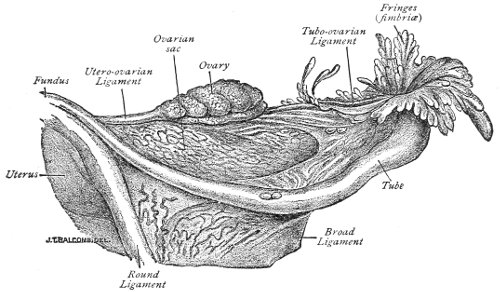
Fig. 163.—Left Fallopian tube from an adult (after Richard).
Tait1 says: “In a few exceptions I have seen a crescentic double fold of the posterior layer of the broad ligament pass down behind the ovary, covering it like the hood of a ‘Nepenthes’ gland. In all such cases the women have been sterile, probably because this hood has prevented the application to the ovary of the opening of 348 the oviduct. I have seen this arrangement give great trouble in the removal of small ovaries.” In some animals the ovarian sac is much better developed than in the human female. In the hyena it forms a complete tunic to the ovary, the cavity of the sac communicating with the peritoneum by a small opening. In rats and mice the sac is complete, and the Fallopian tube communicates with the ovarian sac, but not with the general peritoneal cavity.
Ovarian hydrocele occurs in women when the abdominal ostium of the Fallopian tube opens into a well-formed ovarian sac and the common cavity becomes distended with fluid.
Sutton sums up the peculiarities of ovarian hydrocele as follows:
I. The Fallopian tube opens by its abdominal ostium into a sac on the posterior aspect of the broad ligament.
II. The tube is elongated, dilated, and tortuous, resembling a retort with a convoluted delivery tube.
III. As a rule, there is no evidence of inflammation. The cyst may suppurate should the tube become affected with salpingitis.
IV. In small cysts the ovary will be found projecting on the floor of the sac. In larger specimens it will be incorporated with the wall of the sac, and in very large specimens it is unrecognizable.
An ovarian hydrocele may attain considerable size. A case has been reported in which three pints of straw-colored fluid were found in the cyst. An ovarian hydrocele is sometimes intermitting, discharging its contents through the tube into the uterus.
The symptoms of ovarian hydrocele resemble those of a small ovarian cyst or a tubo-ovarian cyst.
The treatment is celiotomy and removal of the tube and ovary, or, when practicable, the liberation of the adherent end of the Fallopian tube. 349
The histogenesis of cystic tumors of the ovary is not yet definitely settled. Every structure that enters into the composition of the ovary has been supposed to form the starting-point of these tumors. There are many classifications of ovarian cysts based upon the clinical, structural, or genetic features. The classification given here seems to me to be the best we have at present for the practical physician.
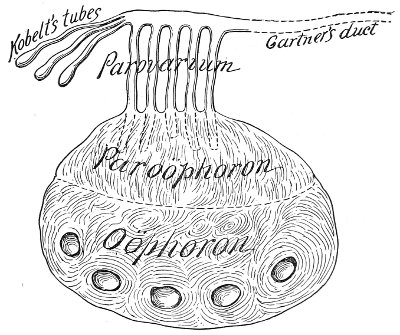
Fig. 164.—Diagram representing the cyst-regions of the ovary and broad ligament.
Cystic tumors of the ovary may be divided into two general classes:
I. Oöphoritic cysts, which originate from the oöphoron, or the egg-bearing portion of the ovary.
II. Paroöphoritic cysts, which originate in the paroöphoron. 350
Cysts of the oöphoron may be subdivided into (a) Follicular cysts; (b) Glandular cysts; (c) Dermoid cysts.
Follicular Cysts.—Follicular cysts originate in the ovarian follicles. If anything occurs to prevent the physiological rupture of a mature ovarian follicle, a follicular cyst may be started. Such cysts begin as retention-cysts of the ovarian follicles.
The condition is usually the result of chronic inflammation. The formation of new connective tissue in the ovarian stroma, the thickening of the tunica albuginea, the presence of inflammatory exudate upon the surface of the ovary, may all prevent the rupture of the follicles. In addition, the inflammatory congestion of the walls of the follicle produces an increased exudation into the ovisac.
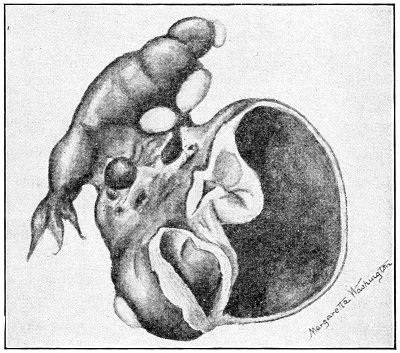
Fig. 165.—Follicular cyst of the ovary.
It seems probable that such inflammatory action may also produce cystic distention in the immature follicles that are situated remote from the surface of the ovary.
Follicular cysts may occur at any age, though they are most common during the period of sexual activity. The 351 follicular cysts may occur in one or in both ovaries; usually both ovaries are affected.
Only one follicle may be involved, or a large number of follicles, in different degrees of cystic distention, may be found scattered throughout the ovary.
Frequently one follicle enlarged to the size of a hen’s egg is observed projecting from the surface of the ovary. Sometimes the intervening septa atrophy, and one large cavity is formed by the union of two or more cystic follicles.
Follicular cysts of the ovary do not increase indefinitely with age. They are limited in growth, and in this respect differ essentially from the glandular oöphoritic cysts. They are usually about the size of a hen’s egg. They rarely attain a size greater than that of the adult fist. Exceptional cases have been reported in which the ovarian tumor was the size of the adult head. The tumor may be composed of one chief cyst-cavity, while the rest of the ovary may present a much less marked degree of cystic distention; or a large number of follicles may be uniformly distended each to the size of a cherry, forming an ovarian tumor as large as a child’s head.
When the ovarian follicle becomes distended the walls usually increase in thickness and strength.
The interior of the cyst is smooth. The character of the lining membrane varies with the size of the cavity. In small cysts it is the membrana granulosa—columnar epithelium. In cysts of medium size the cavity is lined with stratified epithelium. In the largest cavities there may be no epithelium present, the lining membrane being fibrous tissue.
The follicular cyst is usually filled with clear serum having a specific gravity of 1005 to 1020. It resembles normal liquor folliculi. The fluid may be purulent as a result of septic infection, or it may be brown or black from the presence of altered blood. Ova are sometimes found in follicular cysts of moderate size. Sometimes hemorrhage takes place into the follicular cyst, forming 352 a follicular blood-cyst, which may attain the size of a man’s fist.
Cyst of the Corpus Luteum.—A variety of the follicular cyst is the cyst of the corpus luteum. Such a cyst is formed by the degeneration and cystic distention of a corpus luteum. These cysts are usually of small size, rarely exceeding that of a walnut. The walls are thick and of a characteristic light-yellow color. The cavity is lined by a delicate membrane. Cysts of the corpus luteum are rare in the human female, but are very common in some of the lower animals—the cow and the mare.

Fig. 166.—Cyst of the corpus luteum, showing the yellow lining membrane (a); b, small follicular cyst.
The symptoms caused by follicular cysts are those of pressure and ovarian pain. The cyst may become impacted and adherent in the pelvis, and may cause pressure. The ovarian pain is analogous to that described under Chronic Oöphoritis. The pain that accompanies this form of cystic tumor of the ovary is much more marked than in the case of the larger kinds of ovarian cyst, which may be unattended by any ovarian pain whatever. In some cases follicular cystic disease of the ovaries is accompanied by menorrhagia or metrorrhagia which is only relieved by oöphorectomy. This symptom, however, is not usual.
The diagnosis of the condition is made by bimanual 353 examination and by observation of the clinical course of the disease. The cystic disease is very often bilateral. The ovarian enlargement is slow in development and is always limited. A moderate maximum size is reached and may persist for years.
Treatment.—The only curative treatment of follicular cystic disease of the ovaries is by operation and removal of the tumor. Operation is required only in those cases in which the suffering is great. The mere presence of the cystic ovary does not demand operation, whether it causes physical suffering or not, as in the case of the cystic tumors hereafter to be considered. It must be remembered, however, that it is often difficult or impossible to make a differential diagnosis between follicular cyst of the ovary and a young glandular or papillomatous cyst, and it is very much safer in all doubtful cases to adopt the operative rather than the expectant plan of treatment. If, after the abdomen is opened, the cyst is found to be follicular, the ovary need not necessarily be removed.
If, at the time of operation, the ovary is found to present but one follicular cystic cavity, this may be opened and evacuated and part of the wall may be excised. If bleeding occurs from the edges of the cyst-wall, it may be controlled by whipping with a fine continuous suture of silk or catgut. Some operators avoid this bleeding by opening the cyst with the cautery-knife. In any case the bleeding is usually slight if a thin portion of the cyst-wall is selected for the incision. If the ovary is filled with a number of cystic cavities, it is safest to remove the whole organ. If the woman be young and anxious for children, the portion of the ovary that contains the cysts may be excised and the wound in the ovary closed by sutures of fine catgut. Simple puncture of the cysts does no good. The conservative operation is especially desirable in case both ovaries are diseased. When but one is affected, the surgeon need not hesitate so much before performing oöphorectomy.
If, as is very often the case in cystic disease of this character, the Fallopian tubes are found closed by inflammatory 354 adhesions, salpingo-oöphorectomy is usually indicated.
Glandular Cysts.—Glandular cysts are also called multilocular ovarian cysts or ovarian adenomata.
It was formerly thought that all ovarian cysts originated in the Graafian follicles. This view has now been given up by most pathologists. The follicular cysts that have just been described never attain a large size, and run a distinctly different course from the glandular cysts now under consideration.
The glandular cysts probably originate from the tubes of Pflüger. It will be remembered that in the embryo the ovary contains many epithelial tubules derived from the germinal epithelium that covers the surface of the ovary. These are the tubes of Pflüger. In the process of development they become converted into Graafian follicles. Abnormally they persist, and have been found in the ovary at an advanced age, as late as the seventy-fifth year. In the newborn infant these tubes have been found cystic—the size of a pea. Such cystic degeneration of persistent tubes of Pflüger is the probable origin of glandular cysts of the ovary. According to this view, all such cysts are due to a congenital defect. Some are perhaps formed congenitally, and remain stationary or develop in later life.
The central cells of the tubes of Pflüger soften and become liquefied, and the tube becomes distended into a small pouch lined with primitive glandular epithelium.
The outer surface of a typical glandular cyst of the ovary presents a smooth, glistening, silvery appearance. This appearance is subject to considerable variation according to the character of the cyst-contents, the thickness of the wall, and the inflammatory and necrotic changes that have taken place. Sometimes there are ocher-colored or brownish spots upon the surface.
The surface of the cyst is often lobulated, from the presence of smaller cysts or a collection of secondary cysts in the wall. 355
The wall of the cyst is composed of fibrous tissue containing elastic and unstriped muscular fibers. Traces of normal ovarian tissue may be discovered in the cyst-wall. Sometimes a corpus luteum is found in the wall of a cyst of large size, showing that ovarian follicles may ripen and rupture, and that conception may take place even though the ovary is grossly diseased.
The thickest portion of the cyst-wall is that in the region of the pedicle. The thinnest portion is usually opposite the peduncular attachment.
By careful dissection the wall may generally be divided into three layers—an external and an internal layer of fibrous structure, and a middle layer of loose connective tissue. This differentiation is best marked in the region of the pedicle. In the thinnest part of the cyst the coats become blended into a thin, homogeneous, fibrous structure.
The outer surface of the cyst is covered with a layer of endothelial cells. This is not a peritoneal investment. It is intimately connected with the outer fibrous coat of the cyst, and cannot be stripped off. In this respect these cysts differ from some hereafter to be described, in which there is a distinct detachable peritoneal covering.
The blood-vessels of the tumor are distinguished throughout the fibrous wall. When three lamellæ are present, the large arteries are found in the middle layer. Lymphatics, often of large size, are also found in the cyst-wall.
The glandular cyst is always, at first, multilocular; the tumor is made up of several cyst-cavities. As the tumor increases in size the pressure causes atrophy of intervening septa, so that two or more cavities are thrown into one, and the number of loculi becomes correspondingly diminished. As the cyst grows, therefore, the tendency is toward the unilocular form. Careful examination of a unilocular glandular cyst will usually reveal the remains of atrophied septa upon the walls.
The epithelial lining of these cysts is usually composed 356 of columnar cells. In cavities of large size the cells are flattened by pressure, and in cavities of the largest size fatty degeneration and atrophy may have taken place, so that the lining cells entirely disappear.
The cavities are often lined with a soft, velvety membrane, microscopically similar to mucous membrane. The columnar epithelium dips below the surface to form complex mucous glands. These glands may become obstructed, and secondary mucous retention-cysts are formed in the walls of the parent cyst. Such a mass of secondary cysts is often seen projecting into the main cyst-cavity or forming a lobulated prominence upon its outer surface.
Follicular cystic degeneration, such as has already been described, may occur in the ovarian tissue of the wall of the glandular cyst, so that a secondary group of small cystic cavities may be formed.
It is thus seen that the structure of an oöphoritic glandular cyst may be very complex. There may be one or more chief cyst-cavities, on the walls of which may be discovered the remains of septa which had formerly subdivided them. Projecting into the cavities may be seen honeycomb-like masses of secondary mucous retention-cysts; while in the walls of the tumor, perhaps rendering the surface lobulated, may be seen minor cyst-cavities formed by beginning glandular cystic degeneration or by simple cystic degeneration of ovarian follicles (Fig. 167).
The contents of a glandular cyst vary greatly, not only in different cysts, but in the different cavities of the same cyst. Pseudomucin, a peculiar mucoid substance excreted from the lining gland cells, is a most important constituent of the contents of this cyst, and is almost characteristic.
The fluid may be thin and colorless; it may resemble thick, tenacious mucus; it may be oily or syrupy in consistency; or it may resemble transparent jelly. It may be colorless, yellow, apple-green, or brown or black from the presence of decomposed blood. As a rule, the fluid 357 becomes thinner as the cyst increases in size and age. The change is probably due to the alteration that takes place in the character of the lining membrane under the influence of continuously increasing pressure.
The specific gravity of the fluid varies from 1010 to 1050.
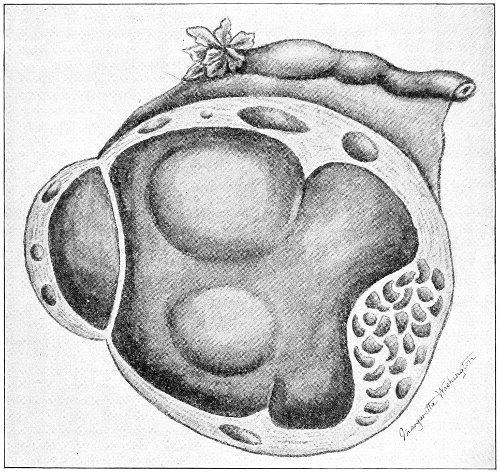
Fig. 167.—An oöphoritic glandular cyst. The section shows the remains of an atrophied septum, a number of follicular cysts in the wall, and to the right a group of mucous retention-cysts.
As glandular cysts of the ovary originate in the free border of the gland, they are in the great majority of cases intra-peritoneal in their growth. They grow into the peritoneal or the abdominal cavity; they do not push aside layers of peritoneum, like the cysts that originate between the folds of the broad ligament, and which are extra-peritoneal in their development. 358
Very rarely glandular cysts of the ovary have been found that grew between the layers of the broad ligament and were extra-peritoneal in development. It may be that in such cases the ovary itself had occupied an abnormal position.
The shape of the ovary is very early destroyed by a glandular cyst. The ovarian tissue is incorporated with, and is spread throughout the cyst-wall. In small tumors the remains of the hilum may be found at the pedicle. In no case is the body of the ovary discoverable as a distinct structure lying upon the surface of the cyst.
The pedicle of the cyst is composed of the ovarian ligament, the upper portion of the broad ligament, and the Fallopian tube. These structures are all more or less thickened and lengthened as a result of the traction and of the altered nutrition produced by the growing cyst.
The vessels of the pedicle that are derived from the ovarian and uterine arteries are of various size. The arteries rarely exceed the size of the radial artery.
Glandular cysts are of unlimited growth. They increase in size until they destroy the woman by direct pressure. They literally crowd her out of existence.
The size they may attain is determined only by the powers of resistance of the woman and the distensibility of the abdominal walls. Glandular cysts have been removed that weighed 200 pounds.
The shape of the glandular cyst is approximately spherical. It is often distorted by pressure, and portions of the tumor may represent a mould of parts of the pelvic or posterior abdominal walls.
The glandular cyst is usually unilateral. The proportion of cases in which both ovaries are affected seems to be about 4 per cent.
In some cases, when both ovaries are affected, the cysts may become fused, so that a single tumor is formed, attached by two distinct pedicles. Operation in such cases is often very embarrassing.
The glandular cyst is the most common form of ovarian 359 tumor. It may occur at any time of life from childhood to old age. It is most common between the ages of twenty and fifty.
Dermoid Cysts.—A dermoid cyst of the ovary is characterized by the presence of skin and cutaneous appendages. Dermoid cysts are found in various parts of the body, but they occur most frequently in the ovary. Of 188 dermoid cysts reported by Lebert, 129 occurred in the ovary.
Dermoid cysts comprise from 4 to 5 per cent. of all ovarian tumors.
Simple ovarian dermoids are usually of small or moderate size, varying from the size of a hen’s egg to that of the adult head. The cysts rarely contain more than 8 pints of fluid.
Dermoid cysts may become larger by fusion with glandular cysts or as the result of inflammation. Dermoid cysts are usually unilateral; both ovaries are affected in about 20 per cent. of the cases. They are primarily unilocular. Sometimes two or more dermoid cysts spring from the same ovary, and these contemporaneous cysts may become united, and the contiguous walls may atrophy so that the cavities communicate.
Dermoid cysts of the ovary have been found at all ages—in the fetus of eight months and in women over eighty years of age. They are observed most frequently from the fifteenth to the forty-fifth year.
The external appearance of the dermoid cyst differs from that of the glandular cyst. It is dull and often yellowish or brownish in color.
Upon the internal surface of the cyst is found a membrane which looks like skin and which has a similar structure. The skin may cover the whole of the surface of the cavity, or it may be restricted to a small area, and with the underlying tissue form a prominence of the cyst wall—the so-called parenchyma body. This body is composed of tissue derivatives of one, two, or all three layers 360 of the blastoderm from the surface inward—the ectoderm, mesoderm, and entoderm.
The following cutaneous appendages are found: hair, sebaceous glands, sweat-glands, teeth, mammæ, horn, nails. The cyst may also contain bone, unstriped muscle, and tissue resembling brain-matter.
The hair may arise from the whole surface of the cyst, or tufts of various length may be found growing from slight prominences of the surface. The hair is usually short; it is sometimes found, however, varying in length from 4 or 5 inches to 5 feet.
There seems to be no relation between the color of the hair of the dermoid and that upon the external surface of the body of the individual. The hair in an ovarian dermoid of a negress has been found of a blonde color.
The hair changes in color with age, and in an old woman may become white.
The hair is constantly shed, and the cyst may contain a large quantity of short loose hair mixed with the other contents. Sometimes the shed hair is found rolled up in balls of sebaceous matter.
Sebaceous glands and sweat-glands are usually numerous.
Teeth may be found free in the cyst-cavity, or they may be attached to bone or cartilage within the cyst-wall, while the crowns project into the cavity; or they may lie completely imbedded in the wall. They are often well formed, though they may be faulty in development and shape. They are usually few in number, ranging from one to ten. Many more teeth than this, however, are sometimes found; in one case there were 300.
Mammæ are found in various degrees of development. In some cases there are present one or more tags of skin resembling a nipple. In others the mammæ may be well formed and may contain glandular tissue.
The bones appear as delicate laminæ or spiculæ in the cyst-wall. They often present a striking resemblance to the flat bones of the skull and the jaw-bones. 361
The contents of a dermoid cyst vary in consistency. All the substances discharged from the lining membrane enter into their composition. They may consist of a thick oily fluid of a yellowish or brown color, or a pultaceous, semi-solid mass. They resemble the contents of a wen or a sebaceous cyst. They are usually filled with loose hairs and exfoliated epithelium. Though the fatty contents may be in a fluid condition during life, yet they solidify when exposed to the air and after death.
In some cases a dermoid cyst has been found in one ovary while a glandular cyst was in the other. Again, a single ovary may be the seat of a mixed tumor composed of dermoid and glandular cysts. In most of such cases the dermoid forms a single loculus of the tumor. Sometimes the septum between the dermoid cavity and the glandular cystic cavity atrophies and the two cavities are thrown into one. Such an occurrence explains those cases in which the cavity of a multilocular cyst is found to be partly lined with skin which is continuous with the cylindrical epithelium characteristic of the glandular cyst.
The sebaceous glands and the sweat-glands in the walls of an ovarian dermoid may become obstructed and undergo cystic degeneration, forming in this way groups of secondary cysts.
Dermoid cysts of the ovary are usually intra-peritoneal in their growth, like the glandular cysts. In some cases, however, they develop between the layers of the broad ligament, and may assume any of the positions characteristic of such extra-peritoneal growths.
Teratoma, a very rare form of ovarian tumor, is an atypical modification of the dermoid, the teratoma bearing a relation to the dermoid similar to that of carcinoma to adenoma. While in the dermoid the chief mass of the tumor has a cystic character, the cystic cavity containing the secretions from the lining epidermal tissue, the teratoma is for the most part a solid tumor, and the productive activity of the tissue is a cellular hyperplasia. 362
They appear as pedunculated nodular tumors, with a smooth surface, usually reaching a large or enormous size. The substance of the tumor is composed of the dermoid tissue spoken of, formed into irregular masses of various size, form, color, and consistency, separated by connective-tissue fasciculæ and infiltrated with small and minute cysts (dilated glands or degenerated areas). The tumor is characterized by an atypical arrangement, form, and structure of the epithelium (after the type of a carcinoma) and an excessive growth of embryonal connective tissue (after the type of a sarcoma). It is extremely malignant, being destructive and distributed by metastasis and implantation.
The cause of dermoid tumors of the ovary is unknown. Several different theories have been advanced, no one of which seems to be generally acceptable.
There is an interesting variety of ovarian cysts which is characterized by the presence of papillomata, or warts, upon the inner surface. These cysts arise from the paroöphoron or from the hilum of the ovary. Many theories have been advanced to explain the origin of these tumors. Pathologists are far from agreeing upon this subject. Perhaps the most popular view among English and American pathologists is that the papillomatous cysts originate from the remains of the Wolffian body which may persist in the paroöphoron in various stages of degeneration.
As paroöphoritic cysts spring from the hilum or the attached portion of the ovary, and develop in the direction of least resistance, they very often separate the lamellæ of the mesovarium and invade the loose connective tissue between the layers of the broad ligament. These cysts are thus very often extra-peritoneal or intra-ligamentous in their development. 363
Some writers of experience state that three-fourths of all papillomatous tumors of the ovary are of intra-ligamentous growth. This has not been the experience of the author. The majority of the papillomatous ovarian cysts that he has seen have been intra-peritoneal in development, and have had as well-defined pedicles as the ordinary multilocular ovarian cyst.
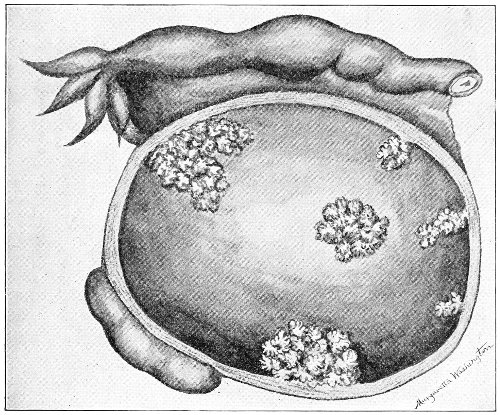
Fig. 168.—Papillomatous cyst of the paroöphoron. The section shows the papillomatous growths in the interior and the relation of the oöphoron.
Cyst-wall.—If the papillomatous cyst be intra-peritoneal in development, two layers of tissue may be distinguished in its wall: an outer dense layer, composed of laminated connective tissue which sometimes contains unstriped muscle-fibers; and an inner loose layer of fibrous tissue. Both layers contain numerous blood-vessels.
If the cyst be extra-peritoneal or intra-ligamentous in 364 its development, we find, in addition to the two layers just described, an outer coat of peritoneum which is derived from the broad ligament.
The internal surface of the cyst—the walls and the papillæ—is covered by a single layer of cylindrical epithelial cells, which may become flattened by pressure in the large cysts. The epithelium is often ciliated.
Upon the interior of the papillomatous cyst are found warts or papillary growths. These growths vary in size from that of a grain of sand to that of the fetal head. They may be scattered over the cyst-wall or collected in groups. The larger growths often form arborescent, cauliflower-like masses, which may be so numerous and luxuriant that rupture of the cyst results.
In color the papillomata vary from whitish to dark red or black, according to the vascular supply. They are sometimes yellow as the result of fatty degeneration. They are usually very vascular, and bleed freely when manipulated.
The papillomata may be sessile or pedunculated. The pedicle is sometimes very long and thin. Calcification of the papillomata often takes place.
Papillary cysts are usually unilocular. In any case the number of secondary loculi is much smaller than in the glandular cyst.
Fluid Contents.—The fluid contents of the papillomatous cyst differ considerably from those of the glandular cyst of the ovary.
In the papillomatous tumor the contents are usually clear and of a watery consistency, with a specific gravity of from 1005 to 1040. They are not often thick, mucous, or gelatinous in consistency, as in the glandular cyst. The color varies from light yellow to dark brown from admixture of blood. As in all cystic tumors, the character of the contents depends upon the accidents that have happened during the growth of the cyst.
Papillomatous cysts are more often bilateral than any 365 other cystic tumors of the ovary. They affect both ovaries in from 50 to 75 per cent. of the cases. For this reason the operator should always carefully examine the second ovary after removing an ovarian cyst, for beginning cystic degeneration may be found in it also.
Papillary cysts are usually of smaller size and of slower growth than glandular cysts. The papillomata usually perforate the cyst and invade the peritoneum before large size has been attained. These tumors, therefore, are not often seen of larger size than the adult head.
Though papillomatous cysts of the ovary are not as common as the glandular cystomata, yet they are by no means unusual. The statistics of operators vary a great deal. In 600 ovariotomies Schroeder found 50 papillomatous cysts—somewhat over 8 per cent. In the experience of the writer they have been very much more frequent than this.
The papillomatous cyst is the most dangerous cyst affecting the ovary. The danger lies in metastasis of the papillomatous growths to the general peritoneum. Metastasis occurs from the perforation of the cyst-wall and the escape into the peritoneum of the papillomatous masses.
The tendency to rupture of the cyst-wall is one of the characteristics of this form of tumor. The wall becomes weakened by atrophy or fatty degeneration, or by direct pressure of the luxuriant papillary growths. These growths make their way to the outer surface of the cyst, and extend thence throughout the peritoneum; or, if rupture takes place, the cyst may become so inverted that the site of each ovary is occupied by a mass of papillomata; the formerly enclosing cyst has disappeared, and its remains can be discovered only by careful dissection (Fig. 169). Such a condition has undoubtedly often been mistaken for primary papilloma of the ovary, the real origin in a papillomatous cyst not having been detected.
The secondary affection of the peritoneum is due not only to continuity of tissue, but to implantation and 366 growth of portions of papillomata that have become broken off and carried to different parts of the peritoneal cavity. Such secondary growths may extend throughout the whole abdomen from the pelvis to the diaphragm, covering any of the viscera. They resemble in all respects the original papillomata found in the interior of the ovarian cyst. They sometimes form cauliflower-like masses as large as the fist, and may be palpated through the abdominal wall. They are very vascular, and bleed profusely on being handled. The smallest particles of papillomata are capable of infecting the peritoneum or other tissues in this way.
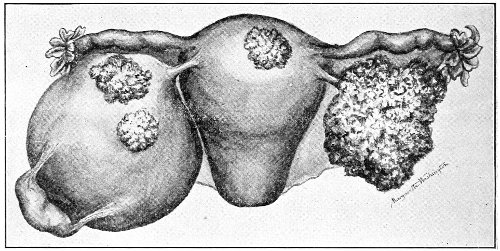
Fig. 169.—Double papillomatous cyst of the ovary. The right cyst has ruptured and is turned inside out, showing a mass of papillomata. Papillomata have penetrated the wall of the left cyst. The peritoneum has been infected, and a papillomatous growth appears on the fundus uteri.
The escape of a small quantity of the cyst-fluid into the abdomen during the removal of the tumor may cause subsequent recurrence in the peritoneum. Secondary development of the growth in the abdominal cicatrix, or its appearance in the site of puncture after tapping, is due to the same cause.
Papillomata of the peritoneum are usually accompanied by ascites. This is a prominent symptom in those cases of papillomatous ovarian cyst in which secondary infection of the peritoneum has taken place. In rare cases 367 ascites is present, though perforation of the cyst and involvement of the peritoneum cannot be detected.
Sometimes perforation of the cyst takes place into adjacent organs, especially if the growth be intra-ligamentous. In such cases the papillomatous masses may protrude into the bladder, the rectum, or the cavity of the uterus. 368
The parovarium consists of a series of fine tubules lying between the layers of the mesosalpinx. It may be seen in the fresh specimen by holding the mesosalpinx stretched between the eye and the light (Fig. 145).
The typical parovarium consists of three parts: a series of vertical tubules; a series of outer tubules free at one extremity; and a larger longitudinal tubule.
The vertical tubules range from five to twenty-four in number. They converge somewhat toward the ovary, where they end in blind extremities and become closely associated with the paroöphoron. At the other end they terminate in the larger longitudinal tubule.
The series of outer tubules are called Kobelt’s tubes. They are free and closed at the distal extremity, while at the proximal extremity they join the longitudinal tubule. The larger longitudinal tubule is called the duct of Gärtner. It may sometimes be traced traversing the broad ligament to the uterus, and through the walls of this organ and of the vagina to its termination at the urethra. It corresponds to the vas deferens in the male. When persistent in the vaginal wall it may become the starting-point of a vaginal cyst.
The vertical tubes of the parovarium are from 0.3 to 0.5 millimeters in diameter. They are occasionally found lined with ciliated columnar epithelium. Usually they contain a granular detritus representing the remains of broken-down epithelium.
Cysts may arise from any of the parts of the parovarium.
Kobelt’s tubes frequently become distended, and form 369 small pedunculated cysts about the size of a pea. They are of no clinical importance (Fig. 145). They are often observed in operations for ovarian disease, and are very often mistaken for the hydatid or the cyst of Morgagni which springs from the Fallopian tube, and which has already been described.
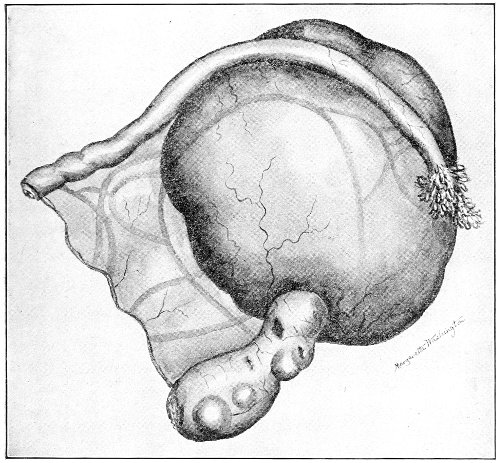
Fig. 170.—Cyst of the parovarium. There is no distortion of the ovary. The Fallopian tube has been much elongated.
The difference between these two varieties of small cysts may be determined by careful examination of the point of origin and by means of the microscope. Sutton states that the cyst of Morgagni has muscular walls and is lined by ciliated columnar epithelium. In the cyst of Kobelt’s tubes the walls are fibrous and the lining is cubical epithelium.
Large cysts of the parovarium originate from the vertical 370 or the longitudinal tubules, and usually remain sessile and develop between the layers of the mesosalpinx and the broad ligament. As the cyst grows and separates the layers of the mesosalpinx, it comes into close relationship with the Fallopian tube. This structure, being held by its uterine connection and the tubo-ovarian ligament, becomes stretched across the surface of the cyst and very much elongated. The elongation of the Fallopian tube is a very constant accompaniment of parovarian cysts. The tube may attain a length of 15 or 20 inches. The fimbriæ may also become much stretched and elongated by the traction of the growing cyst, and may attain a length of 4 inches.
The ovary is unaffected unless the cyst be of very large size, in which case the ovary may be stretched upon the surface of the cyst, so that its position becomes difficult to determine.
There are two varieties of parovarian cyst—the simple and the papillomatous.
The simple parovarian cyst has a very thin wall of uniform thickness. In small cysts, less than the size of a child’s head, the wall may be transparent. It is of a light yellowish or greenish color, and the fine vessels ramifying upon the surface are plainly visible. As one would expect from the direction of growth, the outer covering of the cyst is peritoneum, which is not adherent and may be readily stripped off. The middle coat is composed of fibrous tissue containing unstriped muscle. The lining membrane is ciliated columnar epithelium, stratified epithelium, or simple fibrous tissue, according to the size of the cyst. The changes in the character of the epithelium are due to pressure. The cyst-contents are a clear, limpid, opalescent fluid of a specific gravity below 1010.
In the papillomatous parovarian cyst the interior is covered with warts or papillomatous growths resembling in every respect those that occur in the cyst of the paroöphoron, already described. The papillomatous parovarian 371 cyst exhibits the same clinical features, and is liable to the same accidents, as the paroöphoritic cyst. It may become perforated and infect the general peritoneum.
The walls of the papillomatous parovarian cyst are somewhat thicker than those of the simple parovarian cyst; the fluid contents are not so clear and limpid, and may contain altered blood that has escaped from the papillomata.
Parovarian cysts are almost invariably unilocular. Only a few cases have been reported in which two or more cavities were present.
The cysts are of small size, not often exceeding that of a child’s head. They may, however, attain large dimensions and contain several quarts of fluid.
Parovarian cysts are of very slow growth, and refill but slowly after tapping or rupture. On account of the thinness of the cyst-walls, these cysts seem especially liable to the accident of rupture. Unless the cyst be papillomatous, the bland, unirritating fluid is readily absorbed by the peritoneum, and the cyst may remain quiescent for a long period.
Cysts of the parovarium occur most frequently during the period of active sexual life. Unlike dermoids and cysts of the oöphoron, they are unknown in childhood.
Cysts of the parovarium are much less common than cysts of the oöphoron and paroöphoron. In 284 tumors of the ovary and parovarium operated upon by Olshausen, about 11 per cent. originated in the parovarium.
Some authorities maintain that in rare instances dermoid cysts may arise from the parovarium.
The symptoms of parovarian cysts resemble those of ovarian cysts of similar development. On account of the intra-ligamentous development of the tumor, pressure-symptoms may appear early. The cyst is of such slow growth that the simple parovarian cyst may exist for a long time without giving any trouble whatever. The slow growth is the only clinical feature that would enable one to make a diagnosis between parovarian and ovarian cyst. 372
The chief characteristic features of the large cysts of the. ovary and the parovarium—the glandular cyst, the paroöphoritic cyst, and the parovarian cyst—may be tabulated for comparison as follows:
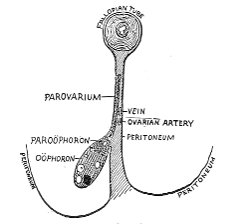 |
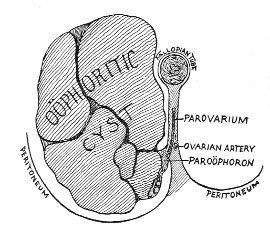 |
Fig. 171.—Section, perpendicular to the long axis of the Fallopian tube, passing through the tube, the parovarium, and the ovary; showing the relation of the structures to the peritoneum of the broad ligament. |
Fig. 172.—Section, perpendicular to the long axis of the Fallopian tube, showing the relation of an oöphoritic cyst to the peritoneum of the broad ligament. |
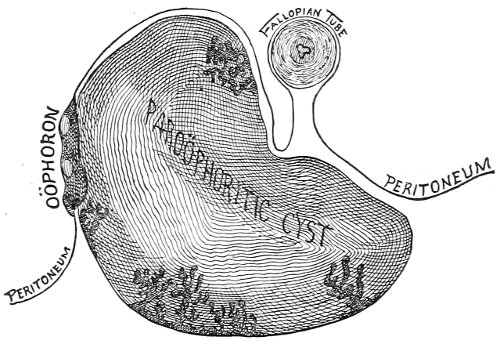
Fig. 173.—Section, perpendicular to the long axis of the Fallopian tube, showing the relation of a paroöphoritic cyst to the oöphoron and the peritoneum of the broad ligament.
Glandular Oöphoritic Cyst.—Intra-peritoneal in development; 373 no peritoneal investment. Ovary destroyed early in the course of the disease. Cyst multilocular.
Fluid contents thick, colored; specific gravity greater than 1010.
Tumor of rapid growth.
Usually unilateral.
Fallopian tube distinct from tumor, and not much, if any, elongated.
Paroöphoritic Cyst.—Often extra-peritoneal in development, in which case there is a detachable peritoneal investment.
Oöphoron not at first involved by the growth.
Unilocular.
Fluid contents less thick and viscid than in oöphoritic cyst.
Interior filled with papillomata.
Tumor usually of slower growth than the oöphoritic cyst.
Very often bilateral.
Fallopian tube more likely to be involved than in oöphoritic cyst.
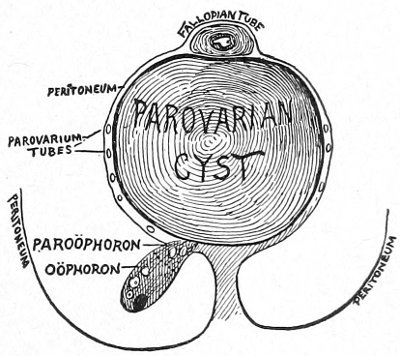
Fig. 174.—Section, perpendicular to the long axis of the Fallopian tube, showing the relation of a parovarian cyst to the ovary, the tube, and the peritoneum of the broad ligament.
Cysts of the Parovarium.—Intra-ligamentous in development. Peritoneal investment which may be stripped off.
Ovary pushed aside, but shape not affected unless the cyst be very large.
Cyst unilocular.
Wall thin. Fluid contents watery, opalescent; specific gravity below 1010.
May or may not have papillomata in interior.
Tumor of very slow growth.
Usually unilateral.
Fallopian tube much elongated and stretched immediately over the surface of the cyst. 374
In the discussion of the secondary changes, the clinical history, and the treatment of cysts, the oöphoritic, paroöphoritic, and parovarian cysts will be considered together under the general heading of ovarian cysts.
There are various accidents which may happen to an ovarian cyst which have an important bearing on the clinical course of the disease. These accidents are: inflammation and suppuration; torsion of the pedicle; rupture of the cyst.
Inflammation and Suppuration.—Inflammation of an ovarian cyst is of very common occurrence. It seems especially liable to happen in the small cysts of pelvic growth. Ovarian dermoids are very often inflamed. The inflammation may result in but a few peritoneal adhesions between the outer surface of the cyst and some of the contiguous structures, as a loop of intestine, the bladder, the anterior abdominal wall, the omentum, etc., or the whole cyst may be universally adherent, so that its removal is rendered most difficult, and in some cases impossible.
The operator should always remember the possibility of these adhesions in removing an ovarian cyst. Its surface should be carefully examined as it is dragged slowly through the abdominal incision, in order that slight adhesions to delicate structures like the omentum and the vermiform appendix may not be recklessly or unknowingly torn. 375
The sources of inflammatory infection of an ovarian cyst are the intestinal tract, the urinary bladder, and the Fallopian tube. Perhaps salpingitis is the most frequent cause of such inflammation. Infection often comes from the vermiform appendix, which is frequently found adherent to the surface of the tumor.
Old adhesions usually contain blood-vessels, which may be of large size, especially if they arise from the intestine, the omentum, or the uterus. In some cases in which the tumor has become detached from the pedicle by rotation or traction the adhesions have been sufficiently vascular to maintain the vitality of the tumor.
Suppuration of ovarian cysts is sometimes seen. It was more frequent in the period when these tumors were treated by tapping, as infection occurred in this way.
Suppuration is most common in ovarian dermoids. The tumor may become adherent to surrounding structures, and may discharge its contents through the bladder, the vagina, the rectum, or the abdominal wall. A tooth thus discharged into the bladder from a suppurating dermoid has in several instances formed the nucleus of a vesical calculus.
A suppurating ovarian cyst sometimes contains gas, either from communication with the intestine or from decomposition of its contents. In such a case the usual tumor-dulness is replaced by a tympanitic note.
Torsion of the Pedicle, or Axial Rotation.—Ovarian tumors occasionally rotate upon their axes, so that the structures that form the pedicle become twisted. The severity of the symptoms that arise from this accident depends upon the degree of compression to which the vessels of the pedicle are subjected from the torsion.
The accident is not now as common as formerly, because the tumor is, as a rule, now removed as soon as it is recognized, and many of the accidents that were described as very frequent by the older writers are avoided. The many recorded cases—chiefly of a date before our present surgical era—show that axial rotation occurred in 376 about 10 per cent. of the cases of ovarian and parovarian tumors. Rokitansky found torsion of the pedicle in 12 per cent. of all cases of ovarian tumors, and in 6 per cent. of the cases it was the cause of death.
The cause of axial rotation is unknown. It has been attributed to alternate distention and evacuation of the bladder, to the passage of feces through the rectum, and to a sudden jar or motion of the body.
The accident is especially likely to occur when an ovarian cyst complicates pregnancy or when both ovaries are cystic. Torsion of both pedicles has been found in women suffering with bilateral ovarian cysts.
Torsion of the pedicle is more apt to occur in cysts of medium and small size than in the large tumors.
Torsion of the pedicle affects equally tumors of the right and left sides. The direction of rotation is usually toward the median line, though it may take place in the reverse direction.
There is considerable variation in the amount of rotation. In some cases the pedicle has twisted through but half a circle, while in others twelve complete twists have been found. A pedicle twisted in this way resembles a rope. Such a high degree of torsion is the result of a slow or chronic process. The rotation of the tumor takes place so gradually, or the arrangement of the blood-vessels in the pedicle is such, that no appreciable effect upon the tumor is produced, and no symptoms arise from it. The operator frequently meets examples of such slow torsion in removing ovarian tumors. In extreme cases the twisting progresses until the blood-supply through the pedicle is arrested, and the cyst may become freed from its peduncular attachment. If adhesions had formed to the cyst-wall, the vitality may be maintained through these channels; the tumor, in fact, becomes transplanted. This phenomenon is most frequent with dermoids.
Very different are the phenomena of acute torsion. Here the vascular supply of the tumor is so suddenly and markedly interfered with that most urgent symptoms 377 immediately arise. The interference with the circulation depends upon the amount of the twist and the character of the pedicle. The effect is first felt by the veins, which are more compressible than the arteries; the venous blood-current becomes obstructed, while the arteries remain open. Venous engorgement of the cyst results; extravasation of blood takes place in the walls, or the veins may rupture and hemorrhage may take place into the cyst-cavity. Death from acute anemia may result from this cause. Thrombosis and necrosis of the tumor may occur as a result of acute torsion.
Rupture of Ovarian Cysts.—Rupture of an ovarian cyst is an accident of not infrequent occurrence. It is probable that small cysts rupture and refill without the attention of the woman or the physician being directed to the accident. The scars of old ruptures are frequently found on the surface of ovarian cysts. Wells found rupture of the cyst 24 times in a series of 300 ovariotomies.
There are various causes which predispose to rupture or lead to it. As the cyst enlarges, the walls become very thin as a result of the distention. The cyst-wall may undergo, in places, retrograde changes—atrophy and fatty degeneration. The wall may become weakened as a result of suppuration, thrombosis, and the results of torsion of the pedicle; and, as has already been said, papillomatous growths destroy the integrity of the wall and lead to perforation.
The immediate cause of the rupture is usually a sudden jar or a fall. Sometimes very slight pressure is enough to rupture the cyst. The manipulations of a physician, turning in bed, and coughing have caused this accident.
The effects of rupture depend upon the character of the cyst-contents.
Hemorrhage may be profuse and rarely fatal. The hemorrhage, however, is usually not severe, because the rupture takes place in the attenuated part of the cyst, which is but poorly supplied with blood-vessels. 378
If the fluid is unirritating to the peritoneum and contains but little solid material, it is often readily absorbed by the peritoneum and passed off by the kidneys. Large quantities of fluid may be absorbed and eliminated in this way. A case has been reported in which the rupture of a cyst was followed by profuse diuresis which lasted four days, during which time 65 pints of urine were discharged.
Another case has been reported in which the cyst ruptured and refilled 34 times during a period of nine years. The fluid on each occasion was absorbed by the peritoneum and discharged by the kidneys without in any way incapacitating the woman.
If the cyst-contents are septic, as is often the case in dermoid cysts, fatal peritonitis will result. The danger of rupture of the papillomatous tumors—general papillomatous infection of the peritoneum—has already been described.
Similar infection may rarely occur from the escape into the peritoneum of the colloid contents of a ruptured glandular cyst. After such an accident the peritoneum has been found covered with tough gelatinous masses, of a gray or yellow color, which reached the size of a hickory-nut. This condition has been called myxoma peritonæi.
Very rare cases of similar metastasis from rupture of dermoid cysts have been reported. In one case yellow nodules the size of a pea, containing light-colored hair, were found scattered upon the peritoneum.
It is probable that when the walls of an ovarian cyst are very thin, slow transudation of the fluid into the peritoneum takes place.
The symptoms produced by ovarian cysts depend upon their size, their position, and the accidents that may arise. If the tumor be intra-peritoneal in its development, the woman’s attention is usually first directed to the pathological 379 condition when the growth has attained sufficient size to extend above the pelvis. The time of the perception of the tumor depends upon the intelligence and powers of observation of the woman and the thickness of the abdominal wall. A cyst often attains a large size and reaches well up into the abdomen before the woman is aware of its existence. In the papillomatous cysts sometimes the first symptoms that attract the woman’s attention appear after the cyst has become perforated and the peritoneum has become invaded by the papillomata.
Pain, except that due to pressure or inflammation or some other accident, is not at all characteristic of ovarian cysts.
If the cyst be intra-ligamentous in development, or if it be wedged in the pelvis, the first symptoms of the disease appear at an earlier date. The intra-ligamentous tumors first separate the layers of the broad ligament; they push the uterus to one side, and press upon the bladder, ureters, and rectum. The disposition of the peritoneum may be altered in a variety of ways by these growths. They may grow altogether behind this membrane, becoming retro-peritoneal, coming into immediate relationship with the rectum; or they may pass behind the cecum and the ascending colon, growing between the layers of the mesocolon. They sometimes develop more especially under the anterior layer of the broad ligament, strip off the peritoneal covering of the bladder, and come into immediate relationship with the anterior abdominal wall; so that if laparotomy is performed, the operator will enter the cavity of the cyst before he has opened the general peritoneum. It is of the greatest importance that the surgeon should be familiar with such unusual ways of development of these tumors, as the operative difficulties that are encountered are most embarrassing.
Pressure upon the ureters occurs not only in the cysts of intra-ligamentous growth, but also in the large-sized intra-peritoneal tumors. It is a frequent complication, 380 and the hydronephrosis and kidney-degeneration that result may be the immediate cause of death.
Doran says that in 32 cases out of 40 autopsies on women with large ovarian tumors, kidney disease, probably caused by pressure of the tumors, was present. The writer has found a ureter distended to an inch in diameter from pressure of a papillomatous cyst. The pressure of the tumor sometimes produces edema of the lower extremities and of the anterior abdominal walls.
The presence of ascites with cysts of papillomatous nature has already been spoken of. Though this complication is especially characteristic of these tumors, and usually indicates peritoneal involvement, yet it is sometimes found with the glandular and the dermoid cysts. In these cases it is caused by the direct mechanical irritation of the peritoneum by the movable tumor. It accompanies also freely movable solid tumors of the ovary and pedunculated fibroids of the uterus.
Notwithstanding the gross disease of the ovaries, the functions of the uterus are in no way specifically affected by ovarian cysts. The uterus may be pushed to one side, pressed backward into the hollow of the sacrum or forward against the pubis, but menstruation may not be affected, and conception may take place even with tumors of very large size.
In some cases there is menorrhagia, or continuous bleeding, which appears with the appearance of the cyst and disappears after its removal. This phenomenon may occur in old women who have long passed the menopause, and may excite the suspicion of coincident malignant disease of the uterus. On the other hand, menstruation may be diminished or arrested.
Reflex disturbances in the breast may occur with ovarian cysts, as in any form of ovarian disease. The areola may become pigmented, the breasts swell, and a milky secretion may be produced even in young girls.
Malignant degeneration may occur in any form of ovarian cyst. It seems to be most frequent in the papillomatous 381 tumors, next in the dermoids, and less frequent in the glandular cysts.
The rapidity of growth of ovarian cysts varies a great deal. The glandular tumors are of the most rapid development. They sometimes attain a very large size within a few months. The rate of accumulation of the fluid depends upon the intracystic pressure, and is consequently greatest immediately after rupture or tapping. Some remarkable cases of great rapidity of accumulation after tapping have been reported. In one case 90 pints of fluid reaccumulated in seven weeks—a rate of about 2 pints a day. In another case 3½ pints of fluid were accumulated every day.
The enormous size attained by ovarian cysts, and the tremendous amount of fluid drawn off from them, are shown by the old records of the days when tapping the cyst was the only treatment. A few references will illustrate this. In one case 1920 pints of fluid were drawn off by 66 tappings in a period of sixty-seven months. In another case 2787 pints were withdrawn by 49 tappings. In another case 9867 pounds were withdrawn by 299 tappings. The fluid in these remarkable cases must have been of low specific gravity, containing but little solid matter, or the women would have sooner succumbed from the drain on the system.
The misery of the women who were slowly crowded out of existence by these enormous tumors, or who, though with life prolonged by tapping, were exhausted by the continuous drain, was depicted in their countenances. The expression was called the facies ovariana. We do not often see it at the present day. Wells describes it thus: “The emaciation, the prominent or almost uncovered muscles and bones, the expression of anxiety and suffering, the furrowed forehead, the sunken eyes, the open, sharply defined nostrils, the long, compressed lips, the depressed angles of the mouth, and the deep wrinkles curving around these angles, form together a face which is strikingly characteristic.” 382
The natural duration of life depends upon the character of the ovarian tumor. A dermoid may exist from childhood and give no trouble—in fact, may not be recognized until some accident starts it into rapid development. Even then it is of comparatively slow and limited growth, and danger from it is due to the accidents, such as inflammation and suppuration, to which it is especially liable.
Though the papillomatous cyst is also of slow growth when compared with the glandular cyst, yet the danger here is due to peritoneal infection, which very often takes place before the tumor has, by its size, begun to annoy the woman.
The glandular cyst, however, is of rapid, continuous, unlimited growth, and usually destroys the woman within a period of three years. Life has been prolonged for a much longer period in some cases by palliative treatment and tapping. On the other hand, life may at any time be cut short by the occurrence of some accident, such as rupture or torsion of the pedicle.
Symptoms of the Accidents that occur in Ovarian Cysts.—The symptoms of inflammation are pain and tenderness over the surface of the tumor. The tenderness is often limited to a local area which marks the position of an intestinal adhesion.
When suppuration takes place, the symptoms indicative of the presence of pus appear—elevated temperature, rapid and feeble pulse, exhaustion, and emaciation.
Symptoms of Torsion of the Pedicle.—There are no characteristic symptoms of slow or chronic torsion, unless, perhaps, retardation of the growth of the tumor appears as a result of the interference with the circulation.
The symptoms of acute torsion are, however, very marked. The woman is seized with sudden and violent pain in the abdomen, accompanied by vomiting and collapse. Sometimes the abdomen becomes rapidly increased in size on account of the venous engorgement of the 383 tumor. If a woman known to have an ovarian tumor is thus attacked, the diagnosis of torsion of the pedicle may be made. The diagnosis is rendered more probable if the woman is also pregnant or if she has been recently delivered. If the woman presents herself for the first time to the physician with these acute symptoms, and he finds by abdominal and pelvic examination that there is an ovarian tumor, he should suspect that torsion of the pedicle has occurred.
Rupture of the Cyst.—Rupture of an ovarian cyst usually follows a fall, a violent attack of coughing, vomiting, etc.
The woman is seized with sudden pain in the abdomen, with perhaps symptoms of collapse and loss of blood.
The shape of the abdomen becomes quickly altered from that characteristic of encysted fluid to that characteristic of free fluid in the peritoneum. The alteration in shape is so marked that it may readily be perceived by the patient.
These phenomena are followed by profuse diuresis, or perhaps by symptoms of peritoneal inflammation.
If the woman survive, there is a gradual reaccumulation of fluid and a return of the abdomen to the former shape.
Examination.—In the early stages of an ovarian cyst, while it is in the pelvic state of development, bimanual examination will reveal the condition. The tumor lies to the side, to the front, or behind the uterus. The uterus may be moved independently of the tumor. The cystic character of the growth may often be determined by palpation; fluctuation may be felt between the vaginal finger and the abdominal hand. If the tumor be intra-peritoneal, with a pedicle, it will be found to be movable, and may be pushed out of the pelvis up into the lower abdomen. If it be intra-ligamentous, the range of motion is limited, the tumor is situated lower in the pelvis, and is in closer relationship with the uterus.
The shape of the tumor is usually spherical. In a multilocular cyst the surface may be lobulated; in a dermoid 384 cyst the pultaceous character of the contents may sometimes be determined by pressure with the vaginal finger.
When the tumor has attained a sufficient size to have extended into the abdomen, much may be determined by careful abdominal examination. The woman should lie upon the back, and all constricting clothing should be removed. The whole abdomen should be exposed.
The bulging or prominence caused by the cyst is usually apparent in a thin woman. It commonly occupies the middle of the abdomen, but when not very large may lie to either side.
Palpation reveals the smooth, spherical character of the growth, or the lobulated surface from the presence of secondary cysts. Perhaps an area of marked tenderness may be discovered, which often shows the seat of peritoneal inflammation and adhesion. In the papillomatous tumors that have become perforated, irregular masses of papillary growths may sometimes be felt through the abdominal walls, situated either on the surface of the tumor or in some other portion of the abdomen. The association of such masses with a cystic tumor of the ovary and ascites renders the diagnosis of papillary cysts very certain.
If the tumor is non-adherent and of medium size, it may be moved from side to side or upward in the abdomen.
Fluctuation may often be elicited by palpation, and is most marked in the unilocular cysts with thin contents. If the contents be thick, as in many of the glandular cysts, or if the cyst be multilocular, fluctuation may not be obtained. The wave of fluctuation is interfered with by intervening septa.
Percussion reveals a central area of flatness which marks the most prominent part of the tumor. Intestinal resonance may be obtained above and to the sides of the cyst, and in some cases below it. In instances of this kind a central area of flatness is found surrounded by a ring of resonance. 385
This phenomenon is very different from that which appears if the fluid accumulation is free in the peritoneum. In the latter case the fluid gravitates to the flanks when the woman is upon her back, and the intestines float to the front, so that there is a central area of resonance, with dulness to the sides. In the very unusual cases in which gas is contained in the cyst-cavity the area of flatness will be replaced by an area of a tympanitic note.
If the woman sits up or lies on either side, the relation between the areas of flatness and resonance is unaltered in the case of an ovarian cyst, while, as is well known, if the fluid be free it will gravitate to the most dependent portion of the abdomen.
Auscultation reveals nothing of importance in regard to ovarian tumors. It is of value in enabling one to make a differential diagnosis between an ovarian tumor and pregnancy.
Vaginal examination in the case of a large tumor shows the character and the position of the lower portion of the growth, and sometimes enables the physician to determine upon which side the tumor had started. In ruptured papillomatous cysts the papillary masses may sometimes be felt behind the uterus when they cannot be detected by the abdominal hand.
The details of the natural history and pathological features already given will often enable the physician to make a differential diagnosis among the different kinds of ovarian cysts. Such a differential diagnosis, however, is of no importance whatever, as all such tumors require similar operative treatment.
To discuss the subject of the differential diagnosis of ovarian cysts from other pelvic and abdominal tumors would require a consideration of all the pathological growths that may occur in the abdomen. About every form of abdominal tumor has been mistaken for ovarian cyst. Differential diagnosis is here also of but little importance at the present day if the examiner is able to 386 exclude pregnancy, phantom tumor, and fat. Operation is indicated in practically all morbid growths of the abdomen, with the exception of inoperable malignant disease; no surgeon should undertake any abdominal operation unless he is prepared to deal with any condition that may be found.
The difficulty of making a differential diagnosis is well illustrated by many cases that have been recorded, in which it was impossible to determine the true nature of the tumor even after the abdomen had been opened.
It is of the greatest importance to exclude pregnancy. Many women have been subjected to the operation of celiotomy because the pregnant uterus was mistaken for an ovarian tumor. Women themselves often intentionally mislead the physician, especially if the pregnancy is illegitimate. They will even carry the deception so far as to go upon the operating table with the full knowledge that they have deceived the surgeon as to their condition.
The physician should always remember the possibility of pregnancy in examining any form of abdominal tumor in women. The mistakes that have happened have usually been the result of carelessness or ignorance on the part of the physician, though some of the most experienced operators have made this error.
The separation of the uterus by bimanual examination as distinct from the abdominal tumor is the most valuable point in the differential diagnosis.
The complication of pregnancy with an ovarian cyst renders the diagnosis more difficult.
It is easier to make a differential diagnosis between an ovarian cyst and pregnancy than between some forms of uterine fibroid and pregnancy.
Repeated examinations are often necessary. It is always advisable, in any case, to make two or more examinations before subjecting the woman to operation. Much which was not at first apparent may be learned by several days of watching and repeated examination.
Phantom tumor is a rare condition. A woman imagines 387 that she is suffering from a tumor and that her abdomen is increasing in size. The condition is likely to occur at the menopause, and there may readily be some physical grounds for the woman’s suspicions, because there may be a constantly increasing accumulation of fat in the abdominal walls and the omentum.
The diagnosis is usually easily made. Careful palpation and percussion fail to reveal any pathological mass in the abdomen or any abnormal area of dulness. In these cases the abdomen is often rendered prominent by intestinal tympany. If any difficulty is experienced at the examination, the woman should be etherized. If a satisfactory diagnosis cannot be made, the case should be watched. Several cases have been reported, and there are probably many unreported, in which no tumor was found after the abdomen had been opened.
A fat abdominal wall or omentum has often been mistaken by the woman, and not infrequently by the physician, for a tumor. These cases are often obscure; indeed, all the difficulties of examination, in case a tumor be present, are very much increased by the enormous deposits of fat that are often present in the abdomens of women.
Careful examination, sometimes with anesthesia, and, if necessary, prolonged watching should be practised. If a fold of the abdominal wall be picked up between the hands, it will often show how much of the abdominal enlargement is due to fat.
Tapping.—At one time the universal method of treating cystic tumors of the ovary was by tapping, or puncture through the abdominal wall. Many women were subjected to this proceeding a very great number of times, and, though not cured, were enabled to drag on a miserable existence until death resulted from exhaustion or from some accident to the cyst. In a few cases the cyst refilled very slowly, relief being experienced for several 388 years before a second tapping became necessary. In still fewer cases the tapping seemed to be curative, the tumor never reappearing after it had been evacuated. Such cases were so unusual that they should have no influence whatever in determining the method of treatment. In the great majority of instances the cyst rapidly refilled. Sometimes the fluid accumulated with such rapidity that evacuation became necessary every few days. Referring again to the old records, we find a case which was tapped 664 times in thirteen years—once in about seven days!
If the cyst were multilocular, tapping furnished but partial relief.
The proceeding itself was attended by serious dangers. Dr. Fock of Berlin in 1856 stated that 25 out of 132 women—or 1 in 5½—died within some hours or a few days after the first tapping. Another operator lost 9 out of 64 cases—or very nearly 1 in 7—within twenty-four hours after the first tapping. The chief mortality occurred in the cases of multilocular tumors. Tapping the unilocular tumors was attended by much less danger.
The sources of danger from tapping were the following: hemorrhage from puncture of a vessel in the cyst-wall; septic or other infection of the peritoneum; and inflammation or suppuration of the cyst.
The majority of the women died in consequence of peritoneal infection.
The danger arose not only from septic infection of the peritoneum, but from papillomatous or other infection from the escape into the peritoneal cavity of some of the cyst-contents. Reference has already been made to the occurrence of the papillomatous infection at the site of puncture in the abdominal wall.
At the present day tapping an ovarian cyst with the hope of cure is never practised.
Tapping as a palliative procedure should never be performed. The dangers that may result from the tapping cannot be disregarded, and no hope whatever of cure can 389 be held out to the patient. When operation is finally performed, it is rendered much more difficult from the adhesions that have resulted from previous tappings.
Operation.—The treatment of ovarian cysts is operative. Celiotomy should be performed and the tumor removed without delay. The dangers due to the accidents that may occur show the risk of waiting after a diagnosis has been made. When the tumor is small the operative complications and dangers are at a minimum.
Even if the tumor be discovered accidentally by the physician, and has never given any trouble to the woman, operation for its removal should be advised. A dermoid that has existed for years may suddenly endanger the woman’s life. Delay in the case of papillomatous tumors—and no one can determine in the early stages whether or not a cyst be papillomatous—is especially dangerous. About one-half the women upon whom I have operated for papillomatous cysts have come to me after the peritoneum had become infected. Though the peritoneum be extensively involved, operation is by no means hopeless. As in the case of tuberculosis of the peritoneum, so in papilloma, the opening and draining of the abdominal cavity may result in cure.
Pregnancy is no contraindication to operation. In fact, the dangers of obstructed labor, of rupture of the cyst, and of torsion of the pedicle urgently call for immediate operation in such cases. Pregnancy usually progresses to full term after operation. 390
Solid tumors of the ovary are of rare occurrence. They are said to be found in about 5 per cent. of all the cases of ovarian tumors that are submitted to operation.
The solid tumors of the ovary are fibromata, myomata, sarcomata, carcinomata, and papillomata.
Fibromata.—Ovarian fibromata are very rare; they are histologically similar to fibroid tumors of other parts of the body. They do not form circumscribed new growths, but affect the whole organ, which becomes uniformly hypertrophied, preserving its general shape and anatomical relations. The tumor may contain, between the bundles of fibrous tissue, small cavities filled with fluid. The growth is usually intra-peritoneal and has a well-formed pedicle; it may, however, in exceptional cases be extra-peritoneal and develop between the layers of the broad ligament. In such a case there is difficulty in determining whether the fibroid originated in the uterus or in the ovary. Ovarian fibromata are usually of small size and slow growth. A case has been reported in which the tumor weighed over 7 pounds.
Corpora Fibrosa.—A variety of the ovarian fibromata are the corpora fibrosa, which are due to fibroid degeneration of the corpus luteum. They are tough, fibrous bodies, about the size of a pea, which are occasionally found upon the surface of the ovary. It is said that they may attain the size of a child’s head. They are usually, however, very small, and have no clinical significance.
Myomata.—Ovarian myomata are composed chiefly of unstriped muscular fiber. They are somewhat more frequent than the pure fibromata. The two growths may 391 be mixed, forming a fibro-myomatous tumor. The myomatous tumor may attain the weight of fifteen pounds.
Sarcomata.—The majority of solid tumors of the ovary are sarcomatous in character, and it seems probable that many tumors that are classed as fibroids or fibro-myomata are in reality ovarian sarcomata. The growth may be either of the spindle-cell or the round-cell variety. Occasionally it is an endothelioma, a form of sarcoma developing from the endothelial cells of the blood- and lymph-vessels.
Sarcoma of the ovary differs from sarcoma in other parts of the body in the fact that it is very often bilateral. Sutton states that both ovaries are affected in about 20 per cent. of the cases. Other observers state that ovarian sarcomata are usually bilateral.
The surface of the tumor is smooth, and the general form and anatomical relations of the ovary are unaltered. Ovarian sarcomata are usually of median size, though they may attain enormous proportions and fill the abdominal cavity.
The tumor is usually of rapid growth; in one case it attained a weight of ten pounds within a period of six months. The growth is accelerated by pregnancy. Ascites is commonly present with ovarian sarcoma, and cachexia may appear rapidly.
Ascites caused by peritoneal irritation may accompany any of the solid tumors of the ovary, as other kinds of freely movable abdominal tumor. It is, however, especially characteristic of the ovarian sarcomata, and is a point of diagnostic importance.
Ovarian sarcomata differ from the fibroid and the myomatous tumors in rapidity of growth, involvement of both ovaries, and the presence of ascites. Ovarian sarcomata may occur at any age. They are relatively very frequent in children. An analysis of 60 cases of ovarian tumors in children collected by Sutton shows that sarcomata occurred 16 times.
The symptoms caused by ovarian fibromata, myomata, 392 and sarcoma are those referable to pressure and peritoneal irritation. These tumors, on account of their moderate size and great mobility, seem to be especially liable to torsion of the pedicle. They should be removed by celiotomy as soon as recognized.
Both ovaries should always be carefully examined, for in sarcoma the disease is often bilateral.
Carcinomata.—Primary cancer of the ovaries is very rare. Secondary infection of these organs is, however, of not infrequent occurrence. It is found in cases of cancer of the breast and of the uterus. In 29 cases of death from cancer of the breast, both ovaries were found to be involved in 3 cases.
Primary cancer of the ovary appears as a solid or a cystic tumor. The solid carcinomata are diffuse infiltrations of the ovarian tissue, forming pedunculated, rarely intraligamentous, ovoid or globular tumors having a smooth or slightly irregular surface. They are either of the medullary or scirrhous type. The medullary form is of rapid growth, and may reach the size of the adult head. The scirrhous form is of comparatively slow growth and smaller size, and in consistency resembles a fibroma.
The cystic carcinomata are similar in form to the multilocular glandular cysts, but are smaller, rarely reaching a greater size than that of the adult head. They are adeno-carcinomata or papillary adeno-carcinomata. The surface of the tumor, its walls, and the septa contain to a greater or less extent solid nodules or plates of various size composed of carcinomatous tissue. The nodules often have a papillary character.
Ovarian carcinoma is usually a bilateral growth. Unlike carcinoma in other parts of the body, it may, particularly the medullary form, occur in childhood. It is usually found between the ages of thirty and sixty years. Ascites is commonly present in cancer of the ovaries, the fluid being often tinged with blood; as the disease develops, edema of the lower limbs and cachexia appear.
Cancer of the ovary is an extremely malignant growth, 393 quickly extending to surrounding structures as implantations on the peritoneum, and by metastasis to distant organs. In more than 75 per cent. of the cases operated upon the disease has returned and terminated in death within the first year.
When cancer of the ovaries is secondary to cancer elsewhere than in the uterus, operation offers no prospect of cure. If the disease is secondary to cancer of the uterus, it may be possible to remove all of the affected structures.
Ovarian Papillomata.—Superficial papillomata of the ovary are of very rare occurrence. In many of the cases in which the papillomata appear to grow from the surface of the ovary there had previously been a papillomatous cyst of paroöphoritic origin, which had become perforated and perhaps inverted, so that, after the cyst had become destroyed, the growths appeared to spring from the ovarian surface. Careful dissection and search for the remains of the old cyst should always be made in such cases.
In superficial papilloma of the ovary the growths are in all respects similar to those found in the interior of papillomatous cysts. They may be isolated upon the surface of the ovary, or they may cover it so completely that the ovary is hidden from view. A section, however, will reveal the ovary lying in the centre of the growth.
The papillomata may be pedunculated or sessile. They vary in size. In some cases they form a mass larger than the adult fist.
The disease is often bilateral. Secondary involvement of the peritoneum occurs, as in the case of papillomatous cyst. The course of the disease is similar to that of a perforated papillomatous cyst. The treatment is immediate celiotomy and removal. As in the case of papillomatous cysts, involvement of the peritoneum is no contraindication to operation.
Tuberculosis of the Ovary.—Tuberculosis of the ovary is usually secondary to tuberculosis of the Fallopian tubes. In tuberculosis of the peritoneum the ovaries 394 are often found to be involved, in some cases without accompanying disease of the tube. In phthisical women the ovaries have been found, in rare instances, to be the only portion of the genital apparatus in which secondary deposit of tubercles took place.
Williams states that primary tuberculosis of the ovaries has not yet been described.
The surface of the ovary may be covered with miliary tubercles, or they may be scattered through the substance of the gland. In other cases the ovary contains cavities filled with cheesy material or pus, forming a tuberculous abscess.
There are no characteristic symptoms of tuberculosis of the ovaries. The condition is usually found at operation or at autopsy, associated with tuberculosis of the peritoneum or of some other part of the genital organs, as the Fallopian tubes and the uterus.
The treatment consists in oöphorectomy, unless operation is contraindicated on account of extensive involvement of other structures.
Tumors of the Ovarian ligament.—Fibroid and sarcomatous tumors have occasionally been found in the ovarian ligament. Doran has reported a fibroid of the ovarian ligament that weighed 17 pounds. The writer has removed a sarcoma of the ovarian ligament that weighed 5 pounds.
It is impossible to distinguish these tumors from similar growths of the ovary. They demand like treatment. 395
Congenital malformations are found in all parts of the genital tract. Some of the more common forms, like arrested development of the uterus, have been referred to in the previous pages. Others will briefly be considered here. Reference to the method of development of the sexual organs will elucidate this subject.
The Fallopian tubes, the uterus, and the vagina are developed from two embryonic structures called the ducts of Müller. These ducts become fused, first at the lower extremity, between the sixth and eighth weeks of fetal life (Fig. 175). The early genital tract thus formed is consequently divided throughout by a septum, which normally disappears during fetal development, so that there results one vaginal and uterine tract, from which the Fallopian tubes branch.
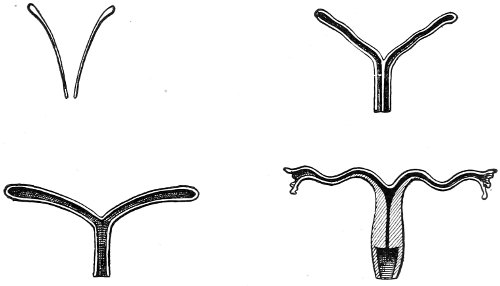
Fig. 175.—Diagrams showing the development of the vagina and the uterus from Müller’s ducts.
The most important malformations of the vagina and 396 the uterus arise from arrest, at any stage, of this normal developmental process.
Very rarely the uterus is completely absent, or it may be represented by a small band of muscular and connective tissue stretched across the pelvis. In other cases the cervix is well formed, while the body of the uterus is but poorly developed.
We have seen that this condition is often associated with pathological anteflexion of the uterus.
Uterus Unicornis.—Sometimes there is arrest in the development of one of Müller’s ducts, so that the uterus becomes one-sided or one-horned and presents only one formed Fallopian tube. In such a case both ovaries may be present.
Uterus Didelphys.—Müller’s ducts may unite only as far as the top of the vagina, no fusion whatever taking place in the uterine portion. In such a case two separated uterine bodies are produced; the condition of double uterus exists (Fig. 176).
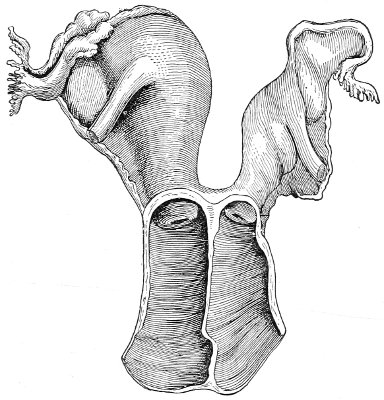
Fig. 176.—Uterus didelphys and double vagina.
Uterus Bicornis Duplex.—In this variety of malformation development has proceeded a step farther than in the 397 preceding variety. The uterine bodies have become externally united. There is, however, no fusion of the cavities. Two cavities are present, opening into a double vagina.
Uterus Bicornis Unicollis.—Here the development of the cervix and the lower part of the uterus is normal. The upper parts of the body of the uterus have not become fused, and diverge sharply from each other. The organ is two-horned (Fig. 177).
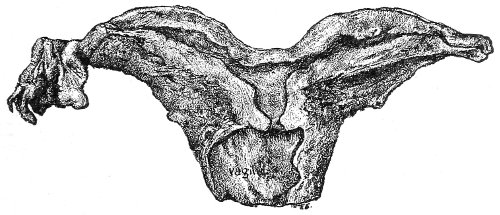
Fig. 177.—Uterus bicornis unicollis (Winckel).
Uterus Cordiformis.—In this variety the two halves of the uterus are united throughout. Externally on the fundus there appears a slight depression, which, with the broad body of the uterus, demonstrates the imperfection of development. The name is derived from the resemblance to the conventional heart-shape.
Uterus Septus.—In this variety development has progressed so far that externally the uterus presents the normal appearance. The septum that divides the two ducts has, however, failed to disappear, and a divided uterus results. The septum may extend throughout the body of the uterus, or it may be less perfectly formed. Often one side of the uterus is better developed than the other (Fig. 178).
Malformation of the Vagina.—Malformation of the vagina is frequently present with malformation of the uterus. The septum that divides Müller’s ducts may persist throughout the whole length of the vagina, forming a double vagina; or the septum may have partly disappeared, 398 being present in various stages of perfection. In double vagina each orifice may be guarded by a distinct hymen.
Sometimes one of the canals of a double vagina is much better developed than the other. The orifice of the poorly developed canal may be closed at its lower extremity, so that the malformation is never recognized by the woman or physician unless the closed canal becomes distended with blood or other secretion. A variety of vaginal cyst may be formed in this way.
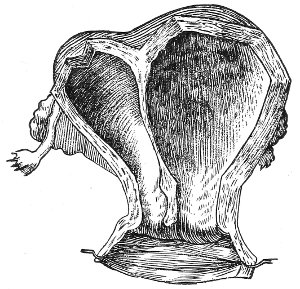
Fig. 178.—Uterus septus (Cruveilhier).
Unilateral Vagina.—In this variety of malformation one of the ducts of Müller fails to develop at all. The condition always occurs with uterus unicornis. The vaginal canal is smaller than normal and may be situated to one side of the median line.
Absence of the vagina rarely occurs. There may be no sign whatever of this structure, or it may be represented by a fibrous cord. The external genitals may also be absent, or they may be well developed.
If the uterus and ovaries are well developed, much trouble may arise from retention of menstrual blood.
An attempt should be made, by means of a transverse incision between the rectum and the urethra, to reach the 399 cervix, and, if possible, to make an artificial vagina by transposition of skin from the buttocks. Such treatment is usually unsatisfactory, as a patulous canal cannot be maintained. It may be necessary to remove the uterus and appendages.
Sometimes the vagina is absent in only part of its course, being open below and represented above by a fibrous cord; or the upper and lower portions may be developed, while the middle portion is imperforate.
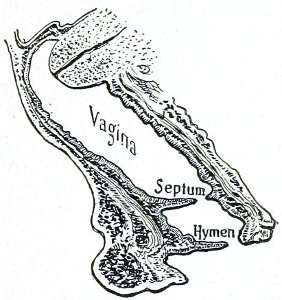
Fig. 179.—Transverse septum of the vagina (Heyder).
These conditions are more amenable to operative treatment than in the case of complete absence of the vagina. The intervening septum should be incised, and the patulous condition maintained by the passage of bougies if necessary.
Sometimes the lumen of the vagina is obstructed by the presence of transverse bands or crescentic folds, which have been described as supplementary hymens (Fig. 179).
A hematocolpos is produced when the vagina becomes distended with menstrual blood above such an obstruction.
Hermaphroditism.—A true hermaphrodite is an individual who possesses the organs of both sexes in a condition of perfect function. The existence of true hermaphroditism is denied by many authorities of the present day, though the older writers firmly believed in it. The coexistence of testicles and ovaries has never been proved beyond doubt in the human subject. It is doubtful if there are any cases, recorded as true hermaphrodites, in which the demonstration of the condition is not open to serious criticism; such individuals are in reality pseudo-hermaphrodites. The term hermaphrodite is still, however, 400 very commonly applied to any individual of doubtful sex.
A pseudo-hermaphrodite is possessed of a distinct sex, and has either ovaries or testicles, though the external genitals and other secondary sexual characteristics may present the appearance of a double sex.
In male pseudo-hermaphroditism the individual has testicles, and the external genital organs simulate those of the female.
In female pseudo-hermaphroditism the individual has ovaries, and the external genital organs simulate those of the male.
In male pseudo-hermaphroditism the condition of hypospadias is usually present, the lower surface of the urethra and the perineum being split. The penis may be very small and imperforate, the urethra opening at its base. The fissure of the perineum closely resembles the vagina, and the split scrotum may be mistaken for the labia. Cases of this kind are on record in which the individuals, ignorant of their true sex, have for years indulged in sexual connection with men.
In female pseudo-hermaphroditism there is hypertrophy of the clitoris and the prepuce, with approximation of the labia majora and contraction or occlusion of the ostium vaginæ, giving the genitals the appearance of the masculine type.
The secondary sexual characteristics of both varieties of pseudo-hermaphrodites—the distribution of hair, mammary development, shape, voice, etc.—are usually of the feminine type.
It is often exceedingly difficult to determine during life the true sex of the individual in cases of hermaphroditism. The only absolute test of the sex is the determination of the genital glands.
The labia should be carefully palpated to determine whether or not testicles are present. Rectal examination should be made to determine the existence of uterus or ovaries. The sexual inclinations of the individual should 401 be observed. The discharge from the genitals during sexual excitement should be examined for spermatozoa.
The presence of a uterus is not necessarily indicative of a female, as a uterus may be associated with a perfect penis and testes; and a periodic discharge of blood from the genitals has been found in men.
If conception occurs, of course, all doubt is removed. If the sex cannot be definitely determined by such examination, it is best to consider the case one of male pseudo-hermaphroditism, which is the usual form, and to treat the individual as a male. 402
Menstruation, or the regular periodical discharge of blood from the uterus, is a phenomenon that occurs only in the human race and in some monkeys. The anatomical changes that accompany menstruation have not yet been definitely determined. In some species of monkey—Semnopithecus entellus and Macacus rhesus2—the following changes appear to take place at the menstrual periods: The endometrium first becomes swollen and congested as a result of the growth of the stroma, and increase in the number and size of the blood-vessels. The vessels in the superficial part of the stroma degenerate and break down, and blood is extravasated into the meshes of the stroma network. The extravasated blood collects into lacunæ which lie close beneath the uterine epithelium. Finally the lacunæ rupture and the blood escapes into the cavity of the uterus, forming the menstrual clot. Then a fresh epithelium grows over the torn surfaces, new blood-vessels are formed, the stroma shrinks, and the endometrium of the intermenstrual period is restored.
Nothing is known with any degree of certainty regarding the cause and significance of menstruation. There is much diversity of opinion in regard to the coincidence of ovulation and menstruation. Heape has shown that for monkeys ovulation and menstruation are not necessarily coincident; in forty-two menstruating specimens of S. entellus not one had a recently discharged follicle in either ovary. In monkeys, therefore, menstruation may take place without ovulation, and it is 403 probable that the same is true for the human female. Ovulation and conception may occur in the human female when menstruation is absent; pregnancy not infrequently occurs during the amenorrhea associated with lactation, and in India, where the girls are married at a very young age, pregnancy and child-birth occur before menstruation has begun.
Leopold (quoted by Hirst) in an examination of twenty-nine pairs of ovaries removed on successive days up to the thirty-fifth after a menstrual period, found a Graafian follicle bursting on the eighth, twelfth, fifteenth, sixteenth, eighteenth, twentieth, and thirty-fifth days after the menstrual period. Thus ovulation frequently occurred without menstruation during the intermenstrual interval. In five cases there was no ovulation at the menstrual period, or menstruation occurred without ovulation.
It seems probable, therefore, that the ripening of the ovum in the ovary is independent of the process of menstruation, though the increased blood-supply to the generative organs during menstruation may, to a certain extent, determine the time of ovulation when a sufficiently ripe ovum is present.
Though menstruation in women is analogous to the rut or “heat” of other animals, yet there are some points of difference: The lower mammals breed only at times of “heat,” and these times of “heat” occur in the wild state only at certain periods of the year, which are dependent upon climatic conditions, the young being born at the season of the year best suited for their survival. Some domestic animals, like the cow, probably as a result of domestication, have no regular breeding time. In the lower mammals “heat” and ovulation appear to be coincident, and these are the only periods during which the female seems normally to have any sexual desire.
The monkeys examined by Heape menstruated throughout the year and yet seemed in the free state to have definite breeding times. 404
The human female, with but few exceptions, menstruates throughout the year and may breed at any time. The exceptions in the case of the human female are of interest. Dr. Frederick A. Cook,3 ethnologist to the first Peary North Greenland Expedition, says of the Esquimaux living in the extreme north, from the seventy-sixth to the seventy-ninth parallels of latitude: “The passions of these people are periodical, and their courtship is usually carried on soon after the return of the sun; in fact, at this time they almost tremble from the intensity of their passions, and for several weeks most of their time is taken up in gratifying them. Naturally enough, then, the children are usually born at the beginning of the Arctic night.” In Queensland the natives are also said to have a special breeding season.
Menstruation usually begins in this country at the fourteenth year. The time of the first appearance of the process is influenced by race, climate, and environment. As a rule, it begins earlier in warm climates and later in cold climates. It is earlier in girls who lead luxurious, indolent lives than in girls of the working classes.
During the first year or two of menstrual life menstruation is often very irregular. It may be absent for several months after its first appearance, or recur at varying intervals before it becomes regularly established. Irregularity at this time calls for no treatment.
Precocious menstruation rarely occurs at a very early age. It has been known to begin, and to recur with regularity, from the time of birth. In such cases there is a corresponding premature development of the sexual organs.
The menstrual discharge consists of blood, mucous secretion from the uterus and vagina, and epithelial cells from the endometrium.
The normal duration of the flow is from two days to a week. The amount of fluid discharged is from 2 to 9 ounces. Menstruation occurs every twenty-eight days, 405 counting from the beginning of one period to the beginning of another. The menstrual interval is subject to considerable individual variations, which appear to be within the limits of health. It sometimes occurs with regularity every two, three, or five weeks. When it occurs every two weeks, the alternate flows are often but small in amount. The occurrence of, or the attempt at, menstruation every two weeks, in a woman who had previously menstruated monthly, is sometimes a symptom of beginning uterine disease.
Menstruation commonly ceases at about the forty-fifth year, when the menopause appears.
Most of the disorders of menstruation have already been considered as symptoms of the various lesions of the genital organs that have been described in the previous pages.
There are some disorders of menstruation, however, often unaccompanied by discoverable lesions, which now demand consideration.
Amenorrhea.—Amenorrhea is the absence of menstruation. Failure of the menstrual blood to be discharged from the vagina, such as occurs in cases of atresia, is not necessarily amenorrhea; menstruation may have taken place, though the most marked phenomenon of this process, the discharge of blood, is concealed.
The term primary amenorrhea, or emansio mensium, is applied to those cases in which menstruation has never appeared. Secondary amenorrhea, or suppressio mensium, is applied to those cases in which menstruation has ceased after having once been established.
Amenorrhea is due to defective development of the organs of generation; to premature atrophy, such as occurs in superinvolution of the uterus; to lesions, pathological and traumatic; to acute and chronic general diseases; and to psychical disturbances.
Menstruation is often absent during the acute diseases, such as typhoid fever, and it may remain suppressed until the general health is fully restored. 406
Amenorrhea may also occur in any chronic debilitating condition. It is common in chlorosis, anemia, phthisis, and malaria.
It frequently results from changes of climate and surroundings, and continues until the person becomes adapted to the new environment. It is seen in emigrants from other countries, and in women who move from the country to large cities. It is often caused by overwork, physical and mental, and by insufficient food. It is not uncommon in studious school-girls.
Amenorrhea is sometimes due to the excessive general development of fat, even in young woman who are apparently in good general health.
Amenorrhea is frequently associated with insanity. It may be caused by fright, grief, or anxiety. The fear of pregnancy after illicit coitus sometimes produces it.
In some unusual cases amenorrhea is present without any discoverable cause. The woman may be in perfect general health, and the sexual organs may be well developed, at least so far as can be determined by physical examination.
In amenorrhea there is often a general periodical disturbance that marks the times at which the menstrual bleeding should occur. There may be headache, flashes of heat, nervousness, nausea and vomiting, and a feeling of fulness and pain in the pelvis. Various cutaneous eruptions may occur as the result of amenorrhea, as in other diseases of the genital apparatus.
The poor health, mental and physical, that usually accompanies amenorrhea is often thought by the patient and her friends to be the result, rather than the cause—as it really is—of the arrested bleeding.
Treatment.—The treatment of amenorrhea depends upon the cause of the condition. Little, if any, benefit is to be expected in those cases due to defective development of the uterus or the ovaries. If an attempt at menstruation is made, as shown by periodical local pain and general disturbance, and the uterus is found to be small 407 and sharply anteflexed, benefit may sometimes result from thorough dilatation of the cervix.
Most cases of amenorrhea demand general treatment. The mode of life should be regulated according to strict hygienic principles. Fresh air, sunshine, baths, and suitable exercise should be prescribed. Studious girls should be made to lead more active lives. A change of surroundings is beneficial. A visit to the seashore and salt-water baths are of advantage.
The general health should be improved by the administration of iron, strychnine, or some other tonic. Blaud’s pill and the hypophosphites are useful. Obesity should be relieved by a regulated diet and exercise. The regularity of the bowels should always be carefully attended to. Most of the so-called emmenagogues are of but little, if any, value. Benefit is sometimes derived from the use of potassium permanganate (gr. j-ij three times a day) and the binoxide of manganese (gr. j-ij three times a day). These medicines should be administered in pill form for several weeks.
Oxalic acid in doses of from ⅒ to ¼ of a grain, given in lemon syrup for a period of from one to four months, has been recommended, and is sometimes very useful.
It seems probable that pelvic massage practised for a period of several months may result in benefit.
Acute suppression of menstruation during a menstrual period is a phenomenon to which the term amenorrhea is not properly applicable. It may be caused by exposure to cold or by some sudden emotional disturbance during the menstrual flow.
The condition may be unaccompanied by any subjective symptoms, or there may be present ovarian and pelvic pain.
The treatment consists in rest in bed, the application of warm fomentations to the lower abdomen, and hot foot-baths. Especial care of the general health should be observed at the following menstrual period.
Scanty Menstruation.—Scanty menstruation occurs 408 when the menstrual flow is much less than normal. It must be remembered that individual peculiarities in this respect may be within the limits of health. When one or more periods are missed, and the flow shows a continual tendency to diminish in amount, treatment may be demanded.
The causes and the treatment of scanty menstruation are those which have already been considered under Amenorrhea.
Vicarious Menstruation.—Vicarious menstruation is the discharge of blood, at the menstrual periods, from some part of the body other than the uterus. In some cases, instead of a discharge of blood, a secretion of another character takes place.
The vicarious discharge may be the only phenomenon present, or it may occur supplementary to the normal uterine bleeding.
The vicarious bleeding may take place from almost any part of the mucous or cutaneous structures. It occurs from the nose, the throat, the lungs, the stomach, the bladder, and the anus. It may occur from an ulcer or other lesion of the external surface. Sometimes the cutaneous hemorrhages appear in the form of ecchymoses.
Various secretions may take the place of the bleeding. A monthly flow of milk from the breasts has been observed, and a periodical diarrhea or leucorrhea has taken place.
Vicarious menstruation is a rare condition. It may occur in defective development of the uterus and ovaries. It is usually found in debilitated nervous women, and accompanies a deficient menstrual discharge from the uterus.
Treatment.—Direct local treatment should be applied to the vicarious bleeding only when it becomes excessive. The general health of the woman should receive attention. Treatment should be applied to any local lesion of the genital apparatus that may be discovered. The directions given for amenorrhea are also applicable here. 409
The menopause is the final cessation of menstruation. The age at which it occurs is dependent upon a great variety of conditions—nationality, climate, mode of life, constitutional and local diseases. In the northern countries of Europe the menopause is said to appear later than in the southern; in England, later than in America. It has been observed that country women menstruate to a later age than city women. The woman who bears a number of children in rapid succession and suckles them not infrequently has a premature menopause. The menopause may appear early in very fat women and in women who are the victims of tuberculosis, nephritis, and diabetes. Disease of the uterus, tubes, and ovaries may retard the menopause. In fibroid tumor of the uterus the menopause may be delayed for several years.
In this country the menopause occurs between the fortieth and fiftieth years—usually about the age of forty-five.
The menstrual bleeding may gradually diminish in amount until it disappears; or it may stop abruptly and permanently; or there may occur one or more intervals of amenorrhea of one, two, or three months’ duration, followed by normal menstrual bleedings, perhaps of diminished amount, before the flow finally ceases.
Profuse bleeding at the time of the menopause and slight bleeding occurring more often than monthly are, unfortunately, viewed by most women as of no moment, and as part of the normal phenomena of the change through which they are passing. The same 410 may be said of the apparent reappearance of menstruation, or of slight irregular hemorrhages occurring after the menopause had been established and menstruation had been absent perhaps for many months. These phenomena are not normal. They should always excite the alarm of the woman, and they demand immediate examination on the part of her physician. As a rule, the bleeding is caused by some pathological condition of the uterus—fungous growths, polypi, fibroids, or cancer. The benign lesions may disappear spontaneously with the progressing atrophy of the womb, and the hemorrhages may cease. Many women undoubtedly recover without treatment, and are thus confirmed in the belief that such irregular hemorrhages are a normal part of the menopause; and the unfortunate women with cancer are thus encouraged to delay seeking medical advice until the disease has progressed too far for cure.
The normal changes of the genital organs that begin at the menopause are those of atrophy slowly progressing to the senile condition. The ovaries atrophy; the epithelial elements gradually give place to connective tissue; the Graafian follicles and corpora lutea are destroyed; the tunica albuginea becomes thick and shriveled. The uterus diminishes in size; the vaginal cervix may disappear; the utricular glands diminish in size and number; the endometrium atrophies. The Fallopian tubes shrink and become shortened, and the fimbriæ disappear. Similar atrophic changes affect the vagina, the external genitals, and the mammary glands.
If the woman is in good general health, and has no disease of the uterus, the tubes, or the ovaries, the menopause may become established without any marked general disturbance.
In many cases, however, very annoying general symptoms appear, and last for one or two years before the woman becomes adapted to the altered conditions.
There may be headache, flushes of heat, nervous depression, derangement of the digestive apparatus, and 411 other functional disturbance. The woman often becomes very fat at this period. The nervous derangement may be so severe as to result in insanity.
The vaso-motor disturbances are often the most annoying. The phenomena of the “flushes” consist of a feeling of heat over the whole or a part of the body, followed by sweating and the sensation of cold or a slight chill. The flushes may occur frequently during the day, sometimes several times during an hour.
The treatment of the menopause should be directed to the maintenance of the general bodily and mental health. The diet should be carefully regulated. Too much nutritious food should be forbidden. Purgatives should be administered whenever necessary. The woman should have plenty of fresh air and the proper amount of exercise. Mental depression demands a change of locality and surroundings. 412
Fistulous openings may exist between the different portions of the genital tract and the neighboring structures. Such fistulæ are the result of childbirth, operative or other form of traumatism, congenital defect, cancer, syphilis, or suppuration. The accompanying diagram (Fig. 180) shows the chief varieties of fistula that occur.
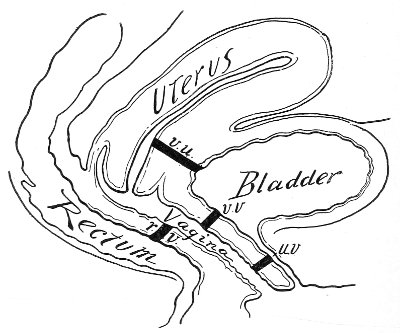
Fig. 180.--Diagram illustrating the chief varieties of genital fistula: v. u., vesico-uterine fistula; v. v., vesico-vaginal fistula; u. v., urethro-vaginal fistula; r. v., recto-vaginal fistula.
Vesico-vaginal Fistula.—The most frequent form of fistulous opening occurs in the septum between the bladder and the vagina. The condition is usually caused by sloughing, the result of prolonged pressure from the fetal head at labor. 413
In some cases such an opening is made for therapeutic reasons by the physician, for the cure of cystitis.
Intelligent midwifery and the prompt and proper use of the obstetrical forceps have greatly diminished the frequency of vesico-vaginal fistula. It was formerly a very common disease. At the present day it is but rarely seen, at least in those parts of the country where women have competent attendance at labor.
The vesico-vaginal opening may be situated at any portion of the septum. It varies very much in size and shape. It may be a small hole barely admitting a fine probe-point, a median slit, or a large irregular opening involving the whole base of the bladder.
The appearance of the fistula varies according to the time that has elapsed since the receipt of the injury. The margins of the opening, which are at first irregular and ulcerated, become in time thin and firm from cicatricial contraction, and the size of the opening becomes similarly diminished.
The first symptom of vesico-vaginal fistula is the involuntary escape of urine from the vagina. If the condition has resulted from pressure at parturition, the incontinence of urine does not appear for five or ten days after labor, when the slough has separated. When a direct laceration of the vesico-vaginal septum has occurred, the urine will escape immediately.
The degree of incontinence varies with the size and the position of the fistula. If the opening is small and is situated in the upper part of the vagina, there may be perfect continence when the woman is in the erect position, as long as the urine remains below the level of the opening. Incontinence returns when the accumulation of urine becomes greater than this and when the woman assumes the recumbent posture. I have seen a woman with a fistula of this kind who was only troubled with incontinence at night.
The secondary symptoms of vesico-vaginal fistula are due to the irritation of the urine. Unless the greatest 414 cleanliness be observed, great suffering may result within a few weeks after the receipt of the injury. The vagina, the labia, and the inner aspects of the thighs become inflamed and excoriated. The mucous membrane of the vagina may become covered with an offensive phosphatic deposit. If the fistulous opening be large, the fundus of the bladder may prolapse into the vagina and become covered with a similar deposit.
Secondary kidney disease, from infection of the ureters, may follow in time.
As the result of disuse the bladder becomes contracted, and its walls become thickened from inflammatory infiltration, so that when the fistula is closed the capacity of the bladder is much less than normal. Disuse of the urethra results also in contraction, which may be so extensive as seriously to complicate treatment.
Physical examination usually reveals the condition. The woman should be placed in the Sims, the genu-pectoral, or the lithotomy position, and the anterior vaginal wall should be examined through the Sims speculum. The examiner should, of course, determine that the involuntary flow of urine comes from the vagina, and not from the urethra. Women are often unable to tell accurately whence the urine escapes, and the single symptom of incontinence of urine is not pathognomonic of fistula.
In most cases the fistulous opening may be readily detected, and a sound passed through the urethra may be made to emerge in the vagina. In the case of small openings, however, obscurely situated in the upper part of the vagina, and especially in case of vesico-uterine fistula, it may be difficult to demonstrate the presence of a fistula. In such cases the bladder may be filled with sterile milk, which may then be seen escaping into the vagina. This is a valuable method of diagnosis in the rare cases of uretero-vaginal fistula.
Treatment.—The method of curing vesico-vaginal fistula was taught to the world by Marion Sims, who operated 415 successfully in 1849, and who published his first article upon the subject in 1852.
Careful preparatory treatment before operation is usually necessary. Unless the vagina and the bladder are in a healthy condition beforehand, every method of operation is likely to fail.
It is necessary to treat all excoriations or ulcerations, to cure the cystitis, and to relieve the tension of all bands of scar-tissue in the vagina that may prevent proper approximation of the edges of the opening.
The phosphatic deposit should be carefully removed from the vaginal walls and the interior of the bladder with a soft sponge or cotton, and a weak solution of nitrate of silver (gr. v to ℥j) should be applied to the raw surfaces.
Frequent warm sitz-baths should be administered daily. The vagina should be washed out several times a day with large quantities of sterile hot water or with a solution of boracic acid (ʒj to the pint).
The urine, which is generally alkaline, should be rendered acid by the use of benzoic or boracic acid.
Emmet advises the following prescription: “2 drams of benzoic acid and 3 drams of borax to 12 ounces of water, of which a tablespoonful, further diluted, should be given three or four times a day.” After the urine has become acid the dose may be reduced.
Every fifth day the solution of nitrate of silver should be applied to the unhealed, excoriated surfaces. It may be necessary to pursue this treatment several weeks before the parts are brought to a healthy condition. Improvement is perceived not only in the condition of the vaginal walls and the bladder, but in the edges of the fistula, which, in place of being hypertrophied and indurated, assume a natural color and density.
In case the vaginal fistula be small, the accompanying cystitis may be difficult to cure, because there is always some residual urine in the bladder. It may then be advisable, as a preparatory step, to enlarge the fistulous 416 opening by a clean incision in the median line, in order to secure more perfect drainage. The cystitis may be kept up by the presence of a phosphatic concretion in the bladder, which may be removed in this way. It is useless to close the fistula until the cystitis is cured.
In every case of vesico-vaginal fistula it is advisable to examine for vesical calculus, that the bladder may not be closed with a calculus in it. The calculus occasionally exists before the formation of the fistula, and perhaps assists in its production, the vesico-vaginal septum being squeezed between the child’s head and the calculus. Usually, however, the calculus forms as a result of the fistula.
When the parts have been brought to a healthy condition the fistula should be examined with a view to the method of closure. The opening should be exposed with the Sims speculum, and the edges at opposite points should be seized with tenacula or forceps and approximated. In this way the surgeon may determine the direction in which the fistula may be closed with the least traction on the sutures. When possible, it is advisable, in order to prevent shortening of the vagina, to close the fistula in the direction of the long axis of the vagina.
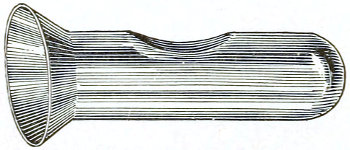
Fig. 181.—Sims’ vaginal dilator.
If the edges of the opening cannot readily be brought together, any restraining bands of tissue in the vaginal walls should be divided with scissors. If these bands are slight and superficial, they may be divided at the time of operation for closure. If, however, they are extensive, preparatory treatment devoted to the liberation of the edges of the fistula must be practised. All restraining bands should be freely divided, and after the vagina has thus been opened up, it should be distended (to prevent subsequent contraction) by introducing a vaginal plug or dilator (Fig. 181) or a rubber bag packed with sponges. Bleeding is generally controlled by the pressure of the 417 plug. The vaginal plugs of glass or of hard rubber are made of various sizes. They should be long enough and thick enough to stretch the vagina without producing sloughing. The plug is retained by a T-bandage.
After this operation the woman should be kept in bed for a week or ten days. The urine should be drawn with the catheter without removing the plug. When suppuration begins the plug will become loosened and may be removed. Emmet says: “It is remarkable how much absorption of the cicatricial tissue takes place in a few weeks when judicious pressure has been maintained by this instrument.”
After removing the plug, vaginal douches should be resumed until healing is complete.
It will be seen from this consideration that the preparatory treatment may be severe and may extend over a long period. Such extensive treatment is not by any means always necessary; when, however, it is required, it is useless to proceed to operation without it.
Operation.—The operation consists in freshening the edges of the fistula with the knife or scissors and bringing them into apposition with the interrupted suture. Different forms of suture have been used by various operators. If the parts are in a healthy condition and are properly denuded and approximated, it makes no difference in the result what form of suture is used. As in all forms of plastic work, I prefer silkworm gut shotted. The operation is most easily performed with the woman in the Sims position, the vagina being exposed with the Sims speculum. The lithotomy or the genu-pectoral position is preferred by some operators. The edge of the opening should be seized with the tenaculum or with tissue-forceps, and a continuous strip of tissue should be removed all around the fistula, extending from the mucous membrane of the bladder out upon the vaginal surface for a quarter or three-eighths of an inch. The vaginal mucous membrane usually retracts somewhat as soon as it is liberated from the fistulous margin, so that the 418 raw surface is broader than the strip removed. It is advisable to avoid any injury to the mucous membrane of the bladder, as free bleeding may take place from this structure. The denuded surface should extend as near as possible to the mucous membrane of the bladder without involving it.
The denudation should be extended some distance beyond each angle of the fistula, in order to secure perfect apposition in these positions.
The length and shape of the needle used for closing the opening varies with the fancy of the operator. As a rule, a small needle, straight or curved at the point, is most convenient (Fig. 182).

Fig. 182.—Fistula-needles.
The needle should be introduced about an eighth of an inch from the edge of the vaginal mucous membrane, and should be made to emerge at the edge of the mucous membrane of the bladder. It should be reintroduced and emerge in the reverse order on the opposite side (Fig. 183). The sutures should be placed about a quarter of an inch apart.
After the sutures have been introduced, and before they have been shotted or tied, the bladder should be thoroughly washed out with a warm boric-acid solution. The operator should make sure that no blood-clot is left in the bladder. After the sutures have been shotted a light gauze tampon may be placed in the vagina. A permanent soft-rubber catheter may be introduced through the urethra, or the urine may be drawn every three or four hours after the operation. If care is given to the cleanliness of the catheter, it is perhaps best to retain it in the bladder for three or four days, after which the urine may be drawn every four hours. The catheter should be removed twice in twenty-four hours for purposes of cleansing. The eye of the catheter frequently becomes obstructed by blood-clot.
It should not be forgotten that the bladder is often much contracted in old cases of vesico-vaginal fistula, 419 and as the capacity is diminished more frequent catheterization than usual is necessary.
Boric or benzoic acid should be continued during the convalescence.
The gauze tampon should be removed on the second day.
The bowels should be moved on the second or third day. The sutures may remain for two weeks. The woman may sit up at the end of two weeks.
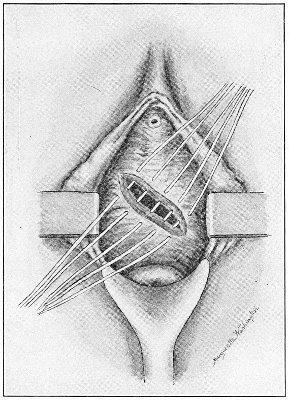
Fig. 183.—Vesico-vaginal fistula with the sutures introduced.
The operation described here—more or less modified in order to meet the requirements of different cases—will result in cure in the great majority of instances. Often much depends upon the ingenuity and the mechanical skill of the operator. Sometimes two or three operations are necessary before the opening can be completely closed, the operator closing part at each sitting.
In the case of a small fistulous opening it may be necessary to enlarge it by free incision before the denudation and the introduction of the sutures can be properly accomplished. 420
In the very rare cases which are incurable by operation kolpokleisis, or closure of the vagina, has been practised by some. The operation was performed by removing a circular strip around the circumference of the vagina, immediately above the ostium vaginæ, and approximating the raw surfaces by a transverse row of sutures. This operation makes of the bladder and the vagina one urinary pouch into which menstrual blood and uterine discharges flow. It should never be practised. I quote from Emmet in this connection: “From my own observation I have learned that it is but a question of a few months, a year, or possibly two years, before serious consequences must arise after leaving a receptacle, like a portion of the vagina, in which the urine may stagnate. To give a retentive power for so short a time is not a sufficient compensation for the suffering and consequences that supervene. As the result of my experience, I would urge that the operation never be resorted to under any circumstances. The maximum has now been reduced to 2 or 3 per cent. of cases where the resources of the surgeon cannot overcome all the difficulties that may be presented in closing a vesico-vaginal fistula.”
The forms of operation in which the cervix uteri is utilized to assist in the closure of a vesical fistula, as a result of which the menstrual blood and the uterine secretions are discharged into the bladder, are contraindicated for similar reasons.
Urethro-vaginal fistula is much less common than vesical fistula. Unless the neck of the bladder be involved, there may be perfect control of urine; though, of course, when the urine is voided it will escape from the ostium vaginæ, and not from the external meatus.
The treatment of urethro-vaginal fistula is essentially the same as that already described for vesico-vaginal fistula. The edges should be denuded, and the opening into the urethra closed over a large-sized catheter. The line of union should be in the long axis of the urethra.
Vesico-uterine Fistula.—In this form of fistula the opening usually extends from the bladder into the cervical 421 canal. It is caused by labor in which the anterior lip of the cervix is lacerated. The lower portion of the cervical laceration may unite, leaving the fistulous opening above.
The diagnosis of the condition is made from observing urine escape from the cervical canal, or by injecting the bladder with milk or other colored fluid. A sound introduced in the cervix may be brought in contact with a probe passed through the urethra and bladder into the fistula.
If these methods of examination are not satisfactory, endoscopic examination of the interior of the bladder will reveal the abnormal opening.
The treatment consists in dividing the anterior lip of the cervix and the vaginal wall down to the fistulous tract; thorough denudation of the walls of the fistula; and closure of the whole incision by interrupted sutures.
Uretero-vaginal Fistula.—This condition is usually the result of injury to the ureter by operation. It may occur from the destruction of tissue caused by pelvic abscess, which discharges through the vaginal vault. In extensive vesico-vaginal fistula caused by sloughing after labor the bladder-wall may become rolled out so that the ureter opens into the vagina.
If but one ureter is involved, one-half of the urine will be discharged in the natural way and the other half by the vagina.
The treatment consists in directing the ureter into the bladder by plastic operation performed through the vagina; or by performing celiotomy, dissecting out the ureter, and implanting it in the fundus of the bladder.
Recto-vaginal Fistula.—Recto-vaginal fistula is usually caused by parturition. The destruction of tissue is sometimes due to syphilis. In the latter case cure is difficult, and sometimes impossible.
The symptom of the condition is the passage of feces and flatus into the vagina.
Sometimes but a very small opening exists, situated immediately above the sphincter muscle; in other cases the greater portion of the recto-vaginal septum is destroyed. 422
The condition may be recognized by placing the woman in the lithotomy position and exposing the posterior vaginal wall by the Sims speculum placed under the pubic arch.
The treatment consists in operation similar to that described under the consideration of vesico-vaginal fistula. The woman should be prepared as for a plastic operation upon the perineum. The rectum should be thoroughly emptied before operating. The sphincter ani should be stretched. It is always advisable, when possible, to close the opening from the vagina.
The mucous membrane of the rectum should be injured as little as possible, in order to limit the bleeding. It may be necessary to relieve tension on the edges of the fistula by making, on each side of the vaginal aspect of the opening, an incision parallel to the long axis of the vagina.
In case of a small fistula situated immediately above the sphincter ani, it is sometimes difficult to denude and to introduce the sutures. It then becomes necessary to divide the perineum and the sphincter ani to the fistula, denude the edges, and to introduce sutures as in a case of complete median laceration of the perineum. Sometimes the recto-vaginal fistula is much larger on the vaginal than on the rectal aspect—is, in fact, funnel-shaped, the destruction of tissue having been greater upon the vaginal surface. If in such a case the edges of the fistula cannot be brought into apposition after freeing all restraining bands, it may be necessary to split the edge of the opening, so that the rectal wall is freed and may be brought together by sutures introduced through the rectum, leaving the vaginal opening to be filled by granulation. The rectal sutures may be introduced by placing the woman in the Sims position and exposing the anterior rectal wall with the Sims speculum.
The after-treatment resembles in all respects that prescribed after operation for laceration through the sphincter ani. The sutures should be removed in two weeks. 423
Before considering in detail the diseases of the urethra and bladder, it will be necessary to describe the modern methods of examining these structures.
The examination of the urethra and bladder has been very much facilitated by the methods and instruments that have been popularized in this country by Kelly. The following apparatus is required: a female catheter; a urethral calibrator; a series of specula with obturators; a head-mirror and light or an electric headlight; long, delicate toothed forceps (Fig. 184); an inclined plane or several hard pillows for elevating the pelvis; small balls of absorbent cotton about the size of a pea, or strips of absorbent gauze cut 1 inch in width and about 10 inches long, for drying out the bladder.
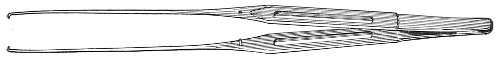
Fig. 184.—Mouse-tooth forceps for bladder.
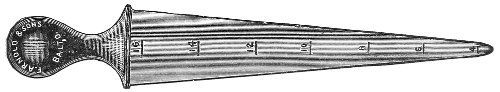
Fig. 185.—Urethral dilator: short lines indicate diameter in millimeters.
The urethral calibrator or dilator (Fig. 185) is a conical metal instrument with a maximum diameter of twenty millimeters. The diameters in millimeters of the various portions are indicated by numbers upon the instrument. 424
The urethral calibrator is useful for dilating the external meatus to a degree sufficient to admit the necessary speculum. The external meatus is, as a rule, the only portion of the urethra that requires dilatation. Any instrument that will pass through the meatus will pass through the rest of the canal.
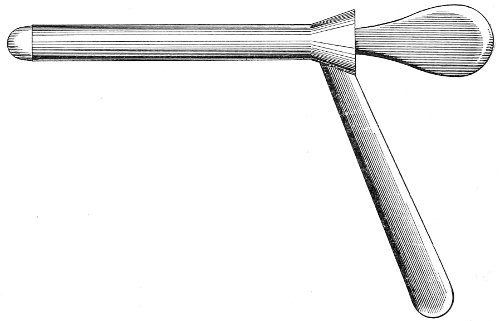
Fig. 186.—Kelly’s cystoscope or vesical speculum.
The speculum (Fig. 186) is a cylindrical metal tube fitted with a handle on which is the number indicating the size of the instrument. There are a number of specula, varying in diameter from 5 to 20 millimeters. Each speculum is fitted with an obturator. The most useful specula are those ranging from 8 to 12 millimeters in diameter. The urethra may readily be dilated up to 12 millimeters, with little if any, external laceration. Dilatation sufficient to admit the largest instrument (20 millimeters) is always accompanied by considerable laceration of the urethral opening. Dilatation of the urethra should never be practised beyond this degree, on account of the danger of subsequent incontinence of urine.
An anesthetic is usually required for the examination, unless the woman be capable of enduring considerable pain, or has become accustomed to the procedure from 425 previous experience. Local anesthesia of the urethra with cocaine (gr. x to ℥j) is often sufficient.
The woman is placed on the table in the lithotomy position, and the bladder is emptied with the catheter. The external meatus is then dilated to the requisite size by inserting the graduated calibrator with a general rotary movement. When the meatus has been stretched sufficiently, as indicated by the number on the calibrator (usually about 12 millimeters), the instrument is withdrawn, and the speculum of corresponding number, armed with the obturator, is introduced; the obturator is then removed.
The hips of the woman are now elevated on the pillows or the inclined plane, or the foot of the table is raised, so that the hips shall be from 10 to 20 inches above the level of the shoulders.
The examiner, armed with the head-mirror or light, is then prepared to inspect the interior of the bladder. If the mirror is used, the light (Argand burner or electric drop-light) should be held close to the pubis of the patient.
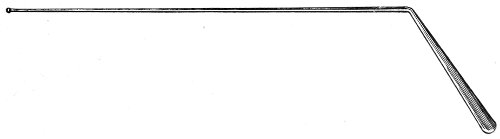
Fig. 187.—Vesical probe or applicator.
Usually a small quantity of urine remains in the bladder after catheterization, or is secreted during the preliminary procedures, and it is necessary to remove this before complete examination of the bladder can be made. This may be done by means of the small balls of absorbent cotton or the strips of gauze grasped with the long-toothed forceps and passed in through the speculum; or some form of suction apparatus may be employed, consisting of a rubber exhaust bulb and a long metal tube perforated at the distal end by small openings. 426
The elevated position of the hips is an essential part of this method of examination; it permits the intestines to gravitate out of the pelvis, and, as soon as the urethra is opened, the bladder becomes distended with air, so that all of its interior may be readily inspected, and applications to the surface may be directly made through the speculum. In some cases it is difficult to produce the requisite distention of the bladder by elevating the hips. This difficulty may arise in the case of very fat women. It then becomes necessary to place the patient in the knee-chest position, when the requisite distention is readily accomplished.
As the speculum is withdrawn from the bladder the internal meatus and the urethral walls may be examined as they fall together beyond the distal end of the instrument.
The female urethra is a musculo-membranous canal averaging 1¾ inches in length, and, when not stretched, about ¼ inch in diameter. The urethra is normally closed by the apposition of its walls. In the neighborhood of the external meatus it is an antero-posterior slit. In the neighborhood of the internal meatus it is a transverse slit. In the middle portion the mucous membrane is arranged in longitudinal folds, and a transverse section shows a stellate closure.
The muscular coat of the urethra contains both striped and unstriped muscular fibers.
The mucous glands of the urethra are most numerous in the region of the external meatus. Skene first described two glands that are worthy of special mention. Skene’s glands are two tubules, large enough to admit a No. 1 probe of the French scale, that lie upon the floor of the urethra immediately within the external meatus. They lie parallel to the long axis of the urethra, and in length vary from ⅜ to ¾ of an inch. They are placed beneath the mucous membrane, in the muscular coat. The orifices of the glands are on the free surface of the mucosa, immediately within the external meatus. In 427 young women the orifices are found about ⅛ of an inch above the plane of the external meatus. If the external meatus be patulous, or if there be any prolapse or inflammation of the mucous membrane of the urethra, the orifices of Skene’s glands may be seen upon each side of the urethral orifice as soon as the labia are separated. In gonorrhea their position is often indicated by a small drop of pus exuding from the orifices. The upper ends of the glands may terminate in a number of divisions.
Urethritis.—Urethritis is much less frequent in women than in men. In the great majority of cases it is caused by gonorrhea. Aside from microscopic examination, urethritis, acute or chronic, may be considered one of the strongest evidences of gonorrheal infection that we have.
Urethritis is also rarely caused by the exanthematous diseases, irritation of concentrated urine, vaginal discharges, chemical irritants, and traumatism.
Symptoms.—The symptoms of urethritis in the acute stage of the disease are frequent and painful urination. Burning and scalding sensations are experienced along the course of the urethra during urination. Occasionally a few drops of blood escape during or after urination. As the disease progresses toward cure or passes into the chronic stage, the intensity of these symptoms diminishes, and finally they disappear.
Examination of the parts shows that the external meatus is red and swollen. The swollen mucous membrane may bulge through the opening, giving the appearance of prolapse. The orifices of Skene’s glands may be conspicuous. If the woman have not recently urinated, a drop of pus may appear at the meatus, or it may be brought into view by vaginal pressure along the course of the urethra. Pressure upon the urethra through the vagina causes pain. This is one of the best tests of inflammation of this structure. The urethra may feel hypertrophied, indurated, or cord-like to the touch. The urethral discharge should always be examined microscopically for the gonococci.
In chronic urethritis the subjective symptoms are usually 428 absent—except, perhaps, frequency of urination. The diagnosis is made by physical examination. If the woman has not urinated for several hours, the examiner will be able to express, by vaginal pressure along the course of the urethra, a drop of muco-purulent fluid resembling the gleety discharge of the male.
The endoscope reveals the presence of congestion and inflammation of the mucous membrane.
Treatment.—In the acute or the painful stage of the disease no local applications should be made. The external genitals should be bathed several times a day with hot water, preferably by means of sitz-baths. Vaginal douches are not indicated unless the vagina be involved in the inflammation. The vaginal syringe may be the means of carrying infection higher up in the genital tract. Rest in the recumbent position, if possible, is desirable. The diet should be non-stimulating, and large quantities of diluent drinks, such as flaxseed tea, should be prescribed. The bowels should be kept loose by saline purgatives.
In the subacute or the chronic stages of the disease boracic acid (gr. x-xx three or four times a day), salol, oil of sandal-wood, cubebs, copaiba, and other drugs used for the similar condition in the male are indicated. After painful micturition has ceased, the physician may make local applications to the urethra, in case the inflammation does not subside satisfactorily without them. Such local applications are not always necessary, and they may do harm unless proper care is exercised in their administration. Asepsis and gentleness are necessary, and the applications should never be too strong or irritating.
Frequent douching of the urethra (two or three times a day if possible) with sterile hot water is often of much benefit. Skene’s reflux catheter should be used (Fig. 188). The shaft of this instrument is fluted or grooved to permit the return of the fluid. The catheter should be introduced as far as the internal meatus; a fountain syringe should be attached to it, and the urethra should be washed out with a quart of hot water. 429
After the irrigation the catheter should be withdrawn and a urethral injection of nitrate of silver (gr. j or ij to ℥j) should be administered. The injection may be given by means of a glass pipette the nozzle of which is large enough to encircle the external meatus. The nozzle should be placed over, not in, the meatus. The female urethra will hold about 15 minims of fluid; more than this should not be injected. As the condition improves the frequency of these treatments may be diminished.

Fig. 188.—Skene’s reflux catheter.
If the condition does not yield to such treatment within a few weeks, application should be made directly to the mucous membrane of the urethra through the endoscope. The urethral canal should be washed out as just described, and the endoscope should be introduced as far as the internal meatus. As it is slowly withdrawn the application should be made over the whole inner surface of the urethra by a fine applicator wrapped with cotton. Nitrate of silver (gr. v-x to ℥j) should be employed.
Sometimes it is found that the suppuration persists in Skene’s glands. A small drop of pus may be found exuding from the orifice of the gland after the rest of the urethra has been restored to a healthy condition. In such a case the gland should be split up on the urethral surface by introducing into it one blade of a fine scissors, and the tract should be carefully wiped out with pure carbolic acid or a strong solution of nitrate of silver.
In every case of urethritis of gonorrheal origin it is of the greatest importance that every trace of the disease should be eradicated before the patient gives up treatment. There is always danger of infection extending to the upper parts of the genital tract. 430
Stricture of the Urethra.—Stricture of the urethra in the woman, unlike the similar condition in the male, is very rare. It is caused by gonorrhea, injury at childbirth or other traumatism, and caustic applications. The stricture may exist at any part of the urethral canal. The form most usually seen is that which occurs at the external meatus, and is caused by the removal of abnormal growths with caustic or with the knife.
The symptoms of urethral stricture in women are much less marked than those in men. There is frequent and difficult urination. Occasionally there is incontinence or partial retention of urine.
If the stricture exist at the external meatus, it may be readily seen and its dimensions determined. If it exist in the upper portion of the urethral canal, it may sometimes be felt by palpation along the course of the urethra through the vagina, the position of the stricture being indicated by local thickening and induration. Its location may also be determined, as in man, by the use of the bulbous bougie or sound.
Treatment.—When the stricture is situated at the external meatus, it may be divided with the knife or forcibly stretched. When it is situated in the upper portion of the urethra, it is best treated by forcible dilatation.

Fig. 189.—Female urethral sound.
The small uterine dilator is the most convenient instrument to use. The dilatation should not extend beyond half an inch, for fear of injuring the urethral walls or producing incontinence. In order to prevent contraction, it is advisable to pass the large urethral sound (10 millimeters) at intervals of one or two days after this operation, until the patency of the urethra is ensured.
In some cases the continual subsequent use of the sound 431 is necessary, as in stricture in the male. The woman may be readily taught the use of the instrument herself.
Prolapse of the Mucous Membrane of the Urethra.—Prolapse of the urethral mucous membrane is of unusual occurrence. Prolapse may be limited to part of the circumference of the meatus, or it may extend around the whole canal. The condition is usually found in weak, debilitated women. It may occur during childhood.
The prolapse may be caused by dilatation of the urethra and the external meatus or by the traction of a neoplasm of the urethra. It sometimes occurs after labor. It may be produced by continual vesical tenesmus, the result of cystitis, calculus, or a tumor of the bladder.
The symptoms, vesical tenesmus and dysuria, are usually present. Sometimes incontinence of urine occurs. The protruding mucous membrane may become irritated and inflamed, and cause much local pain. It has been known to slough off.
Treatment.—The treatment should be directed, in the first place, to the relief of any causative condition, such as cystitis or calculus.
Inflammation of the protruding mucous membrane should be relieved by local applications of hot water and by rest in bed. The mucous membrane should then be gently replaced within the urethra, and contraction of the canal should be promoted by the use of astringent injections of tannic acid or alum.
If the disease does not yield to this treatment, the prolapsed mucous membrane should be excised, and the edges of the mucosa should be stitched to the margin of the meatus by fine suture.
After this operation there is sometimes cicatricial contraction of the external meatus, which may readily be cured by forcible dilatation.
Vesico-urethral Fissure.—Vesico-urethral fissure is an ulcerated crack of the mucous membrane situated at the internal urinary meatus. The upper portion extends into the bladder, the lower portion is in the urethra. 432 Skene describes it as “from ¼ to ⅜ of an inch in length, and from 1/12 to ⅙ of an inch in width at the center, but tapering off at each end. The deepest part has a yellowish-gray color, like that of an indolent ulcer, while the edges are red and actually inflamed, like those of an irritable ulcer.”
Vesico-urethral fissure is usually caused by urethritis. It may also result from injuries during confinement or from the bungling use of the catheter.
Symptoms.—There is a constant desire to urinate, and urination is followed by severe tenesmus. There is a burning pain at the neck of the bladder, increased immediately after urination. Pressure upon the internal meatus through the vagina may cause lancinating pain.
The symptoms resemble closely those of urethritis and cystitis.
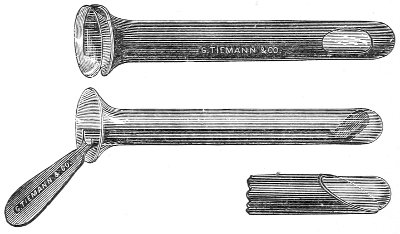
Fig. 190.—Skene’s urethral endoscope.
The diagnosis of vesico-urethral fissure can be made with certainty only by seeing the fissure through the endoscope. The existence of the condition may be suspected in a woman who presents the symptoms just described, and in whom no signs of inflammation or other disease of the urethra or the bladder can be detected.
The open endoscope is not satisfactory for detecting this condition, because the fissure is hidden from view by the folds of mucous membrane at the upper end of the instrument. Skene, who has especially directed attention to vesico-urethral fissure, states that he never was 433 able to detect the lesion until he used the form of endoscope introduced by him (Fig. 190), which consists of a small glass tube like the ordinary test-tube, into which is passed a mirror on a holder. The instrument is passed into the urethra, and light is thrown in by means of the concave head-mirror. By moving the small mirror in the tube, different parts of the urethral walls may be examined. The instrument opens out the folds of mucous membrane immediately above the fissure and renders it visible.
Treatment.—The cure of vesico-urethral fissure is often difficult. The lesion is exposed to continuous irritation from the urine and from the sphincteric action of the muscular fibers at the vesical neck—an action which is much increased by the tenesmus present. This constant muscular action impedes healing, as in the case of fissure of the anus. The internal urinary meatus should be dilated under anesthesia to the extent of ½ inch by means of the graduated bougies or the uterine dilator. After dilatation the woman should be kept in bed and the urine should be rendered as unirritating as possible by the use of diluent drinks and boracic acid.
If this treatment does not result in cure, a vesico-vaginal fistula should be made, so that, by carrying off the urine by this means, rest from functional activity will be furnished to the region of the vesical neck.
No effort need be made to keep the fistula open, as by the time it has closed spontaneously the fissure will have healed.
Dilatation of the Urethra.—Dilatation of the urethra producing symptoms that require treatment is unusual. It may be due to congenital defect, to spontaneous expulsion, or instrumental extraction of a calculus or tumor of the bladder, to excessive dilatation by the surgeon; and it may occasionally follow pregnancy. Skene says, “the hyperemia of the urethra which occurs in pregnancy and which tends to produce overdistention of the veins favors dilatation of the whole urethra.” 434
The urethra may be so dilatable that it will admit the penis—coitus having been practised in this way in a number of instances.
In dilatation of the urethra there may be continuous incontinence of urine, or the urine may escape only during acts of straining, coughing, or lifting.
The condition may be determined by the insertion of sounds or the finger.
Treatment should be directed to the cure of any inflamed condition of the urethra which may accompany dilatation, and to the use of astringent injections of tannic acid.
If incontinence of urine persists it may be necessary to perform a plastic operation, excising a portion of the anterior wall of the vagina and the posterior wall of the urethra, and closing the wound by transverse sutures.
In urethrocele the dilatation is confined to a portion of the urethra, usually the middle third. There is a sacculated condition of the posterior wall of the urethra extending into the vagina. The usual cause of this condition is traumatism during labor. The symptoms are painful and difficult micturition and partial incontinence of urine. The condition may be diagnosed by the use of the sound or the probe, which may be inserted in the sac through the urethra, when the point may be felt by a finger on the anterior vaginal wall. Sometimes the urethrocele produces a distinct bulging in the anterior wall of the vagina.
If the annoying symptoms of urethrocele continue after any accompanying inflammation of the urethra has been relieved, it may be necessary to excise the sacculated portion of the urethra by incision through the vaginal wall and close the wound by suture.
Urethral Caruncle.—The urethral caruncle is a small raspberry-like tumor situated at or just inside of the external meatus. It is composed of dilated capillaries set in a dense stroma of connective tissue and covered with 435 mucous membrane. The tumor varies in size from a pin-head to a hickory-nut. In color it varies from a pale to a bright red. It is usually situated upon the posterior wall of the urethra. There may be two or more such· tumors around the circumference of the meatus, and occasionally they are found in the vestibule. The growth is usually sessile.
The caruncle is often erectile in character, and increases in size at the menstrual period.
The growths bleed very easily on manipulation, and are exquisitely sensitive. The urethral caruncle is the commonest neoplasm of the urethra.
Symptoms.—The most marked symptom of urethral caruncle is pain. Intense pain is experienced at micturition and upon contact with the clothing or other body. Sexual connection is sometimes rendered impossible.
There is usually more or less hemorrhage from the tumor, which may rarely be so profuse as to cause marked anemia. The general health suffers, and nervous symptoms, resulting from the pain and loss of sleep, are often present to a pronounced degree.
Treatment.—The treatment consists in the total extirpation of the growth. It should be picked up with forceps and excised with the knife or scissors. The edges of the mucous membrane should be united by sutures.
Excision should be complete or the tumor may return. In case of recurrence a second operation should be performed.
Urethral Cysts.—Small cysts are occasionally found in the course of the urethra. They may occur at any point from the internal to the external meatus. They are caused by obstruction and distention of the urethral glands. They produce no symptoms unless large enough to cause obstruction to the flow of urine. They may be seen by the endoscope or may be palpated through the vaginal wall.
The treatment consists of incision and removal of part of the cyst-wall.
Polypus.—Mucous polyp of the urethra is of very rare 436 occurrence. The tumor generally has a delicate pedicle, and may protrude from the meatus. It is painless, and causes discomfort only by obstructing the flow of urine.
The treatment consists of removal by torsion, ligature, or excision.
Sarcoma and cancer of the urethra have rarely been observed. The phenomena are those similar to cancer in other parts of the body.
The treatment consists in thorough removal.
The urinary bladder has three coats—an outer incomplete peritoneal investment, a middle muscular coat, and an inner lining of mucous membrane.
The empty bladder is always collapsed, its walls being in apposition. A median sagittal section of the bladder and urethra shows a Y-shaped fissure lying between the symphysis pubis and the uterus, the uterus lying anteverted upon the upper surface of the bladder.
For convenience of description the bladder is divided into three parts—the corpus, or body, the fundus, or base; and the cervix, or neck.
The body of the bladder is all that portion that lies above the plane of the vesical orifices of the ureters and the center of the symphysis pubis.
The part lying below this plane is the base.
The vesical triangle, or the trigone, is that triangular area in the base of the bladder, the angles of which are marked by the vesical orifices of the ureters and the internal meatus of the urethra.
The neck of the bladder is the funnel-shaped portion where the bladder merges into the urethra.
The mucous membrane of the bladder is covered partly with squamous, partly with cylindrical epithelium. The mucous membrane is loosely attached to the muscular coat throughout the body of the bladder, so that when the organ is contracted the membrane is thrown into uneven 437 folds. The mucous membrane is much more closely attached to the underlying structures in the region of the vesical triangle, and it here preserves a smooth surface when the bladder is collapsed.
The vesical triangle is more richly supplied with nerves than are the other portions of the bladder, and is consequently the most sensitive portion.
The vesical orifice of the ureter appears as a dimple, a small truncated cone, or a pin-hole or slit on the mucous membrane.
A transverse band or fold of mucous membrane, known as the intra-ureteral ligament, extends between the orifices of the ureters.
The dimensions of the vesical triangle are subject to individual variations. The triangle is usually equilateral, its sides varying from 1 to 1½ inches in length. The vesical orifices of the ureters are therefore situated at points lying from ½ to ¾ of an inch from the median line—a useful fact to remember in opening the bladder through the vagina.
The vascular supply of the bladder is intimately associated with that of the uterus—a fact that explains the sympathetic disturbance of the bladder in uterine disease. The interior of the normal bladder is of a dull gray-red color. When distended, as in making an endoscopic examination, the minute arteries and veins may be plainly seen upon the surface.
The pressure of the urine in the bladder may be determined by the manometer. In the erect posture the intra-vesical pressure has been found to vary from 12 to 16 inches of mercury. In the recumbent posture the pressure is reduced to from 4 to 6 inches.
Cystitis.—Cystitis, especially of the subacute or the chronic form, is a common disease in women. The pathological changes resemble those seen in inflammation of mucous membrane in other parts of the body.
In the acute stage the mucous membrane is swollen and relaxed, and of a deep-red or hyperemic appearance. 438 Partial exfoliation takes place. The surface may be covered with thick, tenacious mucus or pus.
In the chronic stage the mucous membrane is of a muddy gray color, and may be more or less covered with a muco-purulent secretion. Ulceration, superficial or deep, may occur. The ulcer is sometimes deep and ragged and extends into the muscular wall.
In chronic cystitis we often find on the surface of the mucous membrane small localized areas of inflammation varying in size from ½ inch to 2 inches in diameter, and presenting a congested, granular, or eroded appearance, while the rest of the mucous membrane appears perfectly normal. These areas of inflammation bleed readily when touched. They are most often found in the base of the bladder, though they may occur in any part. When chronic cystitis is limited, it is usually confined to the vesical triangle.
The outer coats of the bladder may be involved in the inflammatory process, and become much thickened and hypertrophied. The ureters and the kidneys may become in time affected, through direct extension of the inflammation in the form of a ureteritis and pyelitis, or through obstruction of the vesical orifice of the ureters from inflammatory thickening. The alteration in the character of the urine is usually marked except in the mild forms of chronic inflammation. The specific gravity is low, varying from 1005 to 1018. In the chronic disease the urine is alkaline and ammoniacal. It contains blood, mucus, pus, and epithelial cells from the vesical mucosa.
Cystitis in women is usually caused by infection at catheterization. The very great improvement in the asepsis of this procedure that has taken place in recent years has in a corresponding degree diminished the frequency of cystitis.
Infection at catheterization is caused not only by the use of a dirty catheter, but by the conveyance of septic material from the external genitals or the urethra into 439 the bladder. For this reason the nurse or the physician should never pass the catheter by touch, as was sometimes formerly taught. The parts should be exposed to view, and the external genitals, vestibule, and meatus should be cleansed.
Cystitis may also be caused by extension of urethritis; by inflammation of adjacent organs; by abnormal urine; by constitutional diseases, as the exanthemata; by injuries to the bladder and displacement of this organ; and by retention of urine.
Symptoms.—The symptoms of cystitis vary with the stage and the character of the affection. Pain, frequent urination, and tenesmus are usually present.
In the acute stages there may be an elevation of temperature. There is a feeling of fulness in the bladder, with pain in the region of this organ. The pain is increased by motion and by the erect position, which increases the intra-vesical pressure. The pain is constant, and is not relieved by evacuation of the bladder. Pressure upon the base of the bladder through the vagina causes pain. This is a useful diagnostic point. There is a frequent desire to urinate, and the passage of urine is followed by straining efforts or tenesmus. The alteration in the character of the urine has already been mentioned.
In time the general system suffers from secondary renal disease and from absorption, through the bladder, of the ingredients of decomposed urine and septic material from the mucous membrane.
The diagnosis of cystitis is easily made by proper examination. It should always be remembered that not every woman who complains of painful and frequent urination and vesical tenesmus is necessarily suffering with cystitis. These symptoms are often caused by disease of the urethra, by displacement of the uterus, which drags upon the neck of the bladder, by the pressure of a tumor, or by displacement of the bladder such as may follow laceration of the perineum. 440
Women may often be seen who have been treated for weeks for cystitis without avail, and who are immediately relieved of all symptoms by the replacement of a retroverted uterus or the closure of a torn perineum. These conditions may in time result in cystitis, but the disease usually disappears with the cure of the causative lesion.
It is of the first importance, therefore, for the physician to make a careful pelvic examination, and to exclude all conditions that might cause irritation of the bladder. Microscopic examination of the urine, by revealing the presence of pus and blood and the epithelial cells of the bladder, is of value in making a diagnosis. The urine for examination should be drawn with the catheter, to prevent contamination from vaginal discharges.
Examination of the urine does not, as a rule, enable one to exclude inflammation of the ureters or of the pelves of the kidneys. If there is any doubt, it may be removed by the use of the endoscope, which will reveal the true condition of the bladder-wall.
As has already been said, tenderness upon pressure through the vagina on the base of the bladder is of diagnostic value in determining the presence of cystitis. In the mild forms of chronic cystitis—those characterized by local areas of inflammation—examination of the urine may throw no light upon the condition, as the secretion of pus or mucus is very slight. The diagnosis can then be made only by means of the endoscope.
It is perhaps advisable in all cases of chronic cystitis to use the endoscope, not only to confirm the diagnosis, but to begin the treatment by making direct local applications.
Treatment.—The treatment of cystitis is general and local. Local treatment should never be used in the acute stages of the disease. Many cases recover completely without any local treatment whatever.
In acute cystitis the woman should be put to bed. The irritation of the bladder is much relieved when the intra-vesical pressure is thus diminished. 441
The diet should be carefully regulated, all stimulating ingredients being withdrawn. An exclusive milk diet is the best.
Saline laxatives should be administered, and continued to the point of mild purgation. One dram of Rochelle salts every two or three hours, given in half a tumblerful of soda-water, is useful for this purpose. Large quantities of diluent drinks should be given, such as flaxseed tea or Vichy water.
If the urine is acid, citrate of potassium may be administered with the diluent drinks, so that from 1 to 2 drams of the salt are taken during the day. Bicarbonate of potassium in similar doses is also useful.
When the urine becomes ammoniacal, boracic acid, in doses of 10 grains from three to six times a day, is most useful. Benzoic acid, in doses of 10 grains three or four times a day, is also valuable.
A very good method is to make a pint or a quart of flaxseed tea, to dissolve in it the requisite amount of citrate of potassium or of boracic acid (as the urine is acid or alkaline), and to administer this in divided doses during the day. This treatment, with rest in bed, should be continued as long as the vesical pain and tenesmus continue.
If the pain and tenesmus are severe, small doses of opium may be given. It is, however, not advisable to use opium unless the suffering of the woman demands it.
If the disease, as the symptoms become less acute, does not progress satisfactorily toward cure, medicines that have a more stimulating effect upon the mucous membrane should be given, such as cubebs and copaiba, oil of turpentine, oil of eucalyptus, and oil of sandalwood.
Many cases of acute cystitis, if carefully treated in this way, will recover completely without the use of local treatment. If, however, the disease does not yield to these measures, local treatment becomes necessary.
In many instances the woman first comes under treatment when the disease has reached a chronic stage; or it 442 may be that the disease has begun subacutely, and has gradually progressed without having presented any symptoms of acute onset. Local combined with general treatment is then often advisable from the beginning.
Local treatment consists of general applications made to the whole of the interior of the bladder through the catheter; direct application, limited to the diseased portions of the mucous membrane, through the endoscope; and operation, or the formation of a vesico-vaginal fistula.
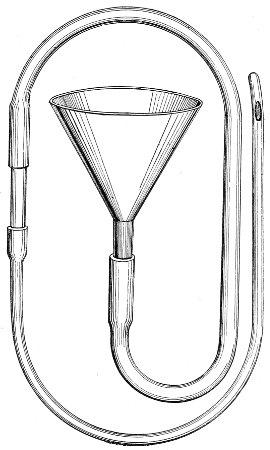
Fig. 191.—Apparatus for washing the bladder.
Washing out the bladder with sterile warm water, either pure or medicated, is often very useful. Gentleness in manipulation and asepsis should be carefully observed in this procedure, or much more harm than good may result from it. The operation, if properly performed, should never give pain to the woman.
A very simple apparatus is required, consisting of a 443 soft-rubber catheter, of moderate size, attached to a small glass funnel by means of a rubber tube and a piece of glass tubing. The whole is about 2 feet long (Fig. 191).
The catheter, slightly lubricated at the point, should be gently introduced into the bladder, and the urine should be slowly withdrawn. As the urine flows into the funnel its character may be observed. The rapidity of the flow of the urine may be regulated by raising or lowering the funnel. As the last portion of the urine is withdrawn the flow should be very slow, in order to prevent injury to the vesical mucous membrane from dragging it into the eye of the catheter.
When the bladder is emptied, sterile hot water may be introduced through the funnel and the process of withdrawal repeated. The mucus, pus, or blood which had remained in the bladder after evacuating the urine may be examined as the water flows into the funnel. This process may be repeated several times if necessary to wash out the bladder. The water should be about the temperature of the body (100° F.). It is less irritating to the mucous membrane if there is dissolved in it boracic acid or common table salt, about 1 dram to the pint, though these ingredients should not be added if they act chemically on the substances subsequently used in the medicated solution.
The quantity of water introduced into the bladder may be regulated by the feelings of the patient. The distention of the bladder should never be great enough to cause pain. Usually an ounce of fluid is all that can at first be tolerated without producing pain. As improvement takes place more fluid may be introduced in the subsequent treatments.
After the bladder has been washed out in this way, applications may be made to the interior by pouring through the funnel the desired medicated solution, the most useful one being a weak solution of nitrate of silver (gr. j or ij to ℥j). This solution should be retained in the bladder for a few minutes, and should then be withdrawn. 444
A solution of sulphate of copper (gr. j-iv to ℥j) is also useful.
At first daily irrigation and application should be thus practised. As the case improves the intervals between the treatments should be lengthened.
This local treatment should always be combined with the general treatment already prescribed—rest in bed if possible, a milk diet, and the administration of boracic acid internally.
Application through the Endoscope.—If the endoscope is used in the first place for diagnosis in a case of chronic cystitis, much time that might otherwise be wasted in unnecessary or useless forms of treatment may be saved. The condition of the parts maybe accurately determined, and the proper form of treatment may be instituted. It may, for instance, be seen that deep ulceration is present, or that other lesions of the bladder are so extensive that the quickest plan of cure will be to proceed immediately to the formation of a vesico-vaginal fistula, without attempting to treat the disease by applications.
Applications may be readily made through the endoscope to any part of the interior of the bladder. Applications made in this way are most useful when the disease is localized. Stronger solutions may be used on the affected areas than when the application is made to the whole surface of the organ.
When the disease is limited to the vesical triangle or to local areas situated elsewhere, the inflamed spots should be touched with a solution of nitrate of silver (gr. v-xx to ℥j). Much benefit is frequently derived from one such application, in connection with the general treatment already indicated. The applications may be made every few days. The procedure causes less discomfort to the woman as she becomes accustomed to it.
Cystotomy.—In cases of ulceration of the mucous membrane, or when the disease has resisted the milder forms of treatment, it may become necessary to perform cystotomy, to furnish an opening for the continuous drain of 445 the urine, and to put the bladder at rest by relieving it from all functional action. This is a most valuable therapeutic operation in cases of obstinate cystitis.
In performing cystotomy the anatomical relations of the ureters and the internal orifice of the urethra must be kept in mind. It will be remembered that the ureters terminate in the bladder at points situated from ½ to ¾ of an inch from the median line.
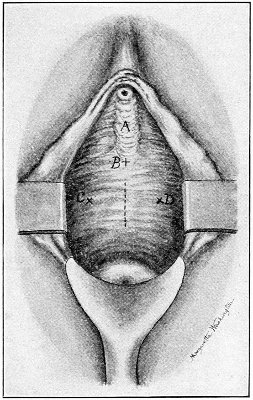
Fig. 192.—Illustration of the position of the incision in vaginal cystotomy, and the relations of the urethra and the ureters: A, anterior vaginal column; B marks the position of the internal urinary meatus; C and D mark the orifices of the ureters. The distance from C to D varies from 1 to 1½ inches. C, B, D is approximately an equilateral triangle.
The course of the urethra is indicated by the anterior vaginal column, which is a single or double thickening of mucous membrane traversed by short transverse folds or ridges. It begins near the external meatus and extends upward for about an inch. The internal meatus may be very approximately located by the upper end of this anterior vaginal column. The incision into the bladder should be made in the median line above this point. 446
The operation should be performed under the influence of an anesthetic. The woman should be placed in the Sims or the dorso-sacral position. The anterior vaginal wall should be exposed with the Sims speculum. A sound should be passed into the bladder, and its point should be pressed against the posterior vesical wall toward the vagina, at the position where the incision is to be made. The incision should be made into the bladder through the tissues fixed on the point of the sound. The opening may then be enlarged with the knife or scissors. The opening should be from 1 to 1½ inches in length. In order to prevent spontaneous closure of the fistula, the mucous membrane of the bladder should be sutured to the mucous membrane of the urethra around the margin of the fistula.
The after-treatment consists in daily washing of the bladder with large quantities of sterile warm water or with the boracic-acid solution. The woman should be placed in the dorso-sacral position, and the fistulous opening should be exposed by the Sims speculum. The water should be introduced into the bladder through the urethra. Care must be taken to hold the edges of the fistula open, so that there may be a free channel of escape.
The patient should at first remain in bed. After the acute symptoms have disappeared she may get up and the frequency of the local treatments may be diminished. Various appliances have been introduced for receiving the continuously escaping urine. None of them, however, are satisfactory. They are difficult to keep clean, they cause pain, and they are liable to become displaced. The best method is to wear a vulvar pad of some absorbent material and to pay strict attention to cleanliness. The progress of the case may be determined by examination of the urine, and by examination of the vesical mucous membrane through the fistula or through the endoscope.
The time required for cure may extend from one to six months. 447
When the vesical membrane has been restored to a normal condition the fistula may be readily closed.
Vesical Calculus.—Stone in the bladder is less common among women than among men. This fact is probably due to the greater size and dilatability of the female urethra, on account of which small calculi may readily pass out.
The symptoms and methods of diagnosis of vesical calculus are similar to those in the male. The stone may often be palpated by bimanual examination.
Treatment.—Small stones uncomplicated with cystitis may be crushed and removed through the urethra. Large stones should be removed by cystotomy. Whenever cystitis is present, it is advisable to perform cystotomy and to make a permanent fistula until the cystitis is cured, when the opening may be readily closed. 448
Gonorrhea in women has been considered disconnectedly in the preceding pages as one of several pathological conditions that affect the different parts of the genital tract. A more connected discussion of the subject will be of value, in view of the frequency of the disease, its often unsuspected or insidious character, and the serious and fatal lesions that it may produce. Lying between the two specialties of venereal diseases and gynecology, it is often ignored or slighted by both.
Acute gonorrhea in the female is much less frequent than in the male. It is rare in the gynecological dispensaries of Philadelphia to see acute gonorrhea of any part of the genito-urinary tract.
The disease is very often subacute or chronic from the beginning, and is not, as in the male, always preceded by a period of acute invasion, the symptoms of which necessarily attract the attention of the patient and the physician. For this reason gonorrhea in the woman is very often overlooked. We can as yet form no accurate estimate of its frequency. Certain lesions, such as pyosalpinx, which may be the remote result of gonorrhea, are often, especially by gynecologists, indiscriminately attributed to this disease without anything like sufficient evidence of such a causative relation.
The fact that the husband may at some time of his life have had gonorrhea, or even that the woman may have had gonorrhea, is no evidence that a pyosalpinx that appears in later years has been caused by this disease. There are many other causes of pyosalpinx besides gonorrhea. The frequent causative relation of sepsis 449 at labor, miscarriage, or criminal abortion, or during the intra-uterine manipulations of the physician, should always be remembered.
I have no intention of underrating the danger to the woman of coitus with a man who is not entirely cured of a gonorrhea or a gleet. The lives of a great many women have been ruined by marriage with incompletely cured gonorrheal husbands, and but very few men in such a condition would contemplate marriage if they were aware of the danger to the woman that results from such an act. But, on the other hand, men who are at all careful of themselves are, without doubt, usually completely cured of gonorrhea; and there are thousands of men in the community who have had one or more attacks of gonorrhea before marriage, and who have now healthy and prolific wives. Every physician of experience will find such examples in the circle of his own practice or acquaintance. It is very unscientific to lay the responsibility upon such husbands for every pelvic inflammatory condition that may appear in their wives.
The difficulty of proving the presence of gonorrhea in women is often very great. As has been said, the disease may begin and may exist for a long time without attracting the attention of the woman. She often pays no attention to a slight burning or tickling sensation in the urethra, which passes off in a few days. She may have had a leucorrheal discharge for a long time, and she may fail to notice any slight alteration in its character or quantity that may have been caused by gonorrhea.
There is nothing in the gross appearance of the discharge from any part of the genital tract which is absolutely pathognomonic of gonorrhea. The condition may be suspected if there is a purulent discharge from the urethra, because urethritis in women is very generally of gonorrheal origin. But, on the other hand, there may be an innocent-looking mucous discharge from the cervix, such as occurs in health or in mild non-specific conditions, yet in which gonococci may be found. 450
The presence of the gonococcus is, of course, positive evidence of gonorrhea. But this organism may be present in small numbers and escape detection even at the hands of experienced observers; or it may be present in the tissues of the infected region and fail to appear in the discharge; or it may in time itself disappear altogether. And thus, when the woman begins to suffer from some of the remote lesions of gonorrhea, such as an endometritis or a salpingitis, and is driven to seek medical advice, she may be unable to give any history whatever of the beginning of the disease; the character of the secretions may teach the physician nothing; the gonococcus may have disappeared from the genital discharge; and though a pyosalpinx may be present which had originally been caused by gonorrhea, yet the gonococcus may likewise have disappeared from the tubal pus, and other pathogenic organisms may be found in its place. It becomes impossible to determine the true origin of the disease.
For these reasons, if the physician is accurate in his observations, and classifies as gonorrheal only those cases the specific origin of which he can prove, the frequency of gonorrheal lesions in women will be considerably understated.
Sanger states that in about one-eighth of all gynecological diseases gonorrhea is the underlying cause. Taylor, viewing the condition from the side of the venereal specialist, says that this statement is conservative and probably nearly correct.
It must be borne in mind that gonorrhea is sometimes caused in other ways than by coitus. This is seen in the epidemics of gonorrhea that occur in children. It is without doubt sometimes caused by the use of an infected vaginal syringe. Cases of rectal gonorrhea are not infrequently thus produced.
Gonorrhea in women may attack any part of the genito-urinary tract. It rarely attacks a number of structures at one time, but it usually becomes localized in one 451 or two parts, such as the urethra, the glands of the vestibule, the vulvo-vaginal glands, the vaginal fornices, or the cervix uteri, and runs a subacute course, and may remain quiescent for a long period. It may in time disappear spontaneously, or it may be excited into activity by a variety of causes, such as traumatism, unusual coitus, labor, or miscarriage. The parts of the genito-urinary apparatus that are covered by pavement epithelium are much more resistant to the gonococcus than are the parts covered with cylindrical epithelium. For this reason the external genital surface and the vagina of the woman, and the vaginal aspect of the cervix, are often exempt when other less resistant structures are attacked.
Gonorrhea attacks the different parts in the following order of frequency: the urethra, the cervix uteri, the vulva, and the vagina.
Gonorrhea of the urethra is the most common form of the disease. The great majority of the cases of urethritis in women are of gonorrheal origin. Whenever there is a purulent or muco-purulent discharge from the urethra gonorrhea should be suspected, whether or not the gonococcus is found in it.
The disease may linger in the mucous glands found near the external meatus and in Skene’s glands for a long time. The symptoms of this condition have already been considered. The disease may present all the phenomena of acute urethritis in the male, or it may be subacute from the beginning.
Gonorrhea of the cervix uteri occurs next in frequency. As far as the few accurate observations that have been made teach us anything, gonorrhea of the cervix is but little less frequent than gonorrhea of the urethra. The disease may exist in conjunction with gonorrhea of some other part, or it may occur alone. The infection takes place directly from the discharge of the penis which comes in contact with the external os. Gonorrhea of the cervix usually begins in a subacute or an insidious manner. It is usually unattended by any general or 452 local symptoms sufficiently marked to attract attention. If the woman had been free from a leucorrheal discharge, she may observe a muco-purulent secretion caused by the gonorrhea. If she had a leucorrhea, the alteration in the character and amount of the discharge is usually not sufficient to attract her attention. In some cases the discharge becomes more purulent in character; in others there is no alteration perceptible to the naked eye.
If the disease runs an acute course, the appearance of the cervix will be that characteristic of acute inflammation. The vaginal cervix is congested; the external os is patulous and is surrounded by a red granular or eroded area, while from it is seen escaping a purulent discharge.
Pelvic pain or discomfort is not usually present unless the body of the uterus is attacked.
All the symptoms of gonorrheal inflammation of the cervix are found in simple non-specific conditions. The only certain diagnosis is made by means of the microscope; and even failure to find the gonococcus will not enable the physician to say with certainty that the disease is not of gonorrheal origin. The gonococcus may be found in any form of discharge from the cervix, even that which to gross examination appears most innocent.
Consequently, in every suspected case a microscopic examination should be made.
The discharge, for examination, should be taken from the cavity of the cervix by means of a sterile platinum loop. If no gonococci are found, a strip of mucous membrane from the cervical canal should be removed with a sharp curette, and it, with the discharge that adheres to it, should be carefully examined.
It may be advisable to examine the discharge immediately after menstruation. A cervical discharge is always increased immediately before, during, and after a menstrual period. This is probably the reason that men are more liable to contract gonorrhea at that time. This fact is so well known that there is a widespread popular belief that gonorrhea may be acquired from coitus, during 453 a menstrual period, with a healthy woman. This is not true. A man cannot acquire gonorrhea from a woman unless she had been previously infected with the disease; otherwise a woman might develop gonorrhea in herself spontaneously, for her discharges come in contact with her own genito-urinary tract.
The greater liability to infection at the time of menstruation is due to the fact that an existing pathological discharge is increased in amount; a subacute disease is rendered more active by the menstrual congestion; and gonococci, quiescent in the superficial cells, are more likely to be thrown off at this time.
Gonorrhea of the cervix very often stops at the internal os. It may, however, extend to the body of the uterus and to the Fallopian tubes, as has already been described. The diagnosis of gonorrheal endometritis can be made only by microscopic examination of the discharge or of a strip of the endometrium removed with the curette.
The gonorrheal discharge of the cervix may infect, secondarily, local areas of the vagina. The most usual position of secondary infection is the posterior vaginal fornix. A red eroded area, caused in this way, is often found. The prolonged contact of the pus produces a localized vaginal gonorrhea.
Primary vaginal gonorrhea is rare in the adult woman, in whom there is the usual resistant power of the epithelium. The mucous membrane of the vagina becomes tough from coitus and childbirth, and is usually impregnable to the gonococcus. Bumm has kept gonorrheal pus in contact with the vaginal wall for twelve hours without producing any inflammatory reaction.
In girls and in young women, in whom the mucous membrane of the vagina is soft and hyperemic, vaginal gonorrhea is more likely to occur. Like gonorrhea in other parts, the disease may be acute or chronic. It may involve the whole vaginal tract or it may be restricted to local areas.
The disease sometimes involves only the lower portion 454 of the vagina, and is most severe on the posterior wall. In other cases it is limited to the posterior vaginal fornix, where it has a tendency to become localized and to persist. In the very early stage the mucous membrane is dry and red. It later becomes covered with a purulent or muco-purulent secretion of a milky color.
If the disease is extensive, severe symptoms may be present. The woman will suffer with burning pain in the pelvis, the pain being increased by any movement.
Acute inflammation of the vagina is usually of gonorrheal origin. A thorough examination of the condition can be made only by placing the woman in the knee-chest position and by exposing the vagina by retracting the perineum with the Sims speculum. The whole vaginal tube, especially the posterior wall near the ostium and the fornices, should be carefully inspected.
Gonorrhea of the vulva may arise primarily, or it may be caused by infection from discharge from the vagina or the cervix. Like gonorrhea of the vagina, it is rare in the adult woman. It is usually seen in girls or in young women. Its occurrence in children has already been referred to.
The disease may extend to the small glands of the vestibule and the fourchette and to Bartholini’s glands; in these situations it may lurk for many years, forming a source of infection to men and a great element of danger to the woman. Suppuration of the glands of the vestibule may result in small urethral fistulæ.
In making an examination of the external genitals the parts should always be thoroughly exposed and the physician should attempt to express the fluid from the orifices of the glands. Microscopic examination of the discharge should be made.
Inflammation of any of the glands of the external genitals is usually the result of gonorrhea.
When the physician examines a woman suspected of gonorrhea, she should not prepare herself beforehand by vaginal douches and washing the external genitals. The 455 urine should not have been voided for some time. Prostitutes, fearing that gonorrhea will be discovered, often remove all discharges as much as possible before they submit to examination. Other women do the same from motives of cleanliness. As the diagnosis depends upon observation of the origin and character of the discharges, such preparation should be avoided.
As has already been said, it may be advisable in doubtful cases to make the examination immediately after a menstrual period, when the discharges are more profuse and perhaps more virulent than at other times. The examiner should always proceed methodically, and should inspect every portion of the external genitals, the vagina, and the cervix. The vestibule, the external meatus, the urethra, the fourchette, the glands of Bartholini, the vaginal walls, the external os, and the cervical canal should in turn be examined. Discharges obtained from these structures should be saved and submitted to microscopic examination.
Though the gonococcus is by no means always found in cases the specific character of which is proved by infection of the man, yet it would escape observation much less often if such thorough examination were made.
If the gonococcus is not found, the diagnosis must be made from the consideration of the lesions that we know occur but rarely except in gonorrhea. Thus, urethritis is a strong diagnostic point in favor of gonorrhea; so is inflammation of the glands of the vestibule, of the fourchette, and of the vulvo-vaginal glands. Vaginitis not caused by the degenerations of old age, by traumatism, or by the discharge from a cancer of the cervix or from a vesico-vaginal fistula is usually of gonorrheal origin. This is especially true of vaginitis localized in the vaginal fornices.
Gonorrhea in women should be most carefully treated until all signs of the disease are eradicated. The treatment has already been discussed under the consideration of the different structures that may be attacked. Gonorrheal 456 cervicitis and endometritis are the most difficult to cure, and it may be impossible to determine with certainty that the disease has been eradicated from these structures. If milder measures fail, the cervical canal and the body of the uterus should be completely curetted, and the raw surface should be treated with pure carbolic acid. The physician should never discharge the patient until she is thoroughly cured. 457
The technique of some of the special gynecological operations, such as perineorrhaphy, and trachelorrhaphy, has already been considered in discussing the treatment of the conditions in which such operations are applicable. The general and local preparation of the patient, the instruments, the dressings, etc., and the technique of the general operations of gynecology that are applicable to a variety of different pathological conditions, such as oöphorectomy and hysterectomy, now demand consideration. The general rules of asepsis that are followed in gynecological operations are the same as those that should be observed in all surgical operations. And although every surgeon should strive to attain perfect asepsis in all operations, yet it is of especial importance for the gynecologist to do so, for he, more often than all others, invades the peritoneal cavity. Of the various structures of the body, the peritoneum is one of the most susceptible to septic influences; and septic infection of the peritoneum, unlike infection of other structures, implies not merely a local disturbance and delay of healing, but general sepsis and death.
Moreover, the gynecologist, operating in the peritoneum, cannot correct any imperfection in his aseptic technique by the use of antiseptic solutions, as can be done in other operations of general surgery. Such antiseptic solutions, if of sufficient strength to be of any value as germicides, are very dangerous in the peritoneum. They may produce fatal poisoning from absorption through the peritoneum; they destroy the delicate peritoneal surface, and thus diminish the very useful power 458 of the peritoneum to absorb blood and serum after the operation; they cause intestinal and other adhesions; and they so impair the integrity of the intestinal walls that septic organisms may be enabled to pass through and infect the general peritoneum.
The gynecologist, thus debarred from the use of antiseptics during a peritoneal operation, must rely altogether upon the perfection of his aseptic technique.
It must not be forgotten that the danger of peritoneal infection, though very much less in the minor gynecological operations on the perineum and the cervix, is yet never altogether absent. The whole genital tract of women communicates directly with the peritoneum, and infection at any point may extend and cause fatal peritoneal sepsis.
The danger increases with the proximity of the infected point to the peritoneum. The danger of salpingitis and peritonitis from trivial intra-uterine manipulations not performed aseptically, such as the passage of a dirty sound, has already been referred to. Fatal peritonitis has followed trachelorrhaphy.
In the various plastic operations of gynecology disastrous results are, of course, not so likely to occur from imperfect asepsis as in those operations that involve opening the peritoneum. In some of these operations, such as closure of a vesico-vaginal or a recto-vaginal fistula, it is impossible to obtain perfect asepsis.
In minor gynecological operations, however, we may use antiseptic solutions which are inadmissible within the peritoneum; and the vascularity of the genital tract is so great that healing is usually rapid and perfect even with very imperfect asepsis. This fact, however, should never justify carelessness on the part of the physician. In every surgical procedure, however trivial, the strictest asepsis should always be observed. The practice avoids, at any rate, a minimum danger; it is a useful training for the physician; and it sets a valuable example to the assistants and nurses. No part of the technique should 459 be “good enough.” It should be as good as it can be made.
The greatest factor in the success of modern gynecology has been asepsis. The doctrine has become so widely spread that the technique, and consequently the results, of careless operators of the present day are much better than those of the best operators before the days of Listerism.
This is not said to justify carelessness. No woman should at operation be exposed to any dangers not inseparable from her condition. The assistants and the nurses should be especially made to feel the responsibility of their positions. A careless nurse or assistant may introduce sepsis and cause death after the most skilfully performed operation. Unfortunately, there is not a distinct realization of this fact. An assistant, though conscious of some carelessness of his own, usually beguiles himself with the belief that death was due to some other cause. If there were a distinct realization of personal responsibility among all concerned at an operation, death from infection through carelessness would be avoided as are other kinds of manslaughter. Unless a surgeon knows that he can furnish the proper aseptic conditions, he has no right to advise a patient to submit to operation unless the disease is such that operation is demanded under any circumstances.
At the present day the gynecologist advises a woman to submit to a serious—potentially fatal—operation, like celiotomy, for the relief of many conditions which cause suffering, but which do not cause death. He does this conscientiously, because he knows that if the operation is properly performed the danger to life is very small. If he is not certain that the proper operative conditions will be at hand, he cannot conscientiously give this advice, and he had better follow some palliative treatment.
Operations are always better done in a well-equipped operating-room than in a private house. In the operating-room we have better asepsis, better light and mechanical 460 appliances, better discipline of assistants and nurses, and greater opportunity of successfully dealing with unexpected complications.
In an operation which is performed in a private house something is always used which is more or less of a makeshift; and makeshifts should not be used in surgery, especially in abdominal surgery. If we hope to obtain perfect results, we must insist upon perfect surroundings and appliances. Continuous success is the result of scientific accuracy and attention to detail. I say continuous success, because this is the only test of good surgery. We should not be misled by occasional brilliant results obtained under imperfect conditions. In such circumstances the operator admits to himself that his patient was lucky. The element of luck should be entirely eliminated. Nothing should be trusted to luck.
Fortunately, most of the operations of gynecology are performed for conditions of such a character that there is no demand for instant operation. The woman can usually wait until suitable conditions are furnished. In cases of emergency the surgeon can only do his best under the existing circumstances, not his best under the best circumstances.
It cannot be denied that good results, as far as mortality is concerned, are obtained in abdominal operations in private houses. The mortality, however, for a long series of cases of all kinds is greater than that obtained in well-equipped hospitals by operators of equal ability. The number of incomplete and imperfectly performed operations is much greater in private houses than in the hospital, for the operator with imperfect surroundings fears to deal radically with some unexpected conditions which he meets, and is satisfied if the woman’s life is saved, though she be not perfectly cured.
It is not necessary to dwell upon the need of proper training of the operator himself in abdominal surgery. The minor gynecological operations may be performed 461 by any one who is familiar with the ordinary principles of surgery and who understands the special technique of the operation. There is no fear of unexpected complications in such operations. Rapidity of work is not essential, as in abdominal surgery, and the operator may study the condition as he proceeds; moreover, errors arising from inexperience or ignorance are not attended by fatal results.
In abdominal surgery, however, the operator should be specially trained for the work. Except in cases of emergency, he should not perform these operations unless he expects to do so continuously. He should be trained by work upon the cadaver and the lower animals and by watching and assisting experienced operators. He should be prepared to deal, without hesitation, with every pathological condition that may be met with in the abdomen; a glance at works on abdominal surgery will show how numerous such conditions are.
A few successes in simple cases in the hands of an incompetent operator will lure him on with false confidence until he finally meets a condition with which he is unable to cope. Either the patient dies as a result, or, if the operator be conservative, the abdomen is closed over an incomplete operation.
The directions which are about to be given apply especially to those operations in which the peritoneal cavity is entered. They may be modified in obvious particulars in case a minor operation is to be performed upon the vagina or the uterus. In such cases special abdominal cleansing is unnecessary and complete evacuation of the intestinal tract is not so important.
The technique described is that which is followed by the writer. Various equally good modifications are employed by other operators. It seems best, however, to give but one rigid method which experience has proved successful. The experienced operator is able to change it according to his individual preferences.
Operating-room.—The operating-room should be 462 well lighted from the top and at least one side. If a good natural light cannot be secured, an electric drop-light will be found very convenient. For work deep in the pelvis or the abdomen a good light is essential. If necessary, light may be directed to the desired point by means of the ordinary head-mirror.
The floor, walls, and ceiling of the room should be of some non-absorbing material. There should be in the room no appliances whatever that are not essential for the performance of the operation.
The interior of the room should be wiped throughout with a mop or with wet cloths, or, still better, flushed with the hose, in order to remove and lay all dust. The room may be wiped throughout with a solution of bichlorid of mercury (1:2000). At the Gynecean Hospital the operating-rooms are disinfected once a week with formaldehyd gas.
The temperature of the room should be not less than 75° F. Shock from bodily loss of heat and exposure of the peritoneum is diminished if the atmosphere of the room is at an elevated temperature.
Apparatus.—All apparatus, such as basins, tables, etc., should be of such a character that it may be sterilized by boiling or by washing with a solution of bichloride of mercury (1:1000). Glass-top tables with painted or nickel-plated frames are preferable. The operating-table should be so arranged that the patient may be placed in the Trendelenburg position (Fig. 193). This position permits the intestines to gravitate out of the pelvis, and is very useful in many operations. There are a great variety of tables in use. Before the Trendelenburg posture was introduced the writer used for several years a plain hard-wood plank supported by two wooden horses. The Boldt table is very convenient. With it there is no necessity for a rubber pad for catching fluids. It is applicable for all gynecological operations. Some operators are in the habit of dressing the operating table by placing on it a blanket and sheet. This is unnecessary, unless the patient is in such a condition of collapse that it is 463 essential to preserve all bodily heat. The blanket usually becomes saturated with fluids and serves no good purpose.
The number and arrangement of the basins, tables, stands, etc. used in an abdominal operation are shown in Fig. 194.
The basins are best sterilized by boiling, or by washing with scalding water (inside and outside) and a solution of bichloride of mercury (1:1000).
The tables and stands are sterilized by washing with the bichloride solution. If wooden-top tables are used, they should be covered with a towel wrung out of a 1:1000 bichloride solution.
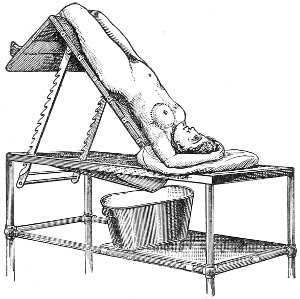
Fig. 193.—Trendelenburg position.
Operator, Assistants, Nurses.—Usually one assistant, who stands opposite the operator, and two nurses, are sufficient. A second assistant, standing beside the operator, is useful to thread needles and to hand instruments and ligatures. The operator, assistants, and nurses should possess such general cleanliness as follows a morning bath. They should not attend any patients suffering with a septic or infectious condition upon the day of the operation. If they have done so upon the previous day, they should subsequently take a general 464 465 bath and change all clothing. Care in this respect is especially desirable on the part of the nurses, whose long hair prevents easy cleansing of the head.
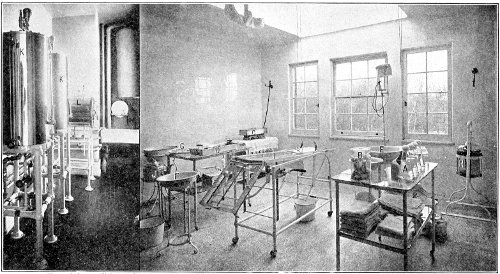
Fig. 194.—View of the sterilizing and operating rooms of the Gynecean Hospital, Philadelphia. The apparatus is arranged for operation. A, flasks of sterile water; B, jar containing silk ligatures in glass tubes; C, instrument-sterilizer containing boiling water; D, tray containing sterile water for instruments at operation; E, basin for washing sponges; F, basin for washing hands of operator during operation; G, tray for sutures, ligatures, and needles; H, jar of cold sterile water; J, kettle of hot sterile water; K, water-sterilizer; L, dressing-sterilizer.
The operator and assistants should wear sterilized outer clothes—cotton shirt and duck trousers. A large sterilized apron put on immediately before the operation is an additional protection. The nurses should wear large sterilized aprons over freshly washed, if not sterilized, dresses.
The hands and forearms of the operator, assistants, and nurses should be bare and especially sterilized. The finger-nails should be short, rounded, and smooth. A long nail is difficult to clean, and in the case of the operator is dangerous, as it may lacerate important structures in the process of enucleation of a tumor. Enucleation of adherent growths is best done with the blunt finger, which passes along the planes of separation. The sharp nail may perforate an intestine or lacerate a blood-vessel, instead of pushing it aside.
The nails, fingers, hands, forearms, and lower part of the upper arms should be thoroughly scrubbed with frequently changed hot water and soap (preferably soft soap) and a large stiff nail-brush. The process should not be done hastily or but once. The soap should be repeatedly washed off and renewed. Five minutes, at least, should be devoted to the scrubbing. The hands and arms should then be similarly scrubbed with alcohol, and finally scrubbed with a solution of bichloride of mercury 1:1000. Immediately before proceeding with the operation the hands and arms should be rinsed in sterile water.
There should be a nail-brush for each solution used. The brushes should be clean and sterilized by boiling or by placing in the steam sterilizer.
After sterilizing the hands, the operator, the assistants, and nurses should touch nothing which is not sterile. If they are obliged to do so, the hands should be again washed.
Rubber gloves, such as are used in general surgery, are 466 very useful in the operations of gynecology. They may be worn to protect the patient in case the operator or the assistants are not certain of the sterility of their hands, or to protect the operator when working upon a septic patient. Rubber gloves should be sterilized in the steam sterilizer.
Sterilization of Dressings, Towels, etc.—The operating-cloths, aprons, sheets, towels, dressings, gauze pads, etc. are most conveniently sterilized by steam heat. The temperature should be at least 100° C. (212° F.). The dressings and bandages should not be too tightly packed, so that all parts may be exposed to the same temperature.
Several kinds of steam sterilizers have been introduced. The most easily obtained is the Arnold sterilizer. An apparatus like the Sprague sterilizer, in which the steam is superheated, is preferable, but, as it is not portable, it is adapted only for hospital use.
The dressings should be maintained at the elevated temperature for an hour or more. Although this method secures very good sterilization, yet there are certain spores which resist such elevated temperature even after a two hours’ exposure. The method of fractional or discontinuous sterilisation has therefore been introduced. Two or three successive sterilizations are practised at intervals of twenty-four hours. Spores which at first escape destruction will have developed into vegetative forms in the intervals, and are destroyed by the final sterilizations.
At the Gynecean Hospital all dressings are sterilized for three consecutive days for two hours each day. The dressings, towels, etc., after sterilization, should be preserved in sterile glass jars or other sterile receptacle.
Sterilization of Instruments.—Instruments, drainage-tubes, catheters, and any rubber appliance may be sterilized by boiling in water for fifteen to thirty minutes. A dilute solution (1 per cent.) of carbonate of soda is preferable, as the instruments are not so easily rusted, and this solution, when boiling, has greater germicidal qualities than plain water. 467
Very convenient instrument-sterilizers are made, in which the instruments are contained in a tray that may be lifted out and placed in the receptacle for containing the instruments during the operation. This receptacle or pan should itself be sterilized, and should contain sterile water, or preferably the sterile solution of bicarbonate of soda, in sufficient quantity to cover the instruments.
It is very convenient to keep on hand a saturated solution of carbonate of soda, sterilized by boiling, a small quantity of which may be added to the water in the instrument-tray. Rusting of instruments is diminished by this means.
Appliances that are injured by moist heat or by steam may be sterilized by thorough washing and soaking in a solution of bichloride of mercury (1:1000). It is useful to keep a large vessel of such a solution on hand, in which apparatus that is not injured by the bichloride may be placed.
The Water.—The water used during the operation, for washing the wound, the abdominal cavity, the sponges, and the hands of the operator and assistants, should be sterilized by boiling or by distillation. The water should be boiled for two hours a day on two consecutive days, or it should be boiled under pressure as in some of the modern water-sterilizers. If the water contain a perceptible sediment, it should first be filtered.
Very convenient water-sterilizers are made, from which the water may be drawn of any desired temperature, after having been both filtered and sterilized by heat. There should always be a large quantity of sterile hot water at hand. Water below the temperature of the body should not be introduced in the peritoneal cavity, and pads brought in contact with the intestines should be wrung out of hot water.
About fifteen gallons of sterile water are usually required in an abdominal operation.
The water should be preserved in sterile pitchers, basins, or other receptacles. 468
Glass flasks are very convenient for containing the water with which the abdomen or pelvis may be washed out. The water may be poured directly into the abdomen from the flask. The flask should be plugged with non-absorbent cotton to prevent the entrance of dust.
Some operators prefer to use a normal salt solution (sodium chloride gr. 90 to water ℥xxxiiiss) for washing out the peritoneum. Such a solution is probably less irritating to the peritoneum than plain water.
If the flasks are used for containing the water, it may be boiled in them, and then preserved by plugging with absorbent cotton until required at the operation. The temperature of the water used for abdominal irrigation should be 100° to 115° F.
Sponges.—In the minor operations about the vagina or uterus the field of operation may be kept clean by irrigation with sterile water or by the use of sponges. Small sponges in holders are commonly used. These sponges, after being washed free of sand and bleached if necessary, may be sterilized by soaking for twelve hours in a solution of bichloride of mercury (1:500). They should then be rinsed in warm water and preserved in a 3 per cent. watery solution of carbolic acid, which should be changed every week.
Artificial sponges, or gauze sponges, are the most convenient in abdominal surgery. They are cheap, and may be destroyed after each operation, and they are very easily and certainly sterilized in the steam sterilizer. Good marine sponges are so expensive that but few operators destroy them after they have been once used. The cleansing and sterilization of such sponges are tedious and uncertain. The gauze sponges answer every purpose.
The gauze sponges may be made of various sizes by sewing together about eighteen layers of plain absorbent gauze. The edges of the gauze should be folded in and hemmed to prevent the escape of loose threads in the 469 peritoneum. Some operators use sponges made by wrapping absorbent cotton somewhat loosely in gauze.
The number of sponges used should always be recorded before the operation. It is advisable to preserve the sponges in sets always of the same number, so that in every case the operator knows that this number, or some multiple of this number, of sponges has been used. The writer uses such sets of seven gauze sponges of the following sizes: one sponge 3 by 3 inches; one sponge 10 by 7 inches; five sponges 5 by 5 inches. Usually one such set of sponges is enough for an abdominal operation. In some cases, however, the first set of sponges may become soiled by the discharge from an abscess or a suppurating tumor, and it is advisable to discard these sponges and to complete the operation with a second clean set.
The number of sponges should never be altered during an operation by cutting one in two.
Sponges should never be removed from the operating-room until the abdomen has been closed and the sponges have been counted. If a sponge falls on the floor or in the vessel to receive slops, it should be put aside until the final counting is completed.
When a set of sponges is used, they should always be carefully counted as they are placed in the basin, for the nurse who prepared and put up the set may have carelessly miscounted them.
Accuracy in regard to the sponges is of the greatest importance. There are a number of recorded cases, and many unrecorded, in which sponges have been left in the abdomen. This accident is usually fatal, though there are several cases on record in which the sponge has made its way, by ulceration, into the intestine, and has been discharged from the anus, or has been removed by subsequent incision through the abdominal wall.
Discipline of the Operating-room.—The discipline of the operating-room should be most rigid. Perfect personal asepsis can be obtained only by continuous 470 watching and criticism. The work should be systematically divided among the assistants and nurses, and each should attend strictly to his or her own department, and to nothing else.
The first assistant should assist the operator with sponges, etc. The second assistant should attend to the instruments, ligatures, and sutures. The first nurse should wash the sponges and place them in a basin of sterile water beside the first assistant. She should also attend to the towels and dressings. The second nurse, under direction of the first, should change soiled water in the sponge- and hand-basins, etc.
No one should pick up anything that may have been dropped upon the floor, and no one, unless it is absolutely necessary, should touch anything that has not been sterilized.
Anesthesia.—With the exception of the operator, the anesthetizer is the most important person at an abdominal operation. A careful, experienced anesthetizer is desirable in all operations, but especially so in an abdominal operation. Much more depends upon him than upon the assistant. The custom of trusting the anesthesia to the least experienced man is reprehensible. Many fatal cases after celiotomy may be attributed directly to the anesthesia.
Every operator of experience has observed the difference in reaction between those patients who have been carefully anesthetized and those who have been improperly anesthetized. In a serious case attended by unavoidable shock the superadded depression of ether-poisoning may be enough to cause a fatal result.
The operator should have nothing to do with the anesthesia, and it should not be necessary for him to watch it. The anesthetizer should make a careful examination of the heart, and should be provided with a hypodermic syringe and the necessary stimulants, which he should use at his own discretion.
He should, of course, use the minimum amount of 471 ether. He should be familiar with the steps of the operation, and he should so regulate the anesthesia that the operator will not be impeded by the straining or struggles of the patient at critical moments.
Preparation of the Patient.—It is always desirable, when possible, to have the patient under observation for several days before operation. As I have already said, a more accurate diagnosis may be made by repeated examinations, and opportunity is afforded for the administration of medicines to improve the general condition. A weak woman about to submit to a serious operation is benefited by the administration of 1/20 grain of strychnine three times a day, for several days before the operation.
During this period the patient should receive a daily bath, a laxative when necessary to produce a daily movement, and a vaginal douche of one gallon of hot water every morning and evening.
The special preparation of the patient is directed to sterilizing the abdominal surface, the external genitals, and the vagina, and to emptying the gastro-intestinal tract. This preparation should begin twenty-four hours before the operation. During this time it is best to confine the patient to bed.
Thorough evacuation of the intestinal tract is very desirable in abdominal surgery. When the intestines are empty and collapsed, the various intra-abdominal manipulations are most easily performed. If the intestine is injured and it becomes necessary to repair it, or if any other intestinal operation is required, it may be performed most easily and with the greatest cleanliness if the gut is empty.
Though it is impossible to sterilize the intestinal tract, yet we most nearly approach the condition of sterilization by thorough evacuation of the bowels.
Twenty-four hours before the operation purgation should be begun by the administration of 1 dram of Rochelle salts, dissolved in half a tumblerful of water or soda-water, every hour until the bowels begin to move 472 freely. Five or six doses are usually sufficient. The lower bowel should finally be emptied thoroughly by an enema of soap and water administered three or four hours before operation. During the twenty-four hours preceding operation the diet should consist of light, easily digested, concentrated nourishment, such as milk, buttermilk, soft-boiled eggs, rare beef, soups, beef-tea, coffee, tea, and whiskey if necessary.
Unless the patient is very weak, no food should be given on the morning of the operation. If her condition does not warrant such abstinence, she may have a glass of milk, buttermilk, coffee, or milk-punch. Such food is required if the operation is performed late in the day.
In very feeble patients a nutrient enema may be administered about two hours before the operation.
A hypodermic injection of 1/20 grain of strychnine is often useful upon the morning of the operation when the patient is in poor condition.
Preparation of the External Genitals and Vagina.—The pubis and the external genitals should be shaved. The woman should be drawn down to the edge of the bed, and the anus, the external genitals, and the vagina should be scrubbed with green soap. The vagina should be washed throughout. The nurse may do this by inserting one or two fingers, or she may retract the perineum with the Sims speculum, and scrub the vagina, the fornices, and the vaginal cervix with cotton held in forceps.
The scrubbing should be followed by a vaginal douche of a gallon of hot water to wash out the soap, and then by a douche of two quarts of bichloride solution (1:2000). One hour before operation the vaginal douche of bichloride should be repeated, and the nurse should introduce in the vagina as far as the cervix a light vaginal tampon of gauze wet with the bichlorid solution. In every abdominal operation on women it is desirable that the external genitals and the vagina should be clean. It 473 may be necessary to pass the catheter or to perform some vaginal manipulation, or the vagina may be opened during the operation.
If the vagina is small or virginal, or if the woman is nervous, the nurse may be unable to perform the method of cleansing just described; and it is then necessary for the operator or the assistant to clean the vagina after the woman is anesthetized. Such cleansing should always be performed, in addition to the cleansing by the nurse, whenever a vaginal operation is performed or it is expected that the vagina will be opened from above. Thorough vaginal sterilization is most easily accomplished when the patient is under the influence of ether, as the perineum is easily retracted and the vagina becomes more patulous. The woman should be placed in the lithotomy position, and the washing should be performed with two fingers or with a soft brush like a jeweller’s brush, or with cotton in forceps. If necessary, the perineum should be retracted with the speculum. Green soap should be used, and the vaginal walls, the fornices, and the cervix should be thoroughly scrubbed. The soap should then be carefully washed out, and the scrubbing should be repeated with bichloride-of-mercury solution (1:2000).
The cleansing of the external genitals and the vagina is best done by the nurse after the final movement of the bowels and immediately before the woman has her general bath.
Sterilization of the Abdomen.—The patient should have a warm bath from head to feet upon the morning of the operation. The abdomen, from the ensiform cartilage to the pubis, should be scrubbed with a nail-brush. Special care should be devoted to cleansing the umbilicus. After this bath the patient should be dressed in a clean flannel undershirt and night-gown and should be placed in a clean bed.
The nurse should then wash the abdomen, from the ensiform cartilage to the pubis and from flank to flank, 474 and the upper third of the anterior aspect of the thighs, first with turpentine, second with green soap, and finally with ether, devoting special care to the umbilicus. The abdomen should then be covered with a large wet bichloride dressing (1:2000), which should not be removed until the patient is upon the operating-table. A towel wrung out of the bichloride solution and held in place by a bandage or binder will answer the purpose. A second cleansing of the abdomen by the operator or the assistant should be done after the patient is upon the table. The surface should be washed with green soap and sterile water, then with ether, and finally with the solution of bichloride of mercury. The washing should not be restricted to the central abdomen, but should extend over the upper parts of the thighs and the flanks, which may be exposed during the operation.
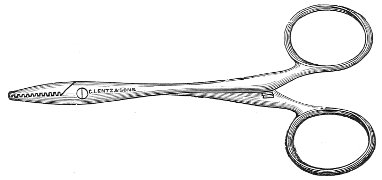
Fig. 195.—Tait’s hemostatic forceps.
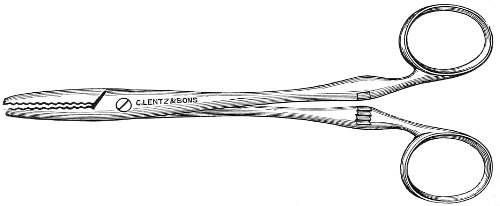
Fig. 196.—Spencer Wells’ forceps.
The bladder should be emptied by the catheter immediately 475 before the patient is placed upon the operating-table.
The patient should be placed upon the operating-table by clean nurses or assistants.
The legs should be strapped to the table. The hands should be held out of the way by the anesthetizer. They may be retained very well by a safety-pin passed through the lower sleeve and the shoulder of the night-gown or the pillow-case.
The undershirt and night-gown should be drawn well up behind, to prevent wetting. If the clothes become wet, they should be changed immediately after operation.
The legs and the chest should be covered with clean blankets. The field of operation should be surrounded by sterilized towels. One large towel with a hole of suitable size in the center is convenient. A pocket may be made immediately below the hole, to retain the instruments when the Trendelenburg position is employed.

Fig. 197.—Knife.
Instruments.—The number and the variety of instruments used by the gynecologist in abdominal operations depend a good deal upon the taste of the individual operator. The list given here comprises all the instruments that are found useful by the writer in abdominal work:
| Small hemostatic forceps (Fig. 195) | 12 |
| Medium-sized forceps | 2 |
| Large forceps (Fig. 196) | 4 |
| Knife (Fig. 197) | 1 |
| Scissors—two pairs of long scissors, one straight and one curved on the flat. | |
| Pedicle-needles (Fig. 198) | 2 |
| Cyst-trocars (Figs. 199 and 200) | 2 |
| Straight, spear-pointed needles, 2½ inches in length, for closing the abdominal incision by the mass-suture.476 | |
| Curved needles for suturing within the abdomen. Fine straight and curved needles for the repair of intestinal injuries. | |
| Large curved needles for catgut, etc. | |
| Abdominal retractors (blunt) | 2 |
| Needle-holder (Fig. 201) | 1 |
| Long dressing-forceps | 2 |
Three sizes of twisted silk are used for suture and ligature: heavy silk for ligature of the large arteries; medium silk for ligature of smaller vessels and for various suturing in the abdomen; fine silk for peritoneal and intestinal suture.

Fig. 198.—Pedicle-needle.
The silk should be as small as is consistent with secure ligature. The heavy silk is necessary for the ligature of pedicles in which a large amount of surrounding tissue is included with the artery.

Fig. 199.—Small curved trocar.
The silk is rolled on glass spools or on cores of gauze, contained in glass tubes plugged with cotton, and is then sterilized in the steam sterilizer by fractional sterilization. It is advisable always to use, for heavy ligature, silk of a uniform size, because the operator becomes accustomed to the strength of the silk and knows just how much strain it will bear. Silkworm-gut is the best material to use for suture of the abdominal incision in 477 case the “through-and-through” or interrupted mass-suture is employed.
The silkworm-gut should be of the heaviest and the longest size. It may be sterilized by boiling with the instruments before the operation.
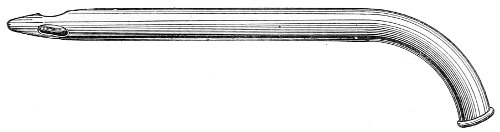
Fig. 200.—Large cyst-trocar.
Catgut is sometimes employed for ligature and suture. The difficulty of securing certain sterilization makes it advisable to avoid using this material within the peritoneal cavity. Sterilized silk is so certainly absorbed in all cases and is so easily employed that the writer has altogether given up the use of catgut within the peritoneum. It is useful as a buried suture for the muscle and fascia of the abdominal wall. Silk is not so certainly absorbed in this position, and if the catgut should happen to be imperfectly sterilized, no worse result than suppuration of the incision will occur.
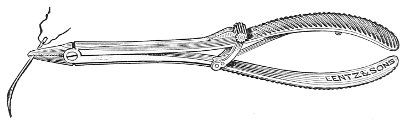
Fig. 201.—Reiner’s needle-holder.
Various methods of sterilizing catgut have been introduced. The writer uses the following method, which bacteriological experiments and clinical experience have shown to be good: The catgut is soaked in juniper oil for one week. The oil is then washed out with ether and the catgut is soaked in ether for forty-eight hours. 478 The gut is then rolled on glass spools and is placed in a glass jar containing pure alcohol. The alcohol is boiled in the jar for an hour at a time on several successive days. The gut is used directly from this jar, and is always boiled in the alcohol for an hour before each operation. In this way, if a considerable amount of gut is prepared at one time, it is subjected to many boilings before it is used up. The alcohol is boiled by placing the glass jar in a vessel of hot water.
The following methods of sterilizing catgut are also good:
The Claudius or Iodin Method for the Sterilization of Catgut.—Cut the catgut into the desired lengths and wind on glass slides or spools. Place in a wide-mouth jar with a glass stopper containing a solution composed of iodin and potassium iodide, each one part, and distilled water 100 parts. In making this solution the iodin and potassium iodide should first be pulverized in a mortar, the distilled water should be added, and stirred with the pestle until solution is complete.
At the end of eight days the catgut is sterile and ready for use. It may be kept indefinitely in the solution without deterioration. Before using take the catgut from the jar with sterile forceps and rinse in sterile water.
The Cumol Method for the Sterilization of Catgut, employed at the Johns Hopkins Hospital.—1. Cut the catgut into the desired lengths, and roll 12 strands in a figure-of-8 form, so that it may be slipped into a large test-tube.
2. Bring the catgut gradually up to a temperature of 80° C., and hold it at this point for one hour.
3. Place the catgut in cumol, which must not be above a temperature of 100° C., raise it to 165° C., and hold it at this point for one hour.
4. Pour off the cumol, and either allow the heat of the sand-bath to dry the catgut, or transfer it to a hot-air oven, at a temperature of 100° C. for two hours.
5. Transfer the rings with sterile forceps to test-tubes previously sterilized as in the laboratory. 479
The cleanest specimens of the crude catgut should be obtained for surgical purposes. There is no doubt that some specimens of crude catgut are more difficult to sterilize than others. A special apparatus has been introduced for sterilizing catgut which renders the process safe and certain.
The writer uses catgut only for suture of the abdominal fascia and muscles. Large-sized gut is employed.
The Dressing.—The dressing of the abdominal wound consists of ten or twelve layers of sterilized gauze, covered by a large sterilized abdominal pad about 1 inch thick, 13 inches long, and 9 inches broad. The pad is made of absorbent cotton enclosed in a layer of gauze. The dressing is retained in place by a six-tailed sterilized abdominal binder of flannel.
If no drainage through the abdominal incision is employed, the use of celloidin with the gauze dressing is of advantage. It retains the dressing securely in position for an indefinite period, and, if used liberally, it acts as a splint for the abdominal wall. Either of the two following formulæ given by Robb may be used:
| ℞. | Ether (Squibb’s), | |||
| Absolute alcohol, | āā. | ℥viss; | ||
| Of a solution made of 15 grains of bichloride crystals dissolved in 11 drams of absolute alcohol, | ♏xvj. |
Mix, and add of Anthony’s “snowy cotton” enough to give the solution the consistence of simple syrup.
| ℞. | Absolute alcohol, | ℥viss; | |
| Iodoform powder, | ʒxiiss; | ||
| Mix, and add ether, | ℥viss. |
Mix, and add of Anthony’s “snowy cotton” enough to give the solution the consistence of simple syrup.
The celloidin should be poured over the edges of the first layers of gauze that are placed upon the wound. 480
Abdominal Drainage.—Drainage of the peritoneum is accomplished by means of the glass drainage-tube (Fig. 202), or by capillary drainage with gauze. The peritoneum may be drained through the abdominal incision or through the vagina. On account of the difficulty of keeping the vagina sterile, drainage through the abdominal incision is the safer method. Vaginal drainage is preferred when the operation is performed through the vagina and no abdominal incision is made, as in the operation of vaginal hysterectomy.

Fig. 202.—Glass drainage-tube.
The glass drainage-tubes should be of various lengths—5 to 7 inches. The outer diameter should be about ⅜ or ½ inch. The lower portion of the tube is perforated with small holes over a distance of about 1½ inches. Around the upper part or neck of the tube, which protrudes from the abdomen, is placed a square of rubber dam, such as is used by dentists, about 8 by 8 inches in size. The tube passes through a hole in the center of the rubber. The tube and the rubber dam may be sterilized by boiling. The tube is usually placed in the lower angle of the abdominal incision, and the abdominal dressing is split so that it may be placed around the tube. The bandage is applied so that the four upper tails pass above the tube and the two lower tails pass below it. The opening of the tube and the rubber dam are outside of 481 the bandage. When the dressing and bandage have been applied, the opening of the tube is plugged with sterile absorbent cotton, and a handful of cotton is placed in the dam, which is then folded over and pinned. A sterile towel is placed over the dam. Some operators insert a cord of cotton or a few narrow strips of gauze to the bottom of the tube, in order to maintain a continuous capillary drain.
Cleansing or emptying the drainage-tube is a procedure which should be very carefully attended to. Strict asepsis should be observed in all the manipulations. For the first few hours the general peritoneum is exposed to danger of infection every time the tube is opened. After the first twenty-four hours, though the danger of general peritoneal infection is remote or absent, yet there is always danger of local infection of the tube-tract. Such local infection may result in a persistent sinus or other complication. A ligature near to or in contact with the tube may become infected, and the sinus will remain open until the ligature is discharged.
The tube may be cleaned by any careful nurse. The bedclothes should be drawn down to the pubis and the clothing should be drawn up, so that the abdomen is exposed. Sterile towels should be placed about the rubber dam. The hands of the nurse should be sterilized. The dam should be opened, the cotton should be removed, and the orifice of the tube exposed. The tube should be emptied with the long-nozzled syringe (Fig. 203), or with some other easily sterilized apparatus by which the fluid may be withdrawn.

Fig. 203.—Syringe for cleaning drainage-tube.
All fluid should be withdrawn from the drainage-tube. The dam should be carefully cleansed by wiping with cotton wet with the solution of bichlorid of mercury. A fresh cotton plug should be inserted in the tube, and 482 the dam should be folded and pinned over a handful of cotton. The whole should then be covered with a sterile towel.
The tube should be emptied or cleaned as often as it becomes filled. It is often necessary at first to clean it every fifteen, thirty, or sixty minutes. If free bleeding is taking place, it is most quickly arrested by frequent cleaning of the tube. Unless the nurse is experienced, the operator or assistant should watch the drainage-tube for the first hour after operation, in order to direct the nurse in regard to the required frequency of cleansing. A record should be kept of the amount of fluid withdrawn.
The intervals between cleansings are gradually increased until once every six or twelve hours becomes sufficient. It is not often necessary to keep the tube in the abdomen longer than two or three days.
The tube should be removed when the fluid discharged becomes serous in character and small in amount—about one dram every four or five hours. Before removing the tube the flannel binder should be opened and the wound should be exposed. When the glass tube is withdrawn, it is best to replace it by a small rubber tube. This may be done by inserting the rubber tube to the bottom of the glass tube, which is then withdrawn. If we were certain that the tube-tract were aseptic, the introduction of the rubber tube would be unnecessary, and we might close the lower angle of the incision immediately by suture. This procedure, however, may be followed by fluid-accumulation and the formation of abscess in the tube-tract. It is therefore safest always to use the rubber tube. The rubber tube should be withdrawn gradually, an inch or two every day, so that the tract will close from the bottom. In order to prevent the rubber tube slipping altogether into the drainage-tract, it is advisable to insert a small safety-pin through the extra-abdominal end. The end of the rubber tube should be surrounded and covered by several layers of gauze and the abdominal pad.
Gauze-drainage.—Capillary drainage with gauze is 483 sometimes more convenient than drainage with the tube. A strip, about 2 inches in width, of several layers of gauze should be carried, from the part of the pelvis to be drained, out through the lower angle of the abdominal incision. When the sutures are introduced the lower angle of the incision should not be too tightly closed, or drainage will be impeded. The extra-abdominal end of the gauze drain should be surrounded and covered by several layers of loosely-packed gauze and by the abdominal pad and binder. Sterile cotton should be tucked under the binder immediately above the pubis, and, if necessary, around the upper and lateral margins of the pad. The dressing need not be disturbed for one, two, or three days, unless the discharge has soaked through the abdominal binder.
A convenient capillary drain is made of a gauze bag containing several strips of gauze.
One objection to the gauze drain is the difficulty of removal. Lymph-processes and granulations penetrate the interstices of the gauze, and often render its removal very difficult. The surgeon fears to use too much force in attempts at withdrawal, because an adherent loop of intestine or the omentum may be pulled out of place or damaged, or the lymph-wall of the drainage-tract may become opened and expose the general peritoneum to infection. To avoid this difficulty the writer has for some time employed a drain made by surrounding the gauze bag with an ordinary rubber condom the end of which has been cut open (Fig. 204). With this arrangement the surgeon may feel certain that there are no adhesions except at the end of the drain. Such drains may be removed as easily as the glass tube. The condom may be sterilized by boiling. Gauze drains should be removed at the end of two or three days. After withdrawing the gauze it is advisable to insert a small rubber tube, for reasons that have been mentioned in considering the use of the glass drainage-tube.
The gauze drain may be used in all cases except when it is necessary to drain pus or some solid material like 484 feces. In such cases the glass tube should be employed, either alone or surrounded by a gauze pack to protect the general peritoneum.
In pelvic surgery the drain, whether glass or gauze, should, as a rule, be placed at the most dependent part of the pelvis, which is the bottom of Douglas’s pouch. It may be placed to either side of the median line in case the chief discharge is expected to take place from this position. Hemorrhage from a bleeding surface deep in the pelvis may often be controlled by the direct pressure of the end of the gauze drain placed over it.
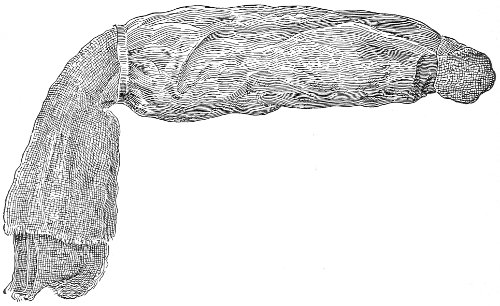
Fig. 204.—Gauze drain with rubber cover.
The drain should be introduced immediately before the abdominal sutures are tied.
Indications for Drainage.—Great diversity of practice exists among operators as to the use of drainage after celiotomy, and a decided change has taken place in regard to drainage during the past twenty years. In the early days of modern abdominal surgery drainage was used very much more than it is at present; some of the best operators used it in the majority of their cases; now a number of operators never use drainage after celiotomy, while others use it only when specially indicated. Much depends upon the individual methods of the operator. The operator who is careless in his asepsis and hemostasis 485 should use drainage oftener than he who is careful in these particulars. The advice, “When in doubt drain,” is very good; but the surgeon should strive to eliminate the element of doubt as much as possible, and to have a definite reason for all his procedures. If drainage is not necessary, it is harmful. It necessitates more frequent dressings and disturbance of the patient, and it prevents perfect closure of the abdominal incision.
The object of drainage is the removal from the peritoneum of discharges which are, or which may become, septic or dangerous. Such discharges are blood, pus, serum, cyst-contents, and ascitic fluid.
Even though the peritoneum be dry and all bleeding be arrested when the operation is completed, yet it must be remembered that a subsequent free serous exudation will take place if the peritoneum has been exposed or subjected to chemical or mechanical irritation.
Infection may take place from imperfect asepsis at the time of operation; or it may be caused by the escape into the peritoneum of septic material which existed in the abdomen before the operation; or it may occur subsequently, from the passage of septic organisms from the interior of the intestine through the intestinal wall.
The absorbing power of the healthy peritoneum is so great that a large amount of fluid (even though not absolutely sterile) may be taken up by it. Injury of the peritoneum from exposure or other irritation not only increases the amount of fluid to be absorbed, but it diminishes the power of absorption; and injury of the intestinal peritoneum or of the wall of the intestine favors the passage of septic organisms through it.
The operator should bear these facts in mind when he considers the subject of drainage.
A certain amount of absorption of blood or other sterile fluid may be trusted to the peritoneum.
It is sometimes impossible to arrest all venous oozing from raw surfaces, and the blood must be left for absorption by the peritoneum, or must be carried off by drainage 486 with the glass tube or with gauze. Drainage enables the operator to watch the amount of hemorrhage after operations, so that if excessive he may employ measures to check it. Drainage also acts as a hemostatic. The direct pressure of the gauze upon the bleeding area checks the hemorrhage, and the continual removal of blood, the promotion of dryness, and the contact of air through the glass tube have a decided hemostatic effect.
Drainage, therefore, is sometimes used not only to remove blood, but to aid in arresting hemorrhage. As the operator becomes more experienced he practises more perfect hemostasis, and learns to obliterate by buried suture, to fold in, or to cover with peritoneum raw bleeding surfaces, so that drainage as a means of hemostasis is less often required. If the operator fears that the peritoneum has become infected from imperfect asepsis at the operation, or from the escape into it of some septic material like pus, he should employ drainage, especially if he expects much subsequent serous or bloody discharge to take place.
If the intestinal wall has been extensively injured, as we sometimes find after an adherent intestine has been liberated, drainage should be employed; for septic organisms most readily pass through such an injured wall, and the damage may be so great that necrosis may take place, with the escape of intestinal contents. It must be remembered that all purulent accumulations in the abdomen and pelvis are not septic. Such accumulations were septic in the beginning, but in the majority of chronic cases the septic organisms have died and disappeared, and the pus is perfectly sterile and harmless to the peritoneum. Consequently, if an ovarian or a tubal abscess ruptures during removal, and the contents escape into the peritoneum, drainage is not necessarily required. For a period of three years the writer had in such cases immediate bacteriological examination of the pus made, and determined drainage from the result of such examination. In the majority of cases the pus was 487 sterile and drainage was not employed. It has been found, as would be expected, that the pus is most often septic in the cases of recent suppuration and in the chronic cases during an acute attack. Experience also teaches that suppurating dermoids are very likely to be septic.
It will be seen from these considerations that in determining the question of drainage much must be left to the judgment and the experience of the operator.
If an aseptic operation has been performed, and there is no intestinal lesion and hemostasis is perfect, drainage is not required. This condition of things is, of course, most often attained by the experienced operator. If the operator fears septic infection for any reason, or fears that the hemostasis is not good, he should employ drainage. At the present day the decided majority of the best operators use abdominal drainage very little.
When general peritoneal sepsis exists before the abdomen is opened, drainage is always indicated.
Vaginal Drainage.—Drainage of the peritoneum through the vagina is usually accomplished by making an opening through Douglas’s pouch into the posterior vaginal fornix. A rubber drainage-tube or a gauze drain may then be inserted. The vagina and vulva should, of course, have been thoroughly sterilized. The vagina should be lightly packed with gauze, and the vulva should be protected by a gauze and cotton dressing. As has been said, the chief objection to vaginal drainage of the peritoneum is the difficulty of sterilizing and maintaining sterile the vagina and the vulva.
The Incision of the Abdominal Wall.—The various abdominal operations of gynecology are performed through an incision in the median line. The position of the incision depends upon the condition to be treated. The incision for performing ventro-suspension of the uterus is made near to the symphysis pubis. The incision for the removal of a large cyst is made at a higher point. As a rule, the incision, about 2 or 2½ inches in 488 length, should be made about midway between the umbilicus and the pubis, and should be extended upward or downward as necessary. The incision should be as small as the operator can conveniently work through. He should not hesitate to enlarge the incision to facilitate any manipulations. The length will depend a good deal upon the thickness of the abdominal walls.
The structures that are incised are the skin, the subcutaneous fat, the parietal fascia, the linea alba or the edge of the rectus muscle, the subperitoneal fat, and the peritoneum.
If the incision is made exactly in the median line, the linea alba will be divided and the sheath of the rectus will not be opened. This is most usual in multiparous women with lax abdominal walls and widely separated recti muscles, and in cases in which the abdomen is distended by a tumor. If the sheath of the rectus is opened, the muscle will be exposed, and the linea alba should be sought on the side upon which the fascia fails to retract.
If the linea alba cannot readily be found, the incision should be carried directly through the muscle. Some operators consider it an advantage, in obtaining subsequent firm union, to expose the muscle in this way. When the subperitoneal fat is reached, it should be torn and pushed aside with the blunt closed forceps or with the fingers.
The peritoneum should be caught with forceps and drawn forward. The assistant should catch the peritoneum with a second pair of forceps at a point about ⅓ or ½ inch to the side of the first pair, and the small fold of peritoneum thus produced should be incised with the knife. As soon as the smallest opening is made in the peritoneum the air rushes in and the intestines and omentum fall back. The opening is then enlarged with the knife or scissors.
The greatest care must be exercised in those cases in which the omentum or the intestines are adherent to the 489 anterior abdominal wall. The experienced operator usually observes indications of such a condition as soon as he has passed through the linea alba. The tissues are more rigid and unyielding than normal, and the peritoneum cannot be readily picked up with the forceps. In such cases the operator should proceed very slowly, and if necessary should enlarge the outer incision and enter the peritoneum at a point above or below the area of adhesion.
Exploration of the Abdomen.—Having opened the peritoneum, the operator should insert two fingers (the middle and the index finger of the left hand) and should carefully examine the condition to be treated.
If necessary, he should retract the edges of the incision, and should place the patient in the Trendelenburg position, in order to make an ocular examination.
It is always advisable to make a preliminary investigation of this kind before proceeding with the operation. In this way the diagnosis will be corrected and complications which must be treated will be determined. It may be found that what was thought to be a cyst is in reality a uterine fibroid or perhaps a normal pregnancy; or the surgeon may discover a hopeless condition, such as extensive cancer or peritoneal papilloma, for which further operation will be useless.
Protection of the Intestines and Omentum.—During all manipulations within the abdomen the peritoneum, intestines, and omentum should be handled most gently. Injury of the peritoneum increases the danger of shock, sepsis, and intestinal adhesions. The intestines should never be allowed to protrude through the abdominal incision unless it is necessary for the performance of the operation. Such a necessity rarely, if ever, arises in gynecological operations. All the intestines may be removed from the field of operation—the pelvis—by placing the woman in the Trendelenburg position. Protrusion of intestines through the abdominal incision should be prevented by using large gauze pads or sponges. 490 It is advisable always to surround the field of operation by a wall of gauze pads. They protect the intestines and prevent the escape of fluids into the upper peritoneum. This precaution is especially desirable when the Trendelenburg position is used, to prevent fluids from the pelvis escaping into the upper abdomen. The pads should be introduced after being wrung out of warm water, and should be replaced by fresh warm pads as soon as they become saturated with fluid. If they become soiled by pus or other septic fluid, it is safest to discard them for the remainder of the operation.
Toilet of the Peritoneum.—The field of operation, and, if necessary, the general peritoneum, should always be cleaned and dried before the abdominal incision is closed. This is done by sponging and by irrigation with warm sterile water or with normal salt-solution. The sponging should be performed with great gentleness, to avoid peritoneal irritation. There are several regions in which fluids and blood-clots are most likely to collect, and which therefore demand especial inspection.
The chief of these regions is the hollow of the sacrum, or Douglas’s pouch. Fluids also collect on the anterior surface of the broad ligaments and in the renal hollows.
If but little fluid has escaped into the abdomen, and the field of operation has been confined to the pelvis, we need look for accumulations of fluid and blood only in Douglas’s pouch and in front of the broad ligaments. If the upper portion of the abdomen has been invaded, it is advisable to inspect the renal hollows. Blood-clot and fluid may be readily removed by the sponge held in the fingers or in forceps.
Irrigation of the peritoneum is not often required. It is not necessary to flood the peritoneum with water in order to wash out blood-clot, which may be removed with more accuracy by sponging. There is always danger, in general irrigation of the peritoneum, of spreading infection.
Local washing of the pelvis is sometimes advisable if 491 the operator fears that the field of operation has been infected by the escape of septic material. Such a condition may exist in operations for tubal or ovarian abscess. The upper peritoneum should be first shut off from the pelvic cavity with a wall of gauze sponges. This may be readily done while the patient is in the Trendelenburg position. She should then be placed in the horizontal position, while the operator, with the left hand pressed against the wall of pads, prevents the intestines entering the pelvis. The abdominal incision should be held open with retractors, and the sterile irrigating fluid should be poured in from a flask or a pitcher. The temperature of the fluid should be 100°-115° F. The fluid may be removed by sponging, and washing may be repeated as often as necessary.
In septic cases the writer has frequently performed such local washing with a bichloride solution (1:2000 or 1:4000), followed by irrigation with plain water.
If the patient is horizontal and the gauze pads be properly placed, there is no danger of any of the fluid entering the upper peritoneal cavity.
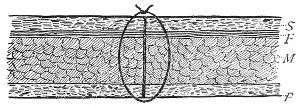
Fig. 205.—The mass-suture for closing the abdominal incision: S, skin; F, fascia; M, muscle; P, peritoneum.
Closing the Abdominal Incision.—A variety of methods have been introduced for closing the abdominal incision. The simplest method, that is applicable to all cases, is the interrupted mass-suture, or the “through-and-through” suture. This suture passes through all the structures of the abdominal wall (Fig. 205). Some operators advise passing the suture to, but not through, the peritoneum. The writer includes the edge of the peritoneum in the suture. These sutures should be placed 492 two or three to the inch, according to the thickness of the abdominal wall.
Care should be taken to include all the structures in the embrace of the suture. A carelessly applied suture sometimes fails to include the retracted fascia and muscle. The needle should first be directed outward and then inward as it passes through the abdominal wall. It should not pass directly through, parallel to the sagittal plane of the incision. Thus when the suture is tied it forms approximately a circle, and the structures included in it are brought into a plane of apposition.
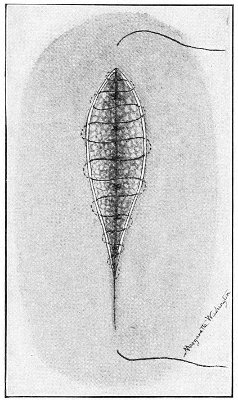
Fig. 206.—The subcuticular or intra-cutaneous suture. The fascia has been united by an interrupted suture.
A long straight needle with a spear-point is convenient for introducing the mass-suture. A gauze sponge should be placed beneath the incision as the sutures are introduced, to prevent injury of the intestines and the escape of blood into the peritoneum. When the pad is removed, the omentum, if readily found, should be drawn down behind the incision. Before each suture is secured the sides of the incision should be drawn forward by traction on the ends of the suture, to ensure accurate apposition upon the posterior or peritoneal aspect. If this precaution is not taken, in a thick or rigid abdominal wall the cutaneous aspect of the incision may be brought into accurate apposition, while a gap will exist between the more posterior structures. Such imperfect apposition is a frequent cause of ventral hernia. The mass-sutures should not be removed for two weeks. The early removal of sterile sutures is of no advantage whatever, and 493 may cause ventral hernia. The writer often leaves them in for three weeks.
After the sutures are removed the incision should be strapped with adhesive plaster.
The application of a buried suture of catgut or of silver wire, passed through the muscle and fascia, is a useful addition to the mass-suture and an additional preventive of hernia.
Various methods of uniting the tissues by sutures in separate layers are used. A very good method is to close the peritoneum by a continuous suture of fine silk, then to unite the muscle and fascia by a continuous suture of catgut, and finally to close the cutaneous edge with an interrupted or a continuous suture of silkworm gut or silk. The subcuticular or the intra-cutaneous suture (Fig. 206) is very convenient for this purpose.
If the abdominal wall be fat, it is advisable to introduce a second catgut suture through the subcutaneous fat. When the structures are united in layers, a hematoma sometimes forms between two planes of suture, and, if not absorbed, the anterior portion of the wound may break down. This accident, which is caused by hemorrhage after the sutures are secured, may be prevented by employing, in addition to the usual dressing, a compress of gauze placed over the incision. 494
The after-treatment of celiotomy is usually very simple. A special nurse is required for the first three days. The patient should lie upon her back for the first two or three days; after this she may be moved partly upon either side, and a pillow may be placed behind her for support.
The head may be supported by one or two pillows. Much comfort is experienced by raising the knees over pillows. The patient often complains bitterly of backache, which may be relieved by slipping a folded sheet or towel under the small of the back.
Thirst is always present after celiotomy, and is usually the symptom of which the patient complains the most. There is much diversity of practice in regard to the administration of water after celiotomy. The writer allows no water during the first twenty-four hours. During this time the lips and mouth are frequently moistened with a cloth wet in cold water or wrapped about a piece of ice. At the end of twenty-four hours small quantities of hot water or cold soda-water (1 dram) are given every fifteen minutes or half hour, and gradually increased as it is found to be retained by the stomach. Hot water relieves thirst as well, and is not so likely to cause vomiting, as cold water.
The chief objection to the early administration of water after celiotomy is that it may cause vomiting. Some operators avoid this by administering the water by the rectum.
Another reason, more or less theoretical, for withholding water is that the absorbing power of the peritoneum 495 is greatest when the tissues of the body contain a deficient amount of water.
Pain after celiotomy seems to bear no relation whatever to the amount of traumatism that has been inflicted. More discomfort may be experienced after ventro-suspension of the uterus than after a hysterectomy. In operations upon the generative organs the chief seat of pain is in the region of the sacrum. Pain is also felt in the ovarian region and in the abdominal incision. The pain begins to abate after the first fifteen or twenty hours. Opium should not be administered unless it is absolutely necessary to allay nervous excitement in a cowardly woman. In such a case a small dose (gr. ⅙) of morphine may be administered hypodermically.
The writer rarely finds it necessary to administer an anodyne. Most patients are able to endure the pain if they are properly encouraged by the physician and the nurse.
There are several objections to the administration of opium. It increases the thirst and it diminishes the functional activity of the gastro-intestinal tract. It retards the passage of flatus by the rectum and causes tympanites, and it increases the difficulty of moving the bowels. It obscures and delays the recognition of symptoms that may demand immediate treatment. The patient who has had no opium is more comfortable at the end of three or four days after celiotomy than one to whom it has been given.
The patient should be encouraged to pass water voluntarily. The application of hot moist cloths to the external genitals sometimes facilitates urination. In many cases the use of the catheter is never necessary. If the urine is not voided about every eight hours, it should be drawn with the catheter. Catheterization should be done with strict attention to asepsis. The former frequency of cystitis from the improper use of the catheter has already been referred to. Catheterization should never be performed under any circumstances by the aid of the 496 tactile sense alone. The nurse should always see what she is doing. The catheter—metal, glass, or preferably soft rubber—should be sterilized by boiling, and should be preserved in a 1:20 solution of carbolic acid.
The catheter may be lubricated with sterilized oil or glycerin. The labia should be separated, and the vestibule and the external meatus should be wiped off with a solution of bichloride of mercury (1:2000).
After the catheter has been used once it should be thoroughly cleansed, inside and out, and sterilized by boiling before being replaced in the carbolic solution.
The secretion of urine is always diminished for a few days after celiotomy, probably on account of the restricted ingestion of fluids. The writer has found the average secretion in 111 cases of celiotomy on women to be, during the first twenty-four hours, 13.4 ounces; during the second twenty-four hours, 14.6 ounces; during the third twenty-four hours, 19.6 ounces. In considering these numbers it should be remembered that the gynecological patient passes, before operation, a daily amount of urine much less than that passed by the average healthy woman.
Food is usually first administered at the end of forty-eight hours. If the patient be feeble, nutriment may be given by the mouth or the rectum before this time. The patient may have any easily digested food that she wishes, such as buttermilk, soup, beef-tea, milk or milk and lime-water, soft-boiled egg, etc. The food should be given frequently in small quantities. Buttermilk is one of the best foods with which to begin. It gratifies thirst and is more readily digested than milk. Half an ounce to an ounce may be given every hour until the retentive power of the stomach is determined.
The bowels should be moved at the end of forty-eight or seventy-two hours. If the patient is uncomfortable and is unable to pass flatus freely, or if there is any abdominal distention, the purgative should be administered at the earlier time (forty-eight hours). If she is comfortable 497 and passes flatus easily, she may wait for three days. Purgation is most readily produced with Rochelle salts, given, in doses of ½ dram in about 3 or 4 ounces of water or soda-water, every hour. After the patient has taken five or six doses she usually feels the inclination to have a movement. If she is unable to accomplish this, she may be assisted with a rectal injection of 1 pint of soap and water and 2 drams of turpentine. The bowels should be moved at least once in every forty-eight hours during the remainder of the convalescence.
Sometimes the bowels are more difficult to move, and it is necessary to repeat the rectal injection at intervals of two or three hours until a good movement is produced. A compound enema composed of Epsom salts ℥j, glycerin ℥j, turpentine ℥iss, water ℥viij, injected high in the bowel through a rectal tube, may be effective. If the Rochelle salts are not retained, or if they fail to act, 1 grain of calomel may be administered every hour for five or six hours.
If the patient does well, vomiting does not often occur after the first twenty-four hours, when the effects of the ether have passed off. When vomiting occurs later than this, it is usually accompanied by abdominal distention and general abdominal pain. It is then an alarming symptom, and may indicate the onset of intestinal paralysis and general peritonitis.
This group of symptoms (vomiting, general abdominal pain, and distention) demands immediate treatment. A hot mustard plaster or a turpentine stupe should be placed over the epigastrium, and an enema of 1 pint of water and ½ ounce of turpentine should be administered, and should be repeated every three or four hours until a fecal movement occurs and flatus is freely discharged. At the same time Rochelle salts should be administered, or, if there is persistent vomiting, 1-grain doses of calomel. The escape of flatus may be assisted by inserting a rectal tube. In case of moderate distention or of intestinal pain from inability to pass flatus, the insertion in the 498 anus of the ordinary rectal nozzle of the syringe will usually give relief. If this is not sufficient, the long rectal tube or a large rubber catheter should be introduced. It should be well greased and passed slowly into the rectum for a distance of 10 or 12 inches.
The patient is sometimes able to pass flatus when upon her side, though she may not be able to do so upon her back. Inability to pass flatus is not necessarily a sign of peritonitis or intestinal paralysis. It may be caused by the unaccustomed position, or pain or nervousness may prevent the woman relaxing the sphincter ani.
If the vomiting persists and becomes bilious, relief is sometimes obtained by thoroughly washing out the stomach through the stomach-tube.
The internal administration of medicines—except the purgatives already mentioned—is of little use in vomiting of this character.
The pulse after celiotomy usually remains below 100. It often, however, reaches 115 or 120, and sometimes higher, in patients who have a favorable convalescence. A rapid pulse unaccompanied by unfavorable abdominal symptoms often indicates some heart-trouble.
A pulse of over 120 accompanied by abdominal distention and vomiting should always excite alarm.
Strychnine and digitalis, administered hypodermically, are the most useful medicines for strengthening the heart and diminishing the rapidity of the pulse. They should be given in large doses—1/20 of a grain of strychnine every three or four hours, and 10 minims of tincture of digitalis at similar intervals.
Hypodermic injections of strychnine are most useful for shock after celiotomy. This drug may be exhibited until the physiological action—twitching or jerking of the muscles—is observed. The writer has administered between 1 and 2 grains during the first twenty-four hours after celiotomy, with recovery.
The temperature after celiotomy runs no regular course. It usually remains below 102° F. A greater elevation of 499 temperature than this may occur during a favorable convalescence; and; on the other hand, a fatal termination may take place when the temperature remains lower. The maximum temperature is usually observed about the second or third day.
The temperature often rises on account of very trivial causes. It may go up one or two degrees if the patient should become constipated, and will drop as soon as a free fecal movement has taken place.
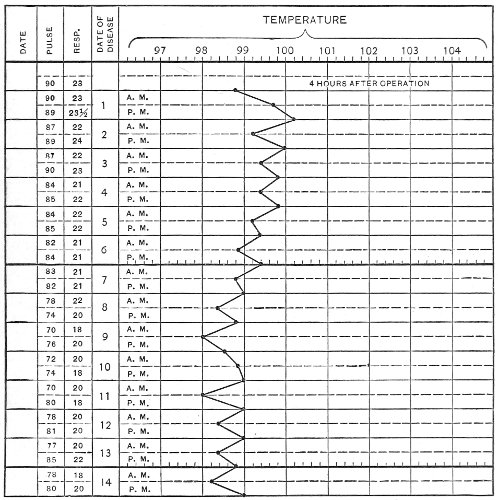
Fig. 207.—Composite temperature-chart of a series of 150 successful cases of celiotomy: average temperatures, pulses, and respirations for two weeks after operation.
The comfort of the patient is much increased by sponging the arms and legs with tepid water. The nurse 500 should be instructed to sponge the patient in this way whenever the temperature reaches 102° F.
The patient should maintain the recumbent posture for three weeks after celiotomy. She may then sit up in bed for two or three days, and if then sufficiently strong, she may leave the bed.
Too great haste in getting up may result in ventral hernia. The incision should be strapped with adhesive plaster for five or six weeks after operation, and the woman should wear some simple form of abdominal binder for the following six months, or for a year if the incision be large. She should be warned against resuming hard work, involving lifting or other abdominal strain, for several months after operation. She should be told of the possibility of ventral hernia, and advised to return immediately for treatment should this condition appear.
The usual causes of death after celiotomy are peritonitis and hemorrhage. The frequency of hemorrhage as a cause of death is often overlooked. The writer feels confident that many deaths which, without post-mortem examination, are attributed to peritonitis, are really caused by hemorrhage. Without doubt, peritonitis and hemorrhage often occur together; the blood that escapes into the peritoneal cavity may be too great in amount for absorption, and may become septic. The source of the hemorrhage is usually a vessel of the pedicle that escapes from the embrace of an imperfectly applied ligature. This accident should not happen if the operator is careful to see that hemostasis is perfect before the abdomen is closed. Bloody oozing from a surface of adhesion is not sufficient to cause death, and may be removed by drainage; the fatal hemorrhage comes from an arterial vessel that has slipped from its ligature. All ligatured vessels should be finally inspected immediately before the abdomen is closed. If a stump is not perfectly dry, a reinforcing ligature should be applied. Care in this particular will save much subsequent anxiety. If the operator knows that his ligatures have been securely applied, he 501 can exclude the possibility of hemorrhage in case alarming symptoms should arise.
If the symptoms of the patient after celiotomy indicate hemorrhage, the abdomen must be reopened and the bleeding vessels secured.
The causes of peritonitis after celiotomy have already been discussed.
The common symptoms are rapid pulse, abdominal distention and pain with inability to pass flatus or feces, and vomiting, which may finally become stercoraceous. The temperature is usually elevated, though it may remain normal or subnormal. Auscultation of the abdomen reveals total absence of all peristaltic sounds. If these symptoms are not arrested by the use of purgatives, turpentine enemata, and the rectal tube, it is probable that the result will be fatal. Death usually occurs on the third day.
The mortality after celiotomy depends upon the condition to be treated, the skill of the operator, and the environment of the operation. Some operations, like ventro-suspension of the uterus, are attended by no mortality. The average mortality after celiotomy for large numbers of gynecological cases of all kinds, in the hands of experienced operators with good operative surroundings, is about 5 per cent. 502
A thorough knowledge of the anatomical relations of the various structures in the pelvis is essential for the performance of the various operations upon the uterus and its appendages.
A detailed description of such anatomical relations is out of place here. It is especially important to study the distribution of the arterial supply and the relations of the ureters. Fig. 208 will refresh the memory upon these points.
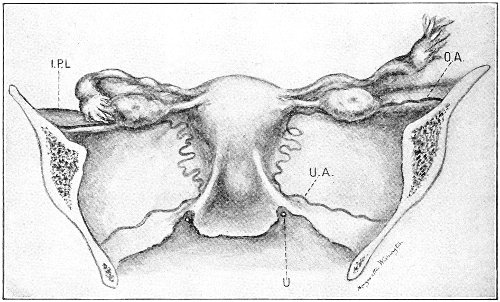
Fig. 208.—Posterior view of the uterus, the tubes and ovaries, and the broad ligaments: I.P.L., infundibulo-pelvic ligament; O.A., ovarian artery; U.A., uterine artery; U., ureter. The utero-sacral ligaments are seen on each side of the posterior aspect of the cervix.
The ovarian artery, which corresponds to the spermatic in the male, is a branch of the abdominal aorta. It runs 503 tortuously between the layers of the upper part of the broad ligament, from the pelvic wall to the upper angle of the uterus. Before reaching the uterus it divides into two branches. The upper branch supplies the fundus uteri; the lower branch anastomoses at the side of the uterus with the uterine artery.
During its course in the broad ligament the ovarian artery gives off branches to the ampulla and the isthmus of the Fallopian tube, to the ovary, and to the round ligament.
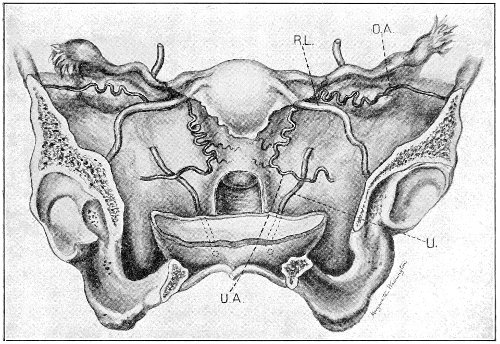
Fig. 209.—Anterior view of the uterus, the tubes and ovaries, and the broad ligaments. The upper part of the bladder, the anterior wall of the vagina, and the peritoneum on the anterior aspect of the broad ligaments have been removed. U., ureter; U.A., uterine artery; O.A. ovarian artery; R.L., round ligament.
The uterine artery arises from the anterior division of the internal iliac, and runs downward and inward toward the cervix uteri. The vessel is tortuous, and is loosely supported by the cellular tissue at the base of the broad ligament. The lowest point which it reaches is on a level with the external os uteri, and at this point it crosses the ureter. 504
At about this point it gives off the circular artery of the cervix, which anastomoses with its fellow of the opposite side. The uterine artery then passes upward, and reaches the uterus near the level of the internal os. It passes along the side of the uterus in a very tortuous manner, and anastomoses with the ovarian artery.
The vaginal arteries usually arise from the anterior division of the internal iliac artery. They sometimes arise from the uterine or middle hemorrhoidal artery.
The ureter passes behind and beneath the uterine artery. The uterine artery crosses the ureter at about the level of the external os uteri. At this point the ureter is ⅗ of an inch distant from the cervix. The distance between the ureter and the artery at the point of crossing is about ⅖ of an inch. It is important to remember these relations in applying a ligature to the uterine artery.
It must not be forgotten that the anatomical relations are altered by any displacement of the uterus from its normal position. Such displacement occurs in disease and when the uterus is dragged upward or downward during operation.
In conditions, such as cancer, which are accompanied by hypertrophy of the cervix, the distance between the ureter and the cervix is much diminished.
Removal of the Uterine Appendages (Salpingo-oöphorectomy).—This operation is performed by ligaturing the ovarian artery in its course through the infundibulo-pelvic ligament and at the uterine cornu, and then excising the Fallopian tube and the ovary.
The peritoneum is opened, and the index and middle fingers of the left hand are introduced into the abdomen. If necessary, the omentum is swept upward out of the pelvis. The fundus uteri is sought, and the fingers, with the palmar surface directed downward, are passed over the posterior face of the uterus, and then outward over the posterior aspect of the broad ligament. The ovary and tube are palpated, and are lifted forward upon the palmar aspect of the two fingers or between the fingers, 505 perhaps with the subsequent assistance of the thumb, into the abdominal incision. The infundibulo-pelvic ligament is exposed, and is rendered tense by the pressure of the fingers behind it. It will be observed that the upper edge of the ligament is thick, while there is a thin, sometimes transparent, area below the free edge. The vessels run in the upper edge of the ligament, and a ligature passed through the thin area will secure them (Fig. 210).
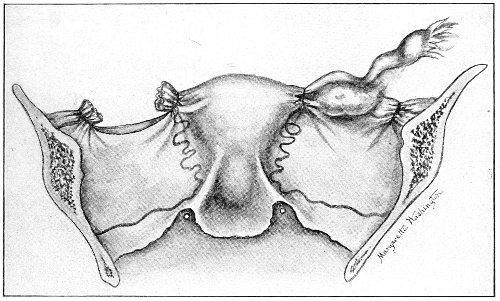
Fig. 210.—Salpingo-oöphorectomy. On the right side ligatures have been placed about the ovarian artery, at the uterine horn, and at the pelvic wall. On the left side the tube and ovary have been excised between such ligatures. If bleeding takes place from the broad ligament, the anterior and posterior peritoneal aspects may be united by suture.
The heavy silk carried in the pedicle-needle should be used. The ligature should be placed sufficiently near the pelvic wall to permit complete excision of the tube and ovary without cutting too close to the ligature. The broad ligament should then be transfixed by a second ligature at a point somewhat to the inside of the first. The second ligature should embrace the ovarian ligament, the isthmus of the tube, and the uterine end of the ovarian artery. This ligature should be placed close to the uterine cornu, in order to permit complete excision of the ovary. 506
The Fallopian tube, the ovary, and the mesosalpinx are then cut away with the scissors. There is usually no bleeding whatever from the unligatured portion of the broad ligament between the two ligatures. The stumps should be carefully inspected, and any bleeding point in the intervening portion of the broad ligament should be picked up and secured by fine ligature; or the peritoneal edges may be united by suture.
This method of operating is in accord with the best surgical principles.
The vessels are secured in their course by ligatures which embrace a minimum amount of surrounding tissue. In the early days of modern abdominal surgery, the operation usually advised was performed with the Tait knot (Fig. 211) or the link-ligature (Fig. 212).
Fig. 211.—The Tait knot. |

Fig. 212.—The link-ligature. |
The ovary and the tube are drawn into the abdominal incision, and the pedicle formed by the broad ligament is transfixed with the pedicle-needle carrying a double ligature.
The loop of the ligature is passed over the tube and ovary and the Tait knot is tied, or the ligature is cut and each half of the pedicle is separately secured, the ligature being crossed or linked in the middle of the stump, to prevent separation.
The operators who apply the ligature in this way do so because they fear hemorrhage if every portion of the broad ligament is not secured.
This fear is unfounded. The objections to this form of ligature, the Tait or the link-ligature, may be given by the following quotation from a former paper by the writer.4 507
“The objections to these ligatures are: The liability to slip; the difficulty or impossibility in some cases of removing all the ovary and tube; the fact that the broad ligament is puckered up and made more tense than normal, and may for this reason cause subsequent pain and discomfort; an unnecessary amount of tissue is strangulated.
“Most operators have seen cases, either in their own experience or in the experience of others, in which the ligature has slipped from the pedicle, either during the operation or some days afterward. I think that this accident, usually unrecognized, is a very common cause of death after oöphorectomy. Tait speaks of a certain number of cases in his own experience in which a hematoma occurred in the broad ligament some hours or days after operation. He says, ‘I cannot form any exact estimate of how many cases of these operative hematoceles I have seen, but it certainly is not less than 50, and is more likely to be 70 or 80.’
“It seems probable that this accident is due to the retraction or slipping of the artery from the embrace of the ligature, while the remaining mass of tissue which forms the pedicle is still retained, and the hemorrhage, therefore, is confined to the broad ligament. I have seen this accident happen before the abdomen had been closed, and have sought for and ligated separately the retracted vessel.
“Slipping of the ligature is due to the form of the mass of tissue which is ligated. The broad ligament is drawn up into a more or less conical shape, all parts converging toward the ligature, and the ligature is really placed at the apex of a cone from which it may readily slip; and the elastic artery, tied when upon the stretch, tends to retract and escape from the embrace of the ligature.
“The second objection is the difficulty or impossibility of removing all the ovary and tube. If the broad ligament is tense, as it often is in single women, or if it is 508 thickened from inflammatory deposit, it is sometimes impossible to bring the tube and ovary through the abdominal incision and to obtain a pedicle which may be ligated so that we may with safety remove all of the ovary. And it is in just such cases that it is usually most desirable that all ovarian tissue should be removed.
“The third objection—the puckering and tension of the broad ligament—may be of less importance than those just considered. However, it seems probable that some of the pain which women suffer after oöphorectomy is due to the traction and counter-traction exerted by different parts of the broad ligament upon a sensitive cicatrix. The broad ligament is pulled up from different directions and converges to the cicatrix, which becomes the point from which the lines of traction radiate.
“It was thought that in case of retroversion this tension of the broad ligament would maintain the uterus in place, the ligaments acting as guys. This, however, is not true. Repeated secondary operations have shown that the uterus has fallen back again to extreme retroversion, notwithstanding such methods of ligature of the broad ligaments.
“The fourth objection is one which appeals to our surgical sense. It is always better surgery to ligate the vessel alone than to include with it a mass of surrounding tissue.”
If the isthmus of the Fallopian tube is diseased, as in some cases of pyosalpinx, so that it is necessary to exsect the tube from the uterine cornu, the second ligature may be passed immediately beneath the tube, including the ovarian ligament and the ovarian artery, but not including the tube; the tube may then be cut out by a wedge-shaped incision in the horn of the uterus. The uterine wound should be closed by interrupted suture (Fig. 212, A). In such cases, however, if the tubal disease is bilateral, it is best to remove the uterus as well as the appendages.
It is not necessary to place both ligatures before cutting away the ovary and tube. The first ligature may be placed about the proximal portion of the ovarian 509 510 artery, and then the infundibulo-pelvic ligament may be cut, bleeding from the distal end being controlled with forceps. This will enable the operator readily to bring the ovary and tube through the incision and to ligate the ovarian artery at the uterine cornu.
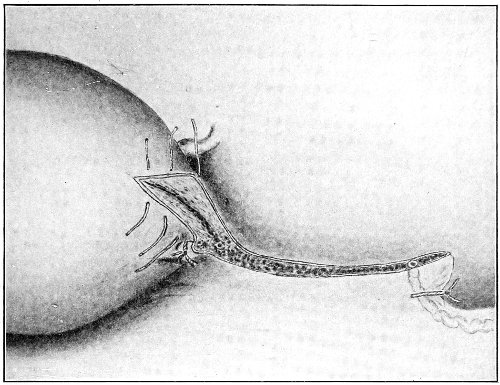
Fig. 212, A.—Position of ligatures and sutures in exsection of the tube.
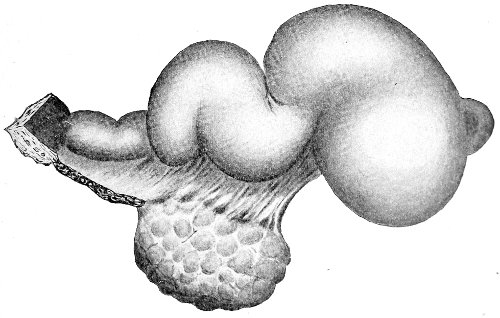
Fig. 212, B.—Pyosalpinx which has been exsected from the uterine cornu.
If adhesions exist, they should be broken with the fingers, or the patient should be placed in the Trendelenburg position and the adhesions should be divided with scissors. The tube and ovary are sometimes completely imbedded in adhesions, and it is necessary to shell them out by careful work with the fingers. The adhesions may be so dense and the anatomical relations so altered that it is difficult or impossible to determine what is ovary and what is tube until the mass is brought into the abdominal incision. In these cases the experienced operator may work by the sense of touch alone. The inexperienced operator had better expose the parts and obtain the assistance of visual examination.
The fundus uteri can usually be determined, and will form a valuable landmark. The enucleation is most easily performed with the fingers. The index and middle fingers, with the palmar surfaces turned downward, should be passed outward from the posterior aspect of the uterus, and should seek a plane along which the structures most readily separate. As a rule, adhesions give way more easily than the tissues of normal structures. Adhesions should not be roughly torn: they should be pushed away from the posterior aspect of the ovary and broad ligament.
The adhesions between the ovary and the broad ligament must be broken by pressure with the fingers before the ovary can readily be brought into the abdominal incision.
After all other adhesions have been relieved it is often found that the ovary still lies low in the pelvis, glued to the posterior aspect of the broad ligament. It should not be dragged, in this condition, into the incision, or the broad ligament may be badly lacerated. It should 511 be peeled off from the broad ligament and rolled up to the incision.
After the structures have been carefully examined and the anatomical relations determined the ligatures should be placed and the tube and ovary cut away. The bleeding from the pelvic adhesions is usually arrested or much diminished as soon as the ovarian artery is ligated. It is best, therefore, to waste no time in attempts to arrest moderate hemorrhage until the appendages have been removed. The pelvis should then be inspected and any bleeding points secured. Omental adhesions should be ligated, if necessary, as they are divided.
If there is a general oozing from the bed of adhesions that cannot be controlled by ligature, one or two gauze pads should be pressed over the region and retained there until the abdominal sutures have been placed. If the bleeding continues notwithstanding such sponge-pressure, it may be necessary to employ drainage. The bleeding may always be controlled by the pressure of the end of the gauze drain placed directly over the raw surface.
If the operator is anxious to arrest menstruation, he must be certain to remove all ovarian tissue and the Fallopian tubes at the uterine cornua. Sometimes, after an adherent ovary has been enucleated, part of the ovarian stroma remains glued to the pelvic wall, the posterior face of the broad ligament, or some other structure. These portions of ovary should be carefully picked off with the forceps. If the operator doubts the complete removal of all ovarian tissue, he should make a note to this effect in the history of the case. Were this always done, the existence of a supernumerary ovary would not be so often assumed.
The directions that have been given here apply to the removal of tubal tumors and small cystic and solid tumors of the ovary. When the ovary is removed there is but little, if any, advantage in leaving the corresponding Fallopian tube in case the tube on the opposite side is healthy. 512
If the patient is anxious for children, the operator should remember that conception is possible with one tube and one ovary, though they be on opposite sides. If an ovarian tumor is removed independently of the corresponding Fallopian tube, the pedicle of the ovary should be transfixed and ligatured in two or more masses.
Removal of an Ovarian Cyst.—The removal of a large ovarian cyst may be facilitated by preliminary tapping as soon as the peritoneum is opened, and withdrawal of the fluid contents. As a general rule, this procedure is advisable if the cyst is too large to be removed through a 3- or 4-inch incision. If, however, the operator should suspect the contents of the cyst to be septic, it is safest to enlarge the incision and to remove the tumor intact, thus avoiding infection of the peritoneum. This advice is especially applicable to dermoid cysts. The contents of such cysts are very often septic. They are thick, and contain a large amount of solid material which passes with difficulty through the trocar. The walls of the cyst are friable and easily torn, so that the puncture-wound of the trocar becomes enlarged and the cyst-contents escape around it; and, finally, the contents of a dermoid are very difficult to remove from the peritoneum.
The dermoid character of a cyst may be suspected from the dull appearance of the walls and the putty-like feeling upon palpation. They are usually of small size, and may be removed bodily through an incision of moderate extent.
Every tumor should be carefully examined before the trocar is plunged into it. The operator should make certain by palpation that the tumor is cystic. The trocar has been thrust into the pregnant uterus, and frequently into a fibroid tumor. In the case of a fibroid profuse hemorrhage may occur from such an accident. The hemorrhage may usually be controlled by forcing a small sponge or gauze pack into the puncture wound. Before tapping the cyst the operator should pass his hand around it and determine the position and character of adhesions. 513
Small cysts about the size of a child’s head may be tapped with the small trocar. The larger instrument is used in cysts of greater size.
In a multilocular cyst the largest loculus should be tapped first. Sponges should be placed in the abdomen around the point selected for puncture. An incision about half an inch in length should be made through the outer coat of the cyst, and the trocar should then be introduced. As the fluid escapes through the trocar and the rubber tube into a vessel at the side of the table, and as the cyst becomes flaccid, the wall of the cyst near the trocar should be seized with large forceps. As the tumor diminishes in size it should be dragged through the abdominal incision. This procedure should not be done quickly or roughly, or adherent intestines may be torn, and bleeding from omental adhesions may escape detection.
As the cyst is drawn out the surface should be examined and adhesions should be separated, and ligatured, if necessary, as they appear. Omental adhesions usually require ligature. The bleeding from omental vessels is often profuse and is not arrested spontaneously. An adherent omentum should be ligatured with medium-sized silk in small sections, not in one mass, before it is cut away from the tumor.
The intestine is sometimes so adherent to the surface of the tumor that it cannot be separated without serious danger to the intestinal wall. In such a case it is best to cut out the adherent portion of the outer wall of the tumor and leave it glued to the intestine. If there is bleeding from the raw surface, it may be checked by folding in the bleeding area with silk suture.
While the operator is dealing with the adhesions the assistant should see that the opening in the cyst is kept in a dependent position and that cyst-contents do not escape into the abdomen. This precaution should always be taken, though it is especially important in the cases of septic and papillomatous cysts. 514
When the pedicle of the cyst is exposed, it should be ligatured as already advised. If the stump of the pedicle is very broad, it may be folded in or covered with peritoneum to prevent intestinal adhesions to it.
The other ovary should always be examined before closing the abdomen.
Operation for the Removal of Intra-ligamentous Cysts.—Intra-ligamentous cysts grow between the folds of the broad ligament. Any oöphoritic tumor may be intra-ligamentous, though the condition is most usually found in cysts of the paroöphoron and the parovarium.
The intra-ligamentous cyst may drag out the broad ligament so that a pedicle may be formed, and the tumor may be removed by the methods already described.
In other cases, however, the cyst is strictly sessile. It lies between the layers of the broad ligament, deep in the pelvis, or perhaps it may have migrated to some other part of the abdomen behind the peritoneum.
The removal of such tumors requires accurate anatomical knowledge of the region in which the growth is situated.
It is necessary to incise the peritoneal covering of the tumor and to enucleate it from its bed. The peritoneum should be incised in the position in which there are fewest blood-vessels. Thus, if the tumor has migrated between the layers of the mesocolon, the incision should be made through the outer peritoneal layer.
Intra-ligamentous cysts often have no pedicular attachments whatever, and may be enucleated without the application of ligature. In other cases a distinct vascular pedicle is found after the peritoneal investment has been opened and its adhesions to the cyst-wall have been separated.
The relations of an intra-ligamentous cyst should be carefully examined before the surgeon proceeds with the operation, and such a cyst should not be mistaken for an extra-ligamentous cyst that has become adherent.
If the tumor is situated between the layers of the broad 515 ligament, it is advisable, as a preliminary step, to ligate the ovarian artery in the infundibulo-pelvic ligament and at the cornu of the uterus. This may usually be readily done; much subsequent bleeding will be prevented by it.
The peritoneum is then incised at the most convenient point over the surface of the tumor, and the surgeon, with the fingers, knife-handle, or closed blunt scissors, proceeds with the enucleation. If inflammatory adhesions have not taken place, enucleation is usually easy. Bleeding vessels should be secured by forceps as they appear, and should be ligated, if necessary, after the cyst is removed.
If a pedicle or fleshy adhesion is met, it should be ligated before division.
During the enucleation the surgeon should follow closely the surface of the tumor. When he has reached a point deep in the pelvis he should be especially careful to avoid injury of the large vessels and the ureter. If the cyst is difficult of removal in this region, it may be advisable to cut out a portion of the cyst-wall and leave it.
Preliminary tapping of intra-ligamentous cysts is not often necessary. They are usually of moderate size, and enucleation may be most readily performed if the cyst is tense.
Sometimes large cysts are but partly intra-ligamentous: the greater portion is free, while the base is included between the layers of the broad ligament. In such cases it is best to tap the cyst and then to enucleate the base as already described.
In other cases the process of enucleation may be facilitated and rendered safe by incising the cyst-wall and introducing two fingers into the cavity to act as guides in separating the cyst from structures deep in the pelvis.
After the cyst has been removed and bleeding points have been secured by ligature, the raw surface, or the bed of the tumor, may be obliterated by bringing the sides into apposition by layers of buried fine silk sutures and by closing with suture the incision in the peritoneum. 516 These raw surfaces often contract very much by the falling together of the sides after the tumor has been removed.
If bleeding from the bed of the tumor cannot be thoroughly arrested, it is unsafe to close the incision in the peritoneum, for a hematoma will form and will cause subsequent trouble. In such a case the gauze drain should be introduced into the bed of the tumor, perhaps after partial closure of the peritoneal incision. Or if the bleeding be very profuse, the edges of the incision in the broad ligament should be sutured to the lower angle of the abdominal wound, and the cavity should be packed with gauze.
The sutures that attach the broad ligament to the abdominal incision may be passed through the whole thickness of the abdominal wall, or through only the fascia, muscle, and peritoneum. The ends of the sutures should be left long to facilitate removal.
In the removal of a cyst of the parovarium by enucleation, the tube and ovary should not be sacrificed unless they are diseased. Small cysts of the parovarium which develop between the layers of the mesosalpinx may very easily be removed by simple incision of the peritoneal capsule and enucleation of the cyst, without injury to the tube and ovary.
Marsupialization of the Cyst.—In rare cases a cyst is found to be so firmly and generally adherent to surrounding structures that its removal is impossible. It is then necessary to practise marsupialization.
The cyst should be evacuated with the trocar, which is introduced at a point which can be readily brought to the abdominal incision. Vegetations, etc. should be removed from the interior of the cyst with the fingers. The opening in the cyst should then be attached to the lower angle of the abdominal incision by interrupted sutures of strong silk that pass through the whole thickness of the abdominal wall and of the cyst-wall. The sutures should be placed close together, and the ends should be 517 left long to facilitate removal. The upper portion of the abdominal incision should be closed with interrupted sutures.
A large double drainage-tube of rubber should be introduced into the cyst, and strips of gauze should be packed around the tube.
The subsequent treatment consists of frequent washing of the interior of the cyst. The sutures in the cyst-wall should be removed at the end of two weeks.
Though marsupialization frequently results in cure, yet it should never be practised unless it is absolutely necessary. It exposes the patient to the dangers of prolonged suppuration and persistent fistula. Malignant degeneration has occurred in the wound. Papilloma may extend to the peritoneum. The procedure is of but little use in the case of multilocular tumors, as all the loculi cannot be evacuated.
The uterus may be removed through an abdominal incision (abdominal hysterectomy), or it may be removed through the vagina (vaginal hysterectomy). A combination of the two methods of operating is sometimes employed.
In many conditions it is not necessary to remove the cervix. Partial hysterectomy or supra-vaginal amputation of the uterus at some convenient point of the cervix may be performed.
Such supra-vaginal amputation of the uterus may be done in nearly all operations that are not performed for malignant disease. In sarcoma or cancer the whole uterus should be removed at the vaginal junction, and, if necessary, the upper portion of the vagina should be excised.
In the case of fibroid tumor and in non-malignant disease of the body of the uterus supra-vaginal amputation is sufficient. Supra-vaginal amputation is an easier and 518 safer operation than complete hysterectomy. Abdominal hysterectomy is most easily performed with the patient in the Trendelenburg position.
Supra-vaginal Amputation of the Uterus.—After the abdomen has been opened, the ovarian artery should be ligated in the infundibulo-pelvic ligament, as in the operation of salpingo-oöphorectomy. A second ligature, or forceps, should then be placed upon the ovarian artery at the uterine cornu.
The round ligament should then be ligatured with medium-sized silk at a point situated about an inch from the uterus. Similar ligatures should then be placed about the ovarian artery and the round ligament on the opposite side.
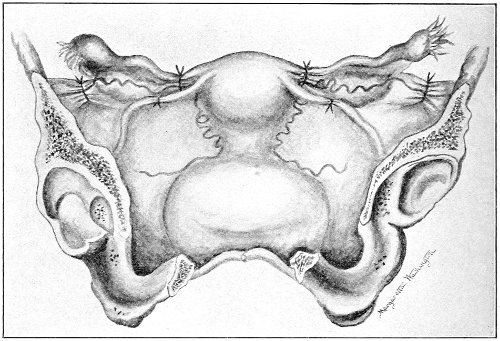
Fig. 213.—Supra-vaginal amputation of the uterus, first step: ligatures have been placed on the ovarian arteries and the round ligament.
The infundibulo-pelvic ligament immediately outside of the abdominal ostium of the tube, the round ligament between the ligature and the cornu, and the broad ligament as far as the uterus should then be divided with scissors on each side.
The uterus is thus freed from all its attachments down 519 to a point somewhat above the level of the internal os. The vessels that remain to be secured are the uterine arteries.
The peritoneum is next divided by a transverse incision across the anterior face of the uterus, immediately below the line of reflection of the peritoneum from the uterus to the bladder. This incision should join at each end the incisions that had been previously made in dividing the broad ligaments.
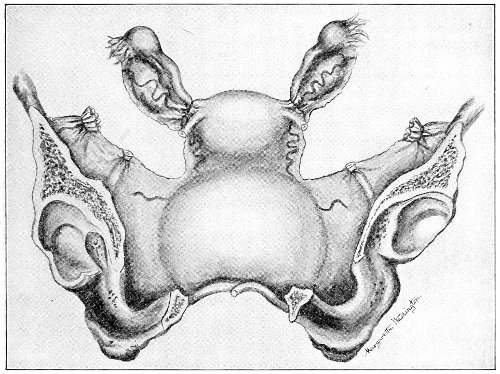
Fig. 214.—Supra-vaginal amputation of the uterus, second step: the broad ligaments have been divided down to the level of the internal os uteri.
The bladder should then be dissected from the anterior face of the uterus and cervix, down to the vaginal junction.
The bladder is but loosely attached to the uterus, and may be readily pushed off with the finger or with closed scissors. The finger pressed out to a short distance on each side of the cervix will push away the anterior layer of the broad ligament with the bladder, so that the uterus is perfectly free in front. 520
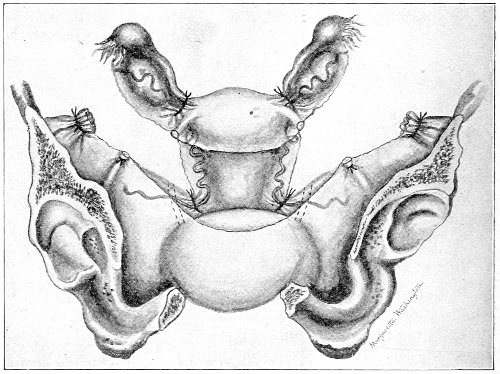
Fig. 215.—Supra-vaginal amputation of the uterus, third step: the peritoneum has been incised across the anterior face of the uterus; the bladder has been dissected from the cervix; the bases of the broad ligaments have been opened; the uterine arteries have been secured by ligatures placed between the ureters and the cervix.
The posterior layer of the broad ligament and the cellular tissue may then be divided, with scissors, along the side of the uterus down to a point somewhat below the level of the internal os. This incision should not be made too close to the uterus, or the uterine artery that runs up along side of the uterus and cervix may be divided. The operator should place one or two fingers upon the posterior aspect of the broad ligament, immediately beside the cervix, and while the uterus is drawn upward should pass a heavy ligature beneath the tissue that includes the uterine artery. The pulsation of the uterine artery may usually be felt by the finger placed behind the broad ligament. This ligature includes the cellular tissue at the base of the broad ligament, the uterine artery, and part of the posterior peritoneal layer of the broad ligament. It does not pass through the anterior 521 peritoneal layer of the broad ligament, which had been previously dissected away. The ligature should be placed as closely as possible to the cervix without including cervical tissue. It should be remembered that the ureter lies about half an inch from the side of the normal cervix and at the level of the external os. The ureter is usually more remote than this when the ligature is passed, because the uterus is drawn upward and the ureter is pushed aside by the fingers at the side of the cervix.
The uterine artery should be secured in a similar way upon the opposite side.
The bases of the broad ligaments should then be divided with scissors between the cervix and the ligatures of the uterine arteries. To prevent slipping of the ligature, ample tissue should be left between the incision and the ligature. As the cervix is not malignant, the incision may be made as close to this structure as necessary.
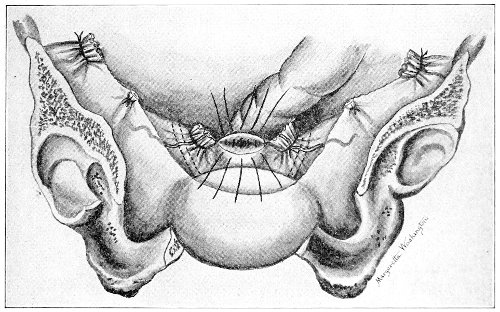
Fig. 216.—Supra-vaginal amputation of the uterus, fourth step: the uterus has been amputated below the level of the internal os; sutures have been introduced to close the stump of the cervix.
The uterus should then be amputated by a wedge-shaped incision through the cervix, making an anterior and a posterior flap. 522
When the cervical canal is opened, it may be immediately sterilized with a solution of bichloride of mercury (1:500).
As the uterus is cut away the flaps of the cervix are secured with forceps. The cervical stump is usually white and dry.
The flaps of the cervix should next be united by interrupted silk suture. Care should be taken to avoid passing a suture through the cervical canal, as it might become infected.
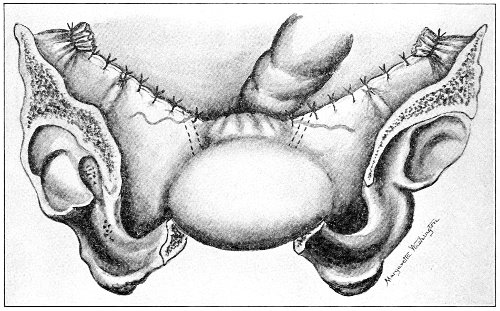
Fig. 217.—Supra-vaginal amputation of the uterus, completed operation: the anterior and posterior peritoneal layers of the broad ligament have been united by sutures; the peritoneal covering of the bladder has been drawn over and sutured to the posterior aspect of the stump of the cervix.
The anterior peritoneal layer of the broad ligament and the peritoneal reflection from the bladder are then drawn over the field of operation and secured by fine silk sutures to the posterior peritoneal layer and the posterior aspect of the cervix. The stump of the cervix, the stump of the uterine arteries, and the cellular tissue of the broad ligaments are thus covered by peritoneum. The only raw surfaces exposed are the stumps of the ovarian arteries and of the round ligaments. These surfaces may also be covered if the operator so desires. 523
Preservation of the Ovaries in Hysterectomy.—Many surgeons consider it advisable to leave the ovaries in hysterectomy for fibroid tumor of the uterus in case these organs are not diseased. If the woman has not yet reached the menopause the disagreeable symptoms of the artificially induced menopause are thus avoided, and any metabolic function that the ovaries may possess is preserved. In hysterectomy for fibroid in women under forty years of age with healthy ovaries it is advisable to leave these organs if this can be done without seriously complicating the operation.
The ovarian artery should be ligated between the ovary and the uterus and the broad ligament should be divided inside of this ligature. The tubes may be left if they can not readily be removed.
Complete Abdominal Hysterectomy.—In this operation the uterus is removed at the vaginal junction. The operation is absolutely necessary in cases of malignant disease of the body and neck of the uterus. It is not often necessary in the treatment of the other conditions for which hysterectomy is performed. The operation requires a longer time than the operation of partial hysterectomy; it is often accompanied by profuse bleeding from the edge of the divided vagina; there is more danger of injury to the ureters, and there is more danger of septic infection, because the vagina is opened; and, finally, the operation very considerably shortens the vaginal canal.
The first steps in the operation of complete hysterectomy are the same as those in partial hysterectomy. In the case of malignant disease of the cervix the ligatures on the uterine arteries should be placed as far from the cervix as possible without including the ureters.
Some surgeons advise the preliminary introduction of bougies into the ureters in order to locate these structures and thus prevent injury to them. If the operator is sure of the position of the ureter he may ligate the uterine artery upon the outer side of the ureter, and carry the 524 incision through structures well outside of the diseased cervix.
After the vessels have been secured and the bladder has been separated from the uterus and the upper part of the vagina, and the broad ligaments have been divided down to the vagina, a transverse incision is made with the knife or scissors into the anterior vaginal fornix. The position of the anterior vaginal fornix may be determined by palpation and percussion. A drum-like sound is obtained by snapping the finger upon the tense vaginal wall.
With the finger in the opening in the anterior vaginal fornix as a guide, the incision is continued around the sides and posterior wall of the vagina. The edge of the vagina is secured by forceps, and bleeding vessels in the walls are ligated. When hemostasis is complete the vagina is closed by sutures that pass through the outer portions of the walls, but do not enter the vaginal canal. The peritoneum is then drawn over the field of operation and the abdomen is closed. If hemostasis is not perfect, gauze drainage through the vagina or the abdominal incision must be employed.
Some operators do not ligate the uterine arteries until the vagina has been opened. The ovarian arteries are secured, the bladder is separated from the uterus and the upper part of the vagina, and the broad ligaments are divided down to a point somewhat below the level of the internal os.
The anterior vaginal fornix is then opened, and the incision is carried around toward the lateral fornices as far as may be done without injury to the uterine arteries. The uterus is then drawn forward and the posterior vaginal fornix is opened, the finger introduced through the opening into the anterior fornix acting as a guide.
The uterus is now attached to the body only by two lateral bands of tissue that include the cellular tissue at the base of the broad ligament, the uterine artery, and a strip of vaginal mucous membrane over the lateral vaginal 525 fornix. This band of tissue, exclusive of the vaginal mucous membrane, is then secured by a ligature that does not enter the vagina, but passes immediately above the strip of vaginal mucous membrane. A finger introduced into the vagina serves to guide the ligature-needle. The uterus may then be cut away.
The ligatures of the uterine arteries are sometimes left long, the ends being carried down into the vagina and a gauze drain being introduced into the vagina, the upper portion of the drain reaching just above the level of the stump of the uterine arteries.
The peritoneum may be left open, or it may be drawn over the drain and the field of operation as already described.
Drainage through the vagina in this way is advisable if the hemostasis be not perfect and if the operator fears septic infection.
In hysterectomy for cancer of the cervix it is usually advisable to remove as much as possible of the cancerous mass by a preliminary operation two or three days beforehand. The diseased tissues should be cut away with the knife, scissors, and the sharp curette, the cavity seared with the thermo-cautery, and closed by approximation of the edges with a few silk sutures. The dangers of septic infection and of transplantation of cancer-cells during the hysterectomy are thus diminished.
The surgeon should always keep in mind the possibility of the transplantation of cancer-cells from diseased into healthy tissues. It seems very probable that some cases of recurrence have been due to this cause. During hysterectomy the operator should therefore avoid, as much as possible, cutting into or manipulating the cancer mass. Instruments, such as hemostatic forceps and volsella forceps, which have grasped diseased tissue, should not be used upon healthy tissue without previous sterilization; and sponges and pads which have been in contact with the cancerous tissue should be discarded.
The methods of operating just described, modified to 526 meet special indications, are applicable to all cases in which hysterectomy is required.
Sometimes, in cases of fibroid tumor, the broad ligament is very much hypertrophied and contains enormous veins, and additional ligatures besides those on the ovarian and uterine arteries are required. It is often necessary to place a large number of forceps upon bleeding vessels on the surface of the tumor as it is cut away from the broad ligament.
The anatomical relations are often very much disturbed, and it may be impossible to determine the position of the cervix and the uterine arteries until the greater part of the tumor has been freed from its connections. Sometimes the tumor so fills the pelvis that it is impossible to ligate, at first, both ovarian arteries. The operator must first attack the more accessible side, ligate the ovarian artery, cut away the broad ligament, strip off the bladder, ligate the uterine artery, and perhaps divide the cervix, before he proceeds to the other side. Bleeding from the tumor must be controlled by the careful application of forceps or ligatures. An inaccessible uterine artery is sometimes most readily reached in this way from below, after the attachments upon the opposite side have been divided and the cervix has been amputated. Some operators perform hysterectomy in all cases by ligating and cutting away from above downward on one side—the more accessible—then cutting across the cervix, and ligating and cutting away on the opposite side from below upward.
The difficulties are greatest in the case of intra-ligamentous fibroids. Such operations are among the most difficult in surgery. The directions given for the treatment of intra-ligamentous cysts are applicable also to this condition. The surgeon should always at first secure the ovarian arteries if possible. He should then incise the peritoneal investment across the anterior or posterior face of the tumor. 527
Enormous veins often lie immediately beneath the peritoneum, and care must be taken to avoid injuring them.
The peritoneum should be stripped off with the fingers or with blunt scissors. Bleeding vessels are secured with forceps as they appear. No attaching structures should be divided until they have been carefully examined, for all anatomical relations are distorted by these growths. The ureter may pass over the top of the tumor, far removed from its normal position on the pelvic floor.
After the surgeon has started the enucleation of a tumor of this kind he must complete the operation. Bleeding cannot be arrested until the tumor has been enucleated, the cervix exposed, and the uterine arteries secured.
The operation is often accompanied by very profuse hemorrhage, but this hemorrhage is always arrested by the ligature of the ovarian and uterine arteries, which alone supply the growth. The surgeon should therefore not delay the operation by the ligature of separate bleeding points until the main vessels have been secured.
Vaginal Hysterectomy.—Vaginal hysterectomy may be performed for the relief of any condition in which the uterus or attached tumor is sufficiently small to pass through the vagina. The operation is very popular with some surgeons. It is but rarely used by the writer. The difficulty in dealing with adhesions and other complications in the upper part of the pelvis seems to be much less when the operation is performed through an abdominal incision.
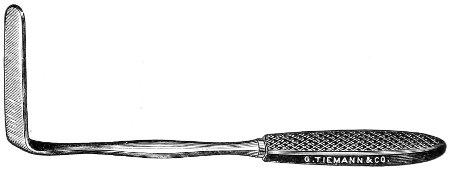
Fig. 218.—Lateral vaginal retractor.] 528
The technique of vaginal hysterectomy varies considerably in the hands of different operators. The vaginal vault is opened with the knife, the scissors, or the cautery. The vessels of the broad ligament are secured with the ligature or with the clamp. The uterus is sometimes divided by longitudinal incision and the halves are separately removed.
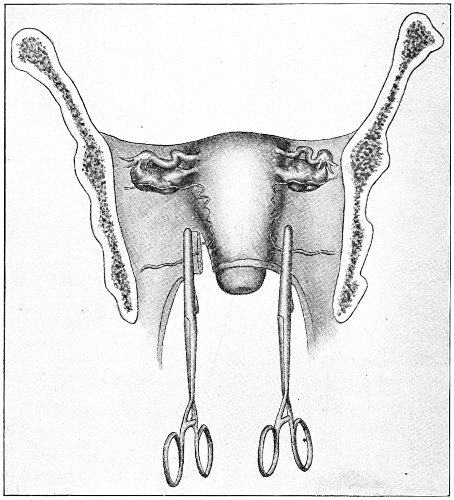
Fig. 219.—Vaginal hysterectomy with clamps: first step (Baldy).
The following are the general directions for the performance of the operation:
The woman is placed in the lithotomy position. The vagina is opened with the Sims speculum and with lateral vaginal retractors (Fig. 218).
If the cervix is septic, it is thoroughly curetted, sterilized 529 with the cautery or by other means, and the sides of the excavation are united by suture.
The cervix is seized by tenaculum forceps and dragged downward and forward.
A transverse incision with knife, scissors, or cautery is made in the posterior vaginal fornix, and Douglas’s pouch is opened.
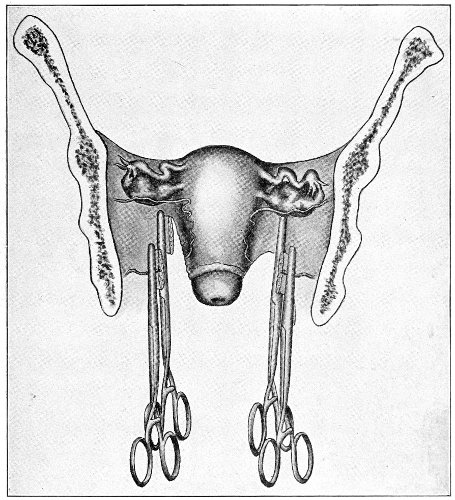
Fig. 220.—Vaginal hysterectomy with clamps: second step (Baldy).
A sponge is introduced into the peritoneum behind the uterus.
Some operators suture the posterior peritoneal layer of Douglas’s pouch to the posterior vaginal wall, to control bleeding and to prevent stripping of the peritoneum. 530
The cervix is now dragged backward and a transverse incision is made across the anterior vaginal fornix.
The bladder is carefully dissected from the anterior face of the cervix with the knife, scissors, and finger, and the utero-vesical fold of peritoneum is opened. The peritoneum and the anterior vaginal wall may here also be united by suture.
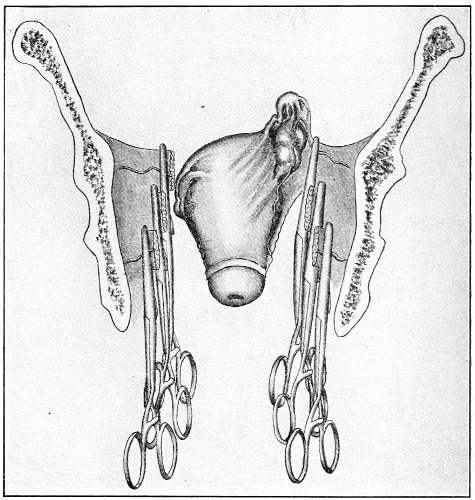
Fig. 221.—Vaginal hysterectomy with clamps: third and final step (Baldy).
An incision may then be made through the vaginal mucous membrane of the lateral fornices, uniting the anterior and posterior incisions.
With a finger in Douglas’s pouch as a guide, the broad ligaments are then secured in successive portions by ligature or by strong clamp forceps, and the uterus is cut away with the scissors as the ligatures or clamps are placed. 531
As the upper portion of the broad ligaments is reached the procedure may be facilitated by retroverting or anteverting the uterus, the fundus being dragged through the posterior or the anterior incisions in the vaginal vault.
The tubes and ovaries should be removed when possible, especially in the case of malignant disease.
After the uterus has been removed the vagina may be packed with a gauze drain that reaches upward between the stumps of the uterine arteries; or, if ligatures have been used, the vaginal vault may be closed. The former procedure is the safer. When the gauze drain is used, it is advisable to leave the ends of the ligatures on the uterine arteries long and protruding into the vagina. The ligatures usually become infected, and their removal is facilitated by this procedure. If clamps are used, they should be removed in forty-eight hours.
The treatment after vaginal hysterectomy is the same as that already described after celiotomy.
Combined Vaginal and Abdominal Hysterectomy.—A combined vaginal and abdominal operation is sometimes performed in order to enable the surgeon to deal with adhesions and other complications in the upper part of the pelvis.
The operation is usually begun below. The vaginal connections and the bladder are separated from the uterus, and the bases of the broad ligaments are secured with the ligature or the clamp; the cervix is freed from its attachments to the broad ligament.
The abdomen is then opened and the operation is finished from above, the uterus being removed through the abdominal incision.
The writer performs the combined operation in the reverse order, as follows:
The abdomen is first opened. The ovarian arteries and the round ligaments are secured by ligature. The bladder is separated from the uterus and the upper part of the vagina. The broad ligaments are divided to a point somewhat below the level of the internal os. 532
A gauze pad is then introduced to the bottom of Douglas’s pouch, and another to the bottom of the space between the uterus and the bladder. The abdominal incision is then closed.
The rest of the operation is performed through the vagina. The posterior and anterior vaginal fornices are opened by incisions made directly upon the gauze pads. The vaginal mucous membrane is divided over the vaginal fornices by an incision that joins the anterior and posterior incisions in the vaginal vault. The bases of the broad ligaments are secured by strong clamp-forceps, and the uterus is cut away and removed through the vagina. The gauze pads are then removed, and the vagina is drained with gauze introduced as far as the upper end of the forceps.
The following are the advantages of the latter method of operating:
If sterilization of the vagina and the cervix is not perfect, the cleaner part of the operation is performed first. The bladder is more easily separated from the uterus by operating from above than by way of the vagina. The vaginal vault is quickly and safely opened by incisions made upon the gauze pads, which keep the intestines out of the way.
The uterus and the infected cervix are removed through the vagina, and not through the abdominal cavity.
If the operation is performed for cancer of the cervix, the incision is made more accurately beyond the limits of the disease if the vaginal vault is opened through the vagina than if it is opened from above.
Werder, of Pittsburg, has advised the following combined operation: The abdomen is opened, and the uterus, tubes, and ovaries are freed as in ordinary hysterectomy. The ureters are dissected out, and the uterine arteries are ligated near their origin. The bladder is entirely freed from the uterus, and also, for a considerable distance, from the vagina. The recto-vaginal space is then opened, and the posterior vaginal wall is stripped 533 from the rectum as far down as necessary. The lateral vaginal attachments are loosened. The uterus and vagina are then pushed down into the pelvic outlet, and the peritoneum from the anterior pelvic wall is united with that covering the rectum, thus shutting off the pelvis from the general peritoneal cavity and covering all raw surfaces with peritoneum. The abdomen is then closed.
The patient is then placed in the lithotomy position. The uterus—which is found protruding at the vulva—is seized with volsella forceps and drawn completely out of the vulvar orifice with the inverted vagina. With the finger in the rectum and the sound in the bladder as safeguards against injuring these organs, the inverted vagina is amputated with the knife or the thermo-cautery. The chief advantage of this operation is that a large vaginal cuff may be removed.
Abdominal Myomectomy.—In some cases of uterine fibroid it is proper to remove the tumor without taking away the uterus. This operation—myomectomy—is performed as follows:
The abdomen is opened by a free incision, the pelvis is elevated, and the intestines are displaced from the pelvic cavity in the usual manner. The tumor and the uterus are surrounded by gauze sponges, and, where possible, should be brought outside the abdominal cavity. An incision is made around the pedicle or through the capsule of the tumor, and it is enucleated by dissection with the sharp or the blunt end of the scalpel. During the operation hemorrhage may be controlled by an assistant, who compresses with his fingers the vessels on each side of the uterus, or by placing a temporary rubber ligature about the cervix uteri.
Hemostasis is effected and the wound in the uterus is closed by layers of continuous or interrupted catgut sutures. Great care should be taken to prevent hemorrhage between the layers of suture, and to insure accurate closure of the incision in the uterus. The temporary 534 ligature about the cervix, or the compression of the vessels of the broad ligaments, should be removed from time to time during the process of suturing and after closure of the uterine wound, in order to determine the position of bleeding points and the efficiency of the hemostasis; and before closing the abdominal incision the uterine wound should be inspected for several minutes while the woman is in the horizontal position.
The abdomen may usually be closed without drainage. 535
Removal of the tube and ovary upon one side has no effect upon menstruation or upon any of the other characteristics of the woman.
Removal of the tubes and ovaries upon both sides is followed within forty-eight hours by slight bleeding from the uterus, lasting for one or two days.
If the removal of the tubes and ovaries has been complete, menstruation, in the majority of cases, never reappears.
In a few cases menstruation appears for one, two, or three periods after the operation, usually in diminished amount, and then ceases for ever. In some other cases there is a period of a few months of amenorrhea, followed by two or three scanty menstrual flows, before the bleeding permanently ceases.
These phenomena, it will be observed, are similar to those of the normal menopause.
The woman after double salpingo-oöphorectomy experiences the nervous and gastro-intestinal disturbances that so usually accompany the menopause. She, in fact, passes through a premature menopause, the phenomena of which may persist for one or two years.
The secondary sexual characteristics of the woman—the voice, the figure, and the growth of hair—are not altered if the appendages are removed during adult life. The case may be different if the appendages are removed in the undeveloped girl, in whom the ovarian influence is essential for complete development.
The woman loses none of her feminine attractions. 536 She may, indeed, become better-looking if the operation has relieved chronic suffering. It is said that Gyges, king of Lydia, caused the removal of ovaries from women with a view to prolonging their charms.
Double oöphorectomy may be followed by obesity if the woman have a tendency to form fat. The relief of suffering and the consequent improved nutrition favor the development of obesity. There seems to be nothing inherent in the operation to cause it. Many women remain thin after the operation.
The emotions of the woman are unaltered by double oöphorectomy, with the exception of some cases in which the sexual desire is destroyed. Sexual desire is dependent upon such a variety of conditions, both within and without the woman, that it is difficult to determine the amount of influence that removal of the ovaries exerts upon this feeling.
It is undoubtedly true that sexual desire is sometimes destroyed by the operation. On the other hand, the sexual desire is very often restored by the operation, which relieves the former dyspareunia, or painful coitus. 537

1 Diseases of the Ovaries, 1883, p. 6.
2 Heape, Trans. Obstet. Soc. of London, vols. xxxvi., xl.
3 New York Journal of Gynecology and Obstetrics, March, 1894, p. 282.
4 “The Ligature in Oöphorectomy,” read before the Philadelphia Academy of Surgery, February 3, 1896.
Inconsistent spelling and hyphenation are as in the original.
End of the Project Gutenberg EBook of A Text-book of Diseases of Women, by
Charles Bingham Penrose
*** END OF THIS PROJECT GUTENBERG EBOOK A TEXT-BOOK OF DISEASES OF WOMEN ***
***** This file should be named 54982-h.htm or 54982-h.zip *****
This and all associated files of various formats will be found in:
http://www.gutenberg.org/5/4/9/8/54982/
Produced by deaurider, Wayne Hammond and the Online
Distributed Proofreading Team at http://www.pgdp.net (This
file was produced from images generously made available
by The Internet Archive)
Updated editions will replace the previous one--the old editions will
be renamed.
Creating the works from print editions not protected by U.S. copyright
law means that no one owns a United States copyright in these works,
so the Foundation (and you!) can copy and distribute it in the United
States without permission and without paying copyright
royalties. Special rules, set forth in the General Terms of Use part
of this license, apply to copying and distributing Project
Gutenberg-tm electronic works to protect the PROJECT GUTENBERG-tm
concept and trademark. Project Gutenberg is a registered trademark,
and may not be used if you charge for the eBooks, unless you receive
specific permission. If you do not charge anything for copies of this
eBook, complying with the rules is very easy. You may use this eBook
for nearly any purpose such as creation of derivative works, reports,
performances and research. They may be modified and printed and given
away--you may do practically ANYTHING in the United States with eBooks
not protected by U.S. copyright law. Redistribution is subject to the
trademark license, especially commercial redistribution.
START: FULL LICENSE
THE FULL PROJECT GUTENBERG LICENSE
PLEASE READ THIS BEFORE YOU DISTRIBUTE OR USE THIS WORK
To protect the Project Gutenberg-tm mission of promoting the free
distribution of electronic works, by using or distributing this work
(or any other work associated in any way with the phrase "Project
Gutenberg"), you agree to comply with all the terms of the Full
Project Gutenberg-tm License available with this file or online at
www.gutenberg.org/license.
Section 1. General Terms of Use and Redistributing Project
Gutenberg-tm electronic works
1.A. By reading or using any part of this Project Gutenberg-tm
electronic work, you indicate that you have read, understand, agree to
and accept all the terms of this license and intellectual property
(trademark/copyright) agreement. If you do not agree to abide by all
the terms of this agreement, you must cease using and return or
destroy all copies of Project Gutenberg-tm electronic works in your
possession. If you paid a fee for obtaining a copy of or access to a
Project Gutenberg-tm electronic work and you do not agree to be bound
by the terms of this agreement, you may obtain a refund from the
person or entity to whom you paid the fee as set forth in paragraph
1.E.8.
1.B. "Project Gutenberg" is a registered trademark. It may only be
used on or associated in any way with an electronic work by people who
agree to be bound by the terms of this agreement. There are a few
things that you can do with most Project Gutenberg-tm electronic works
even without complying with the full terms of this agreement. See
paragraph 1.C below. There are a lot of things you can do with Project
Gutenberg-tm electronic works if you follow the terms of this
agreement and help preserve free future access to Project Gutenberg-tm
electronic works. See paragraph 1.E below.
1.C. The Project Gutenberg Literary Archive Foundation ("the
Foundation" or PGLAF), owns a compilation copyright in the collection
of Project Gutenberg-tm electronic works. Nearly all the individual
works in the collection are in the public domain in the United
States. If an individual work is unprotected by copyright law in the
United States and you are located in the United States, we do not
claim a right to prevent you from copying, distributing, performing,
displaying or creating derivative works based on the work as long as
all references to Project Gutenberg are removed. Of course, we hope
that you will support the Project Gutenberg-tm mission of promoting
free access to electronic works by freely sharing Project Gutenberg-tm
works in compliance with the terms of this agreement for keeping the
Project Gutenberg-tm name associated with the work. You can easily
comply with the terms of this agreement by keeping this work in the
same format with its attached full Project Gutenberg-tm License when
you share it without charge with others.
1.D. The copyright laws of the place where you are located also govern
what you can do with this work. Copyright laws in most countries are
in a constant state of change. If you are outside the United States,
check the laws of your country in addition to the terms of this
agreement before downloading, copying, displaying, performing,
distributing or creating derivative works based on this work or any
other Project Gutenberg-tm work. The Foundation makes no
representations concerning the copyright status of any work in any
country outside the United States.
1.E. Unless you have removed all references to Project Gutenberg:
1.E.1. The following sentence, with active links to, or other
immediate access to, the full Project Gutenberg-tm License must appear
prominently whenever any copy of a Project Gutenberg-tm work (any work
on which the phrase "Project Gutenberg" appears, or with which the
phrase "Project Gutenberg" is associated) is accessed, displayed,
performed, viewed, copied or distributed:
This eBook is for the use of anyone anywhere in the United States and
most other parts of the world at no cost and with almost no
restrictions whatsoever. You may copy it, give it away or re-use it
under the terms of the Project Gutenberg License included with this
eBook or online at www.gutenberg.org. If you are not located in the
United States, you'll have to check the laws of the country where you
are located before using this ebook.
1.E.2. If an individual Project Gutenberg-tm electronic work is
derived from texts not protected by U.S. copyright law (does not
contain a notice indicating that it is posted with permission of the
copyright holder), the work can be copied and distributed to anyone in
the United States without paying any fees or charges. If you are
redistributing or providing access to a work with the phrase "Project
Gutenberg" associated with or appearing on the work, you must comply
either with the requirements of paragraphs 1.E.1 through 1.E.7 or
obtain permission for the use of the work and the Project Gutenberg-tm
trademark as set forth in paragraphs 1.E.8 or 1.E.9.
1.E.3. If an individual Project Gutenberg-tm electronic work is posted
with the permission of the copyright holder, your use and distribution
must comply with both paragraphs 1.E.1 through 1.E.7 and any
additional terms imposed by the copyright holder. Additional terms
will be linked to the Project Gutenberg-tm License for all works
posted with the permission of the copyright holder found at the
beginning of this work.
1.E.4. Do not unlink or detach or remove the full Project Gutenberg-tm
License terms from this work, or any files containing a part of this
work or any other work associated with Project Gutenberg-tm.
1.E.5. Do not copy, display, perform, distribute or redistribute this
electronic work, or any part of this electronic work, without
prominently displaying the sentence set forth in paragraph 1.E.1 with
active links or immediate access to the full terms of the Project
Gutenberg-tm License.
1.E.6. You may convert to and distribute this work in any binary,
compressed, marked up, nonproprietary or proprietary form, including
any word processing or hypertext form. However, if you provide access
to or distribute copies of a Project Gutenberg-tm work in a format
other than "Plain Vanilla ASCII" or other format used in the official
version posted on the official Project Gutenberg-tm web site
(www.gutenberg.org), you must, at no additional cost, fee or expense
to the user, provide a copy, a means of exporting a copy, or a means
of obtaining a copy upon request, of the work in its original "Plain
Vanilla ASCII" or other form. Any alternate format must include the
full Project Gutenberg-tm License as specified in paragraph 1.E.1.
1.E.7. Do not charge a fee for access to, viewing, displaying,
performing, copying or distributing any Project Gutenberg-tm works
unless you comply with paragraph 1.E.8 or 1.E.9.
1.E.8. You may charge a reasonable fee for copies of or providing
access to or distributing Project Gutenberg-tm electronic works
provided that
* You pay a royalty fee of 20% of the gross profits you derive from
the use of Project Gutenberg-tm works calculated using the method
you already use to calculate your applicable taxes. The fee is owed
to the owner of the Project Gutenberg-tm trademark, but he has
agreed to donate royalties under this paragraph to the Project
Gutenberg Literary Archive Foundation. Royalty payments must be paid
within 60 days following each date on which you prepare (or are
legally required to prepare) your periodic tax returns. Royalty
payments should be clearly marked as such and sent to the Project
Gutenberg Literary Archive Foundation at the address specified in
Section 4, "Information about donations to the Project Gutenberg
Literary Archive Foundation."
* You provide a full refund of any money paid by a user who notifies
you in writing (or by e-mail) within 30 days of receipt that s/he
does not agree to the terms of the full Project Gutenberg-tm
License. You must require such a user to return or destroy all
copies of the works possessed in a physical medium and discontinue
all use of and all access to other copies of Project Gutenberg-tm
works.
* You provide, in accordance with paragraph 1.F.3, a full refund of
any money paid for a work or a replacement copy, if a defect in the
electronic work is discovered and reported to you within 90 days of
receipt of the work.
* You comply with all other terms of this agreement for free
distribution of Project Gutenberg-tm works.
1.E.9. If you wish to charge a fee or distribute a Project
Gutenberg-tm electronic work or group of works on different terms than
are set forth in this agreement, you must obtain permission in writing
from both the Project Gutenberg Literary Archive Foundation and The
Project Gutenberg Trademark LLC, the owner of the Project Gutenberg-tm
trademark. Contact the Foundation as set forth in Section 3 below.
1.F.
1.F.1. Project Gutenberg volunteers and employees expend considerable
effort to identify, do copyright research on, transcribe and proofread
works not protected by U.S. copyright law in creating the Project
Gutenberg-tm collection. Despite these efforts, Project Gutenberg-tm
electronic works, and the medium on which they may be stored, may
contain "Defects," such as, but not limited to, incomplete, inaccurate
or corrupt data, transcription errors, a copyright or other
intellectual property infringement, a defective or damaged disk or
other medium, a computer virus, or computer codes that damage or
cannot be read by your equipment.
1.F.2. LIMITED WARRANTY, DISCLAIMER OF DAMAGES - Except for the "Right
of Replacement or Refund" described in paragraph 1.F.3, the Project
Gutenberg Literary Archive Foundation, the owner of the Project
Gutenberg-tm trademark, and any other party distributing a Project
Gutenberg-tm electronic work under this agreement, disclaim all
liability to you for damages, costs and expenses, including legal
fees. YOU AGREE THAT YOU HAVE NO REMEDIES FOR NEGLIGENCE, STRICT
LIABILITY, BREACH OF WARRANTY OR BREACH OF CONTRACT EXCEPT THOSE
PROVIDED IN PARAGRAPH 1.F.3. YOU AGREE THAT THE FOUNDATION, THE
TRADEMARK OWNER, AND ANY DISTRIBUTOR UNDER THIS AGREEMENT WILL NOT BE
LIABLE TO YOU FOR ACTUAL, DIRECT, INDIRECT, CONSEQUENTIAL, PUNITIVE OR
INCIDENTAL DAMAGES EVEN IF YOU GIVE NOTICE OF THE POSSIBILITY OF SUCH
DAMAGE.
1.F.3. LIMITED RIGHT OF REPLACEMENT OR REFUND - If you discover a
defect in this electronic work within 90 days of receiving it, you can
receive a refund of the money (if any) you paid for it by sending a
written explanation to the person you received the work from. If you
received the work on a physical medium, you must return the medium
with your written explanation. The person or entity that provided you
with the defective work may elect to provide a replacement copy in
lieu of a refund. If you received the work electronically, the person
or entity providing it to you may choose to give you a second
opportunity to receive the work electronically in lieu of a refund. If
the second copy is also defective, you may demand a refund in writing
without further opportunities to fix the problem.
1.F.4. Except for the limited right of replacement or refund set forth
in paragraph 1.F.3, this work is provided to you 'AS-IS', WITH NO
OTHER WARRANTIES OF ANY KIND, EXPRESS OR IMPLIED, INCLUDING BUT NOT
LIMITED TO WARRANTIES OF MERCHANTABILITY OR FITNESS FOR ANY PURPOSE.
1.F.5. Some states do not allow disclaimers of certain implied
warranties or the exclusion or limitation of certain types of
damages. If any disclaimer or limitation set forth in this agreement
violates the law of the state applicable to this agreement, the
agreement shall be interpreted to make the maximum disclaimer or
limitation permitted by the applicable state law. The invalidity or
unenforceability of any provision of this agreement shall not void the
remaining provisions.
1.F.6. INDEMNITY - You agree to indemnify and hold the Foundation, the
trademark owner, any agent or employee of the Foundation, anyone
providing copies of Project Gutenberg-tm electronic works in
accordance with this agreement, and any volunteers associated with the
production, promotion and distribution of Project Gutenberg-tm
electronic works, harmless from all liability, costs and expenses,
including legal fees, that arise directly or indirectly from any of
the following which you do or cause to occur: (a) distribution of this
or any Project Gutenberg-tm work, (b) alteration, modification, or
additions or deletions to any Project Gutenberg-tm work, and (c) any
Defect you cause.
Section 2. Information about the Mission of Project Gutenberg-tm
Project Gutenberg-tm is synonymous with the free distribution of
electronic works in formats readable by the widest variety of
computers including obsolete, old, middle-aged and new computers. It
exists because of the efforts of hundreds of volunteers and donations
from people in all walks of life.
Volunteers and financial support to provide volunteers with the
assistance they need are critical to reaching Project Gutenberg-tm's
goals and ensuring that the Project Gutenberg-tm collection will
remain freely available for generations to come. In 2001, the Project
Gutenberg Literary Archive Foundation was created to provide a secure
and permanent future for Project Gutenberg-tm and future
generations. To learn more about the Project Gutenberg Literary
Archive Foundation and how your efforts and donations can help, see
Sections 3 and 4 and the Foundation information page at
www.gutenberg.org Section 3. Information about the Project Gutenberg
Literary Archive Foundation
The Project Gutenberg Literary Archive Foundation is a non profit
501(c)(3) educational corporation organized under the laws of the
state of Mississippi and granted tax exempt status by the Internal
Revenue Service. The Foundation's EIN or federal tax identification
number is 64-6221541. Contributions to the Project Gutenberg Literary
Archive Foundation are tax deductible to the full extent permitted by
U.S. federal laws and your state's laws.
The Foundation's principal office is in Fairbanks, Alaska, with the
mailing address: PO Box 750175, Fairbanks, AK 99775, but its
volunteers and employees are scattered throughout numerous
locations. Its business office is located at 809 North 1500 West, Salt
Lake City, UT 84116, (801) 596-1887. Email contact links and up to
date contact information can be found at the Foundation's web site and
official page at www.gutenberg.org/contact
For additional contact information:
Dr. Gregory B. Newby
Chief Executive and Director
[email protected]
Section 4. Information about Donations to the Project Gutenberg
Literary Archive Foundation
Project Gutenberg-tm depends upon and cannot survive without wide
spread public support and donations to carry out its mission of
increasing the number of public domain and licensed works that can be
freely distributed in machine readable form accessible by the widest
array of equipment including outdated equipment. Many small donations
($1 to $5,000) are particularly important to maintaining tax exempt
status with the IRS.
The Foundation is committed to complying with the laws regulating
charities and charitable donations in all 50 states of the United
States. Compliance requirements are not uniform and it takes a
considerable effort, much paperwork and many fees to meet and keep up
with these requirements. We do not solicit donations in locations
where we have not received written confirmation of compliance. To SEND
DONATIONS or determine the status of compliance for any particular
state visit www.gutenberg.org/donate
While we cannot and do not solicit contributions from states where we
have not met the solicitation requirements, we know of no prohibition
against accepting unsolicited donations from donors in such states who
approach us with offers to donate.
International donations are gratefully accepted, but we cannot make
any statements concerning tax treatment of donations received from
outside the United States. U.S. laws alone swamp our small staff.
Please check the Project Gutenberg Web pages for current donation
methods and addresses. Donations are accepted in a number of other
ways including checks, online payments and credit card donations. To
donate, please visit: www.gutenberg.org/donate
Section 5. General Information About Project Gutenberg-tm electronic works.
Professor Michael S. Hart was the originator of the Project
Gutenberg-tm concept of a library of electronic works that could be
freely shared with anyone. For forty years, he produced and
distributed Project Gutenberg-tm eBooks with only a loose network of
volunteer support.
Project Gutenberg-tm eBooks are often created from several printed
editions, all of which are confirmed as not protected by copyright in
the U.S. unless a copyright notice is included. Thus, we do not
necessarily keep eBooks in compliance with any particular paper
edition.
Most people start at our Web site which has the main PG search
facility: www.gutenberg.org
This Web site includes information about Project Gutenberg-tm,
including how to make donations to the Project Gutenberg Literary
Archive Foundation, how to help produce our new eBooks, and how to
subscribe to our email newsletter to hear about new eBooks.