Project Gutenberg's The Home Medical Library, Volume I (of VI), by Various
This eBook is for the use of anyone anywhere at no cost and with
almost no restrictions whatsoever. You may copy it, give it away or
re-use it under the terms of the Project Gutenberg License included
with this eBook or online at www.gutenberg.org
Title: The Home Medical Library, Volume I (of VI)
Author: Various
Editor: Kenelm Winslow
Release Date: January 31, 2009 [EBook #27943]
Language: English
Character set encoding: ISO-8859-1
*** START OF THIS PROJECT GUTENBERG EBOOK THE HOME MEDICAL LIBRARY ***
Produced by Juliet Sutherland, Chris Logan and the Online
Distributed Proofreading Team at http://www.pgdp.net
The Home Medical
Library
By
Kenelm Winslow, B.A.S., M.D.
Formerly Assistant Professor Comparative Therapeutics, Harvard
University; Late Surgeon to the Newton Hospital;
Fellow of the Massachusetts Medical Society, etc.
With the Coöperation of Many Medical
Advising Editors and Special Contributors
IN SIX VOLUMES
First Aid :: Family Medicines :: Nose, Throat, Lungs,
Eye, and Ear :: Stomach and Bowels :: Tumors and
Skin Diseases :: Rheumatism :: Germ Diseases
Nervous Diseases :: Insanity :: Sexual Hygiene
Woman and Child :: Heart, Blood, and Digestion
Personal Hygiene :: Indoor Exercise
Diet and Conduct for Long Life :: Practical
Kitchen Science :: Nervousness
and Outdoor Life :: Nurse and Patient
Camping Comfort :: Sanitation
of the Household :: Pure
Water Supply :: Pure Food
Stable and Kennel
New York
The Review of Reviews Company
1907
Medical Advising Editors
Managing Editor
Albert Warren Ferris, A.M., M.D.
Former Assistant in Neurology, Columbia University; Former Chairman,
Section on Neurology and Psychiatry, New York Academy of Medicine;
Assistant in Medicine, University and Bellevue Hospital Medical
College; Medical Editor, New International Encyclopedia.
Nervous Diseases
Charles E. Atwood, M.D.
Assistant in Neurology, Columbia University; Former Physician, Utica
State Hospital and Bloomingdale Hospital for Insane Patients; Former
Clinical Assistant to Sir William Gowers, National Hospital, London.
Pregnancy
Russell Bellamy, M.D.
Assistant in Obstetrics and Gynecology, Cornell University Medical
College Dispensary; Captain and Assistant Surgeon (in charge),
Squadron A, New York Cavalry; Assistant in Surgery, New York
Polyclinic.
Germ Diseases
Hermann Michael Biggs, M.D.
General Medical Officer and Director of Bacteriological Laboratories,
New York City Department of Health; Professor of Clinical Medicine in
University and Bellevue Hospital Medical College; Visiting Physician
to Bellevue, St. Vincent's, Willard Parker, and Riverside Hospitals.
The Eye and Ear
J. Herbert Claiborne, M.D.
Clinical Instructor in Ophthalmology, Cornell University Medical
College; Former Adjunct Professor of Ophthalmology, New York
Polyclinic; Former Instructor in Ophthalmology in Columbia University;
Surgeon, New Amsterdam Eye and Ear Hospital.
Sanitation
Thomas Darlington, M.D.
Health Commissioner of New York City; Former President Medical Board,
New York Foundling Hospital; Consulting Physician, French Hospital;
Attending Physician, St. John's Riverside Hospital, Yonkers; Surgeon
to New Croton Aqueduct and other Public Works, to Copper Queen
Consolidated Mining Company of Arizona, and Arizona and Southeastern
Railroad Hospital; Author of Medical and Climatological Works.
Menstruation
Austin Flint, Jr., M.D.
Professor of Obstetrics and Clinical Gynecology, New York University
and Bellevue Hospital Medical College; Visiting Physician, Bellevue
Hospital; Consulting Obstetrician, New York Maternity Hospital;
Attending Physician, Hospital for Ruptured and Crippled, Manhattan
Maternity and Emergency Hospitals.
Heart and Blood
John Bessner Huber, A.M., M.D.
Assistant in Medicine, University and Bellevue Hospital Medical
College; Visiting Physician to St. Joseph's Home for Consumptives;
Author of "Consumption: Its Relation to Man and His Civilization; Its
Prevention and Cure."
Skin Diseases
James C. Johnston, A.B., M.D.
Instructor in Pathology and Chief of Clinic, Department of
Dermatology, Cornell University Medical College.
Diseases of Children
Charles Gilmore Kerley, M.D.
Professor of Pediatrics, New York Polyclinic Medical School and
Hospital; Attending Physician, New York Infant Asylum, Children's
Department of Sydenham Hospital, and Babies' Hospital, N. Y.;
Consulting Physician, Home for Crippled Children.
Bites and Stings
George Gibier Rambaud, M.D.
President, New York Pasteur Institute.
Headache
Alonzo D. Rockwell, A.M., M.D.
Former Professor Electro-Therapeutics and Neurology at New York
Post-Graduate Medical School; Neurologist and Electro-Therapeutist to
the Flushing Hospital; Former Electro-Therapeutist to the Woman's
Hospital in the State of New York; Author of Works on Medical and
Surgical Uses of Electricity, Nervous Exhaustion (Neurasthenia), etc.
Poisons
E. Ellsworth Smith, M.D.
Pathologist, St. John's Hospital, Yonkers; Somerset Hospital,
Somerville, N. J.; Trinity Hospital, St. Bartholomew's Clinic, and the
New York West Side German Dispensary.
Catarrh
Samuel Wood Thurber, M.D.
Chief of Clinic and Instructor in Laryngology, Columbia University;
Laryngologist to the Orphan's Home and Hospital.
Care of Infants
Herbert B. Wilcox, M.D.
Assistant in Diseases of Children, Columbia University.
Special Contributors
Food Adulteration
S. Josephine Baker, M.D.
Medical Inspector, New York City Department of Health.
Pure Water Supply
William Paul Gerhard, C.E.
Consulting Engineer for Sanitary Works; Member of American Public
Health Association; Member, American Society Mechanical Engineers;
Corresponding Member of American Institute of Architects, etc.; Author
of "House Drainage," etc.
Care of Food
Janet McKenzie Hill
Editor, Boston Cooking School Magazine.
Nerves and Outdoor Life
S. Weir Mitchell, M.D., LL.D.
LL.D. (Harvard, Edinburgh, Princeton); Former President, Philadelphia
College of Physicians; Member, National Academy of Sciences,
Association of American Physicians, etc.; Author of essays: "Injuries
to Nerves," "Doctor and Patient," "Fat and Blood," etc.; of scientific
works: "Researches Upon the Venom of the Rattlesnake," etc.; of
novels: "Hugh Wynne," "Characteristics," "Constance Trescott," "The
Adventures of François," etc.
Sanitation
George M. Price, M.D.
Former Medical Sanitary Inspector, Department of Health, New York
City; Inspector, New York Sanitary Aid Society of the 10th Ward, 1885;
Manager, Model Tenement-houses of the New York Tenement-house Building
Co., 1888; Inspector, New York State Tenement-house Commission, 1895;
Author of "Tenement-house Inspection," "Handbook on Sanitation," etc.
Indoor Exercise
Dudley Allen Sargent, M.D.
Director of Hemenway Gymnasium, Harvard University; Former President,
American Physical Culture Society; Director, Normal School of Physical
Training, Cambridge, Mass.; President, American Association for
Promotion of Physical Education; Author of "Universal Test for
Strength," "Health, Strength and Power," etc.
Long Life
Sir Henry Thompson, Bart., F.R.C.S., M.B. (Lond.)
Surgeon Extraordinary to His Majesty the King of the Belgians;
Consulting Surgeon to University College Hospital, London; Emeritus
Professor of Clinical Surgery to University College, London, etc.
Camp Comfort
Stewart Edward White
Author of "The Forest," "The Mountains," "The Silent Places," "The
Blazed Trail," etc.
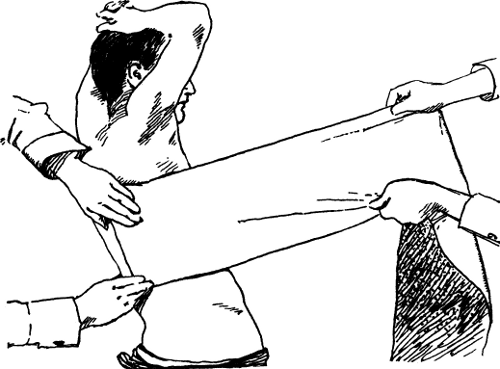
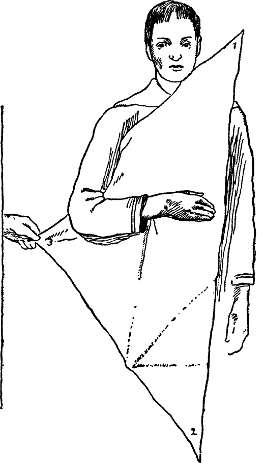
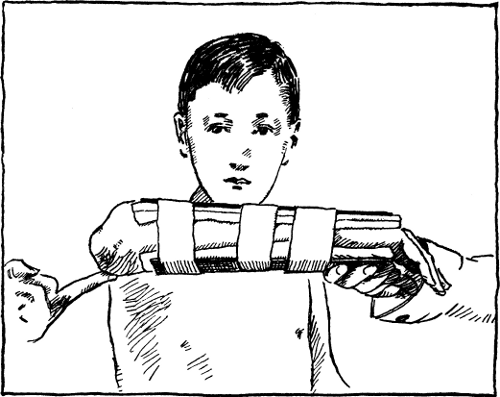
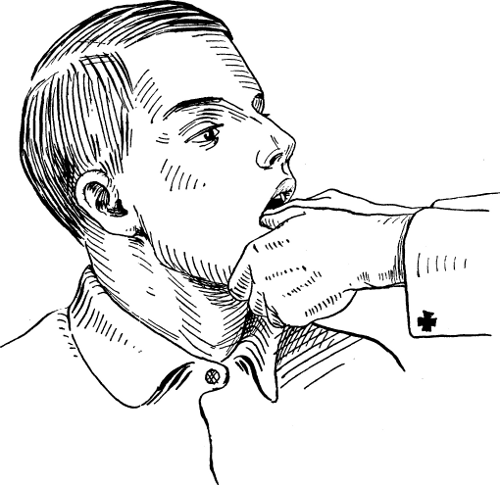
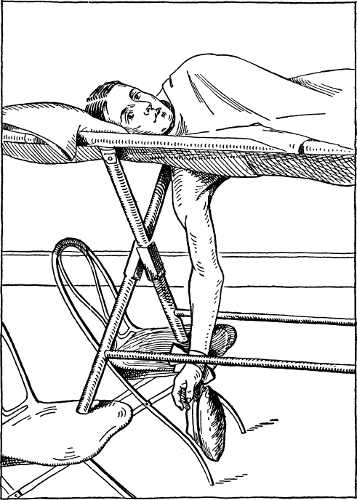
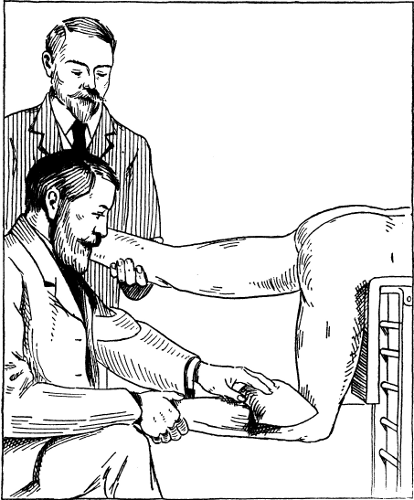
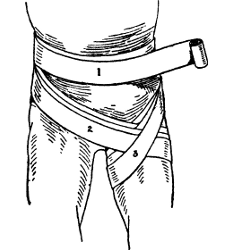
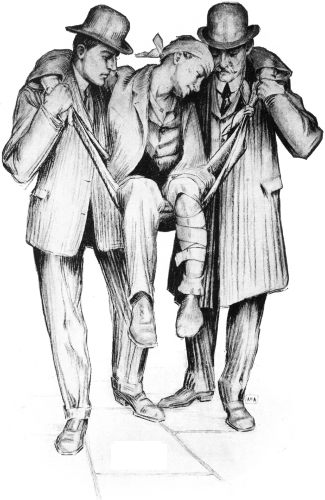 A DESIRABLE METHOD OF CARRYING THE INJURED.
A DESIRABLE METHOD OF CARRYING THE INJURED.
By this plan even the unconscious victim of an accident may be
transported a long distance, because the bearers' hands are left
entirely free and thus prevented from becoming cramped or tired, as
when a "seat" is made with clasped hands. In the method illustrated
above the patient is placed in a seat made by tying a blanket, sheet,
rope, or strap in the form of a ring. Each bearer then places his
inner arm about the patient's body and with his outer hand holds the
patient's arm around his neck.
The Home Medical
Library
Volume I
FIRST AID IN EMERGENCIES
By KENELM WINSLOW, B.A.S., M.D. (Harv.)
Formerly Assistant Professor Comparative Therapeutics, Harvard University;
Late Surgeon to the Newton Hospital; Fellow of
the Massachusetts Medical Society, etc.
ASSISTED BY
ALBERT WARREN FERRIS, A.M., M.D.
Former Assistant in Neurology, Columbia University; former Chairman,
Section on Neurology and Psychiatry, New York Academy
of Medicine; Assistant in Medicine, University and Bellevue
Hospital Medical College; Medical Editor,
"New International Encyclopedia"
GERM DISEASES
By KENELM WINSLOW, B.A.S., M.D. (Harv.)
New York
The Review of Reviews Company
1907
Copyright, 1907, by
The Review of Reviews Company
THE TROW PRESS, NEW YORK
[Pg 1]
Contents
PART I
| CHAPTER |
|
PAGE |
| I. |
Restoring the Apparently Drowned |
27 |
| |
Reviving the Patient—How to Expel Water
from the Stomach and Chest—Instructions
for Producing Respiration—When
Several Workers are at Hand—When
One must Work Alone—How to Save a
Drowning Person. |
|
| II. |
Heat Stroke and Electric Shock |
39 |
| |
First-aid Rules—Symptoms of Heat Exhaustion—Treatment
of Heat Prostration—What
to Do in Case of Electric Shock—Symptoms—Artificial
Respiration—Mortality
in Lightning Strokes. |
|
| III. |
Wounds, Sprains, and Bruises |
50 |
| |
Treatment of Wounds—Bleeding from Arteries
and Veins—Punctured Wounds—Oozing—Lockjaw—Bruises—Abrasions—Sprains
and Their Treatment—Synovitis—Bunions
and Felons—Weeping
Sinew—Foreign Bodies in Eye, Ear, and
Nose. |
|
| IV.[Pg 2] |
Fractures |
80 |
| |
How to Detect Broken Bones—Fracture
of Rib and Collar Bone—Instructions for
Applying Dressings—Bandage for Broken
Jaw—Fracture of Shoulder-blade, Arm,
Hip, Leg, and Other Bones—Compound
Fractures. |
|
| V. |
Dislocations |
118 |
| |
Varieties of Dislocations—Method of Reducing
a Dislocated Jaw—A Dislocated
Shoulder—Indications when Elbow is Out
of Joint—Dislocation of Hip, etc.—Forms
of Bandages. |
|
| VI. |
Ordinary Poisons |
139 |
| |
Unknown Poisons—Symptoms and Antidotes—Poisoning
by Carbolic and Other
Acids—Alkalies—Metal Poisoning—Aconite,
Belladonna, and Other Narcotics—Chloral—Opium,
Morphine, Laudanum,
Paregoric, and Soothing Sirups—Tobacco,
Strychnine, etc. |
|
| VII. |
Food Poisons |
147 |
| |
Poisons in Shellfish and Other Food—Symptoms
and Remedies—How Bacteria
are Nourished—Infected Meat and Milk[Pg 3]—Treatment
of Tapeworm—Trichiniasis—Potato
Poisoning. |
|
| VIII. |
Bites and Stings |
155 |
| |
Country and City Mosquitoes—How Yellow
Fever is Communicated—Treatment
of Mosquito Bites—Bee, Wasp, and Hornet
Stings—Lice—Fleas and Flies—Centipedes
and Scorpions—Spiders—Poisonous
Snakes—Cat and Dog Bites. |
|
| IX. |
Burns, Scalds, Frostbites, Etc. |
171 |
| |
General Rules for Treating Burns and
Scalds—Hints on Dressings—Burns
Caused by Acids and Alkalies—Remedies
for Frostbite—Care of Blisters and Sores—Chilblains—Ingrowing
Toe Nails—Fainting
and Suffocation—Fits. |
|
PART II
| CHAPTER |
|
PAGE |
| I. |
Contagious Maladies |
191 |
| |
Symptoms and Treatment of Scarlet Fever—Diagnosis—Duration
of Contagion—Difference
Between True and German
Measles—Smallpox—Cure a Matter of
Good Nursing—Chickenpox. |
|
| II.[Pg 4] |
Infectious Diseases |
221 |
| |
Typhoid Fever—Symptoms and Modes of
Communication—Duration of the Disease—The
Death Rate—Importance of Bathing—Diet—Remedies
for Whooping
Cough—Mumps—Erysipelas. |
|
| III. |
Malaria and Yellow Fever |
247 |
| |
Malaria Caused by Mosquitoes—Distribution
of the Disease—Severe and Mild
Types—Prevention and Treatment—Yellow
Fever not a Contagious Disease—Course
of the Malady—Watchful Care and
Diet the only Remedies. |
|
[Pg 5]
INDEX
To First Aid and General Topics
Note.—The Roman numerals I, II, III, IV, V, and VI indicate the
volume; the Arabic figures 1, 2, 3, etc., indicate the page number.
Abrasions, I, 64
Abscess, alveolar, II, 58
Acids, burns by, I, 176, 177
poisoning by, I, 140
Acne, II, 145
Adenoids, II, 61
Adulterated food, tests for, V, 91
Adulteration of food, V, 87
Ague, I, 247
cake, I, 254
Air-bath, the, IV, 159
Albumen, IV, 262
Alcohol, use of, IV, 44, 153
Alcoholic drinks, IV, 153
Alcoholism, III, 47, 52
Algæ, remedy for, V, 56
Alkalies, burns by, I, 177
poisoning by, I, 140
Amenorrhœa, III, 75
Anæmia, III, 174
Ankle, sprain of, I, 65, 67, 68
Ankle-joint fracture, I, 115
Antitoxin, II, 77
Apoplexy, III, 49
Appendicitis, III, 256
Arm, fracture of, I, 91
Arteries, systemic, III, 168
Artery, bleeding from an, I, 51, 52
Arthritis, II, 177
Artificial respiration, I, 28
Asthma, II, 104
Astigmatism, II, 26
Athletics, home, IV, 69
Auricles of the heart, III, 168
BABY, bathing the, III, 109
care of the, III, 108
clothing of the, III, 110
diet for the, III, 134
food for the, III, 132; IV, 261
nursing the, III, 114
teething, III, 113
temperature of the, III, 110
weaning the, III, 117
weighing the, III, 112
Bacteria, destruction of, V, 238–253
in food, I, 147–154
in soil, V, 135
Baldness, II, 167; IV, 21
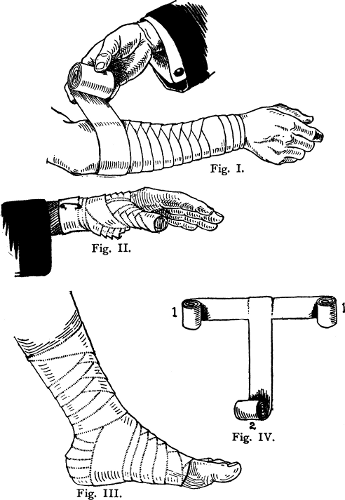
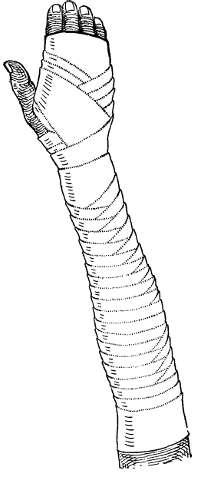
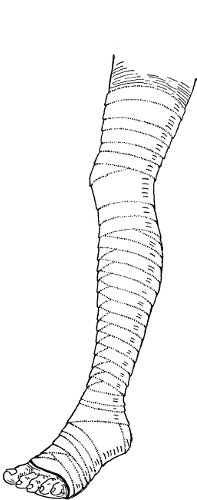
BANDAGES, I, 133
forms of, I, 132, 134, 136, 137
for bruises, I, 62–64
for fractures, I, 83–117
for sprains, I, 65–72
for wounds, I, 51–61
Barley water, IV, 263
Bathing, indoor, IV, 19, 155
outdoor, IV, 16
in convulsions, III, 35
in malaria, I, 259
in pneumonia, II, 94
in scarlet fever, I, 197
[Pg 6]in skin irritations, II, 140
in smallpox, I, 216
in typhoid fever, I, 231
in yellow fever, I, 266
BATHS, cold, IV, 15
foot, IV, 157
hot, IV, 19, 156
tepid, IV, 19
Turkish, IV, 20, 159
warm, IV, 19
Bed sores, I, 233
Bed-wetting, II, 213
Bee stings, I, 158
Beef, broth, IV, 261
juice, IV, 262
parts of, IV, 198
scraped, IV, 262
tea, IV, 261
Bellyache, III, 247
Bilious fever, I, 247
Biliousness, III, 184
BITES, cat, I, 170
dog, I, 170
flea, I, 162
fly, I, 164
lice, clothes, I, 161
lice, crab, I, 162
lice, head, I, 160
mosquito, I, 155
snake, I, 166
spider, I, 164
tarantula, I, 164
wood tick, I, 159
Black eye, II, 14
Blackheads, II, 145
Black water fever, I, 256
Bladder, inflammation of the, II, 215
stone in the, III, 264
BLEEDING, from an artery, I, 51, 52
from a vein, I, 51, 52
from punctured wounds, I, 52, 53
from the lungs, I, 62
from the nose, I, 61
from the scalp, I, 60
from the stomach, I, 62
from the womb, III, 82
Blood, deficiency of, III, 174
oozing of, I, 54
Bloody flux, III, 222
Boils, II, 157
Bottles, milk, III, 128
Bowel, prolapse of the, III, 143
BOWELS, catarrh of the, III, 205
diseases of the, III, 205
inflammation of the, III, 252
obstruction of the, III, 268
passages from the, IV, 247
Bowleg, III, 162
Brain, anatomy of the, III, 22
arteries of the, III, 22
autopsies of the, II, 230
Breasts, care of, after childbirth, III, 105
inflammation of the, III, 140
Breath, holding the, III, 153
Breathing, how to test the, IV, 248
to produce artificial, I, 28, 34, 43, 178, 186
Bright's disease, acute, II, 220
chronic, II, 222
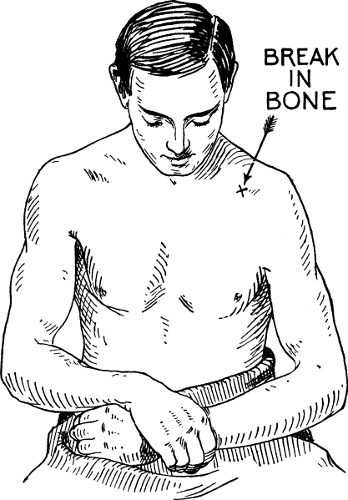
BROKEN BONE, I, 80
ankle, I, 115
arm, I, 91
collar bone, I, 85
finger, I, 101
forearm, I, 94
hand, I, 101
hip, I, 104
how to tell a, I, 80
jaw, I, 89
kneepan, I, 109
leg, I, 111
rib, I, 83
shoulder blade, I, 91
thigh, I, 106
wrist, I, 99
Bronchial tubes, diseases of the, II, 87
Bronchitis, II, 88, 91
[Pg 7]Broth, beef, IV, 261
chicken, IV, 261
clam, IV, 263
mutton, IV, 261
oyster, IV, 267
veal, IV, 261
BRUISES, bandages for, I, 63
treatment of, I, 62, 63
Bunion, I, 72
BURNS, I, 171
about the eyes, II, 16
from acids, I, 176
from alkalies, I, 177
from electric shock, I, 45
first class, I, 172
second class, I, 172
third class, I, 173
severe, I, 174
Callus of the skin, II, 156
Camp comfort (See Contents VI)
Camp cookery (See Contents VI)
Camp cure (See Contents VI)
CAMPING, in the North Woods, VI, 195
in the Western Mountains, VI, 214
outfit, VI, 212
Cancer, II, 123
of the breast, II, 124
of the lip, II, 125
of the stomach, II, 125
of the womb, II, 125
Canker, II, 68
Capillaries, systemic, III, 168
Carbuncle, II, 161
Carotid arteries, III, 22
Catarrh, II, 41, 54, 55
of the bowels, III, 205
effect of, on the ears, II, 38, 41
of the stomach, III, 185
Catarrhal deafness, II, 39
inflammation of eye, II, 18
Cat bite, I, 170
Catheter, how to use a, II, 219; IV, 252
Centipede sting, I, 164
Cereals as food, IV, 35, 229
Cerebellum, III, 22
Cerebral arteries, III, 22
Chafing, II, 142
Chagres fever, I, 256
Change of life, III, 70
Chapping, II, 142
Chicken broth, IV, 261
Chickenpox, I, 217
Chilblains, I, 182
Childbed fever, III, 107
Childbirth, after-pains in, III, 105
articles needed during, III, 96
bleeding after, III, 86
care after, III, 103
care in, III, 98
CHILDREN, DISEASES OF, III, 140
adenoids, II, 61
bed-wetting, II, 213
bowel, prolapse of the, III, 143
bowels, catarrh of the, III, 209
bowleg, III, 162
breath, holding the, III, 153
breasts, inflammation of the, III, 140
chickenpox, I, 217
cholera infantum, III, 211
chorea, III, 155
colic, III, 267
constipation, III, 238
convulsions, III, 34
cord, bleeding of the, III, 142
cough, II, 91
croup, II, 83
diarrhea, III, 208, 209
diphtheria, II, 77
dysentery, III, 213
epilepsy, III, 39
earache, II, 48
fever, III, 146
food for, III, 132–139
foreskin, adhering, III, 141
glands, enlarged, III, 149
hip disease, III, 161
[Pg 8]holding the breath, III, 153
knock knees, III, 163
larynx, spasm of the, III, 153
measles, I, 198
German measles, I, 203
membranous croup, II, 79
milk poisoning, III, 209, 211
mumps, I, 235
navel, sore, III, 142
pains, growing, III, 146
Pott's disease, III, 157
rickets, III, 151
ringworm, II, 149
rupture, II, 128
scarlatina, I, 192
scarlet fever, I, 192
scrofula, III, 149
scurvy, II, 182
sore mouth, II, 65
spine, curvature of the, III, 157, 159
St. Vitus's Dance, III, 155
stomach, catarrh of the, III, 209
urine, painful passage of, III, 141
urine, retention of, III, 141
wasting, III, 144
whooping cough, I, 238
worms, III, 240
Chills and fever, I, 247
Cholera, III, 228
infantum, III, 211
morbus, III, 226
Chorea, III, 158
Cinder in the eye, I, 176; II, 13
Circulation, the, III, 168
Circumcision, III, 142
Clam broth, IV, 263
Climacteric, the, III, 70
Clothing, proper, IV, 22
Cochlea, II, 46
Coffee, use of, IV, 43
Cold, exposure to, I, 181
in the head, II, 55
sore, II, 147
COLIC, III, 247
gallstone, III, 261
in babies, III, 267
intestinal, III, 249
mucous, III, 219
renal, III, 263
Collar-bone fracture, I, 85
Complexion, the, IV, 20
Confinement, III, 97
Congestion of the eyelid, II, 17
Conjunctivitis, II, 16, 18
Constipation, in adults, III, 233
in children, 238
Consumption, II, 96
fresh-air treatment for, II, 102
outdoor life for, VI, 72
prevention of, II, 104
Contagion, in cholera, 229
in conjunctivitis, II, 19
in diphtheria, II, 80
in eruptive fever, I, 191–220
in gonorrhea, II, 199
in grippe, II, 108
in mumps, I, 236
in syphilis, II, 206, 209
in whooping cough, I, 238
CONTAGIOUS DISEASES, I, 191
Convalescence (See Contents VI)
Convulsions, in children, III, 34
in adults, I, 188
COOKING (See Contents IV)
baking, IV, 171
boiling, IV, 180
braising, IV, 182
broiling, IV, 172
camp, VI, 220
cereals, IV, 229
eggs, IV, 184
entrées, IV, 219
fish, IV, 188
frying, IV, 175
game, IV, 202
poultry, IV, 202
roasting, IV, 171
sauces, IV, 216
[Pg 9]sautéing, IV, 174
shellfish, IV, 195
soups, IV, 207
stewing, IV, 181
time of, IV, 177
utensils, IV, 232
vegetables, IV, 223
Copper sulphate method, V, 52
Copper vessels, use of, V, 67
Cord, bleeding of the, III, 142
Corns, II, 154
Costiveness, III, 233
COUGH, acute, II, 87, 91
whooping, I, 238
Cricoid cartilage, II, 70
Cross eye, II, 33
Croup, membranous, II, 79
ordinary, II, 83, 92
Curvature of the spine, III, 157, 159
Cystitis, II, 215
Dandruff, II, 167
Deafness, catarrhal, II, 39
chronic, II, 36
temporary, II, 33
Delirium tremens, III, 50
DIARRHEA, acute, III, 205
chronic, III, 217
of children, III, 208, 209
DIET, IV, 26, 107, 123, 138, 153
animal, IV, 39
details of, IV, 146
errors of, IV, 107
for babies, III, 132
for brain workers, IV, 126
for long life, IV, 107
for the aged, IV, 112
proper, IV, 138
relation to climate, IV, 108
rules for, IV, 110, 123
simplicity of, IV, 138
vegetable and animal, IV, 39
Digestion, effect of dress on, IV, 42
hygiene of, IV, 26
processes of, IV, 28
Diphtheria, II, 77
DISINFECTANTS, chemical, V, 243
physical, V, 240
solutions for, V, 247
Disinfection, V, 238
of rooms, V, 249
DISLOCATIONS, elbow, I, 125
hip, I, 129
jaw, I, 118, 120
knee, I, 119
shoulder, I, 122
Dog bite, I, 170
Doses of drugs, IV, 255
Dressings, for bruises, I, 63, 64
for wounds, I, 53, 57
surgical, I, 131
Drink, nutritious, IV, 118
Drinking, steady, III, 52
DROWNED, arousing the, I, 27
producing respiration in the, I, 28, 34
restoring the, I, 27
saving the, I, 36
Drowning person, death grasp of a, I, 37
saving a, I, 36
swimming to relief of a, I, 36
Drugs, doses of, IV, 255
Drum membrane, II, 33, 43, 45, 46, 48
Dysentery, in adults, III, 222
in children, III, 213
Dysmenorrhea, III, 71
DYSPEPSIA, III, 185
causes of, IV, 27
nervous, III, 190
EAR, anatomy of the, II, 33, 37, 46
diseases of the, II, 33
foreign bodies in the, I, 78; II, 39
water in the, II, 42
wax in the, II, 35
Earache, II, 40
moderate, II, 48
[Pg 10]Eating, proper mode of, IV, 140–149
Eczema, II, 163
climatic, II, 164
occupation, II, 164
seborrheic, II, 164, 165, 167
Eggnog, IV, 268
Eggs, as food, IV, 33, 184
soft-boiled, IV, 266
Egg water, IV, 262
Elbow, dislocation of, I, 125
ELECTRIC SHOCK, I, 43, 46
Enteric fever, I, 221
Enteritis, catarrhal, III, 205
Entero-colitis, III, 209
Enteroptosis, IV, 43
Environment, importance of, III, 65
Epiglottis, II, 70
Epilepsy, III, 39
spasms in, III, 39
without spasms, III, 40
Erysipelas, I, 244
Eustachian tube, II, 37, 38, 41, 46, 49, 50
Exhaustion, mental and nervous, VI, 91–145
EXERCISE, IV, 48, 66
corrective, IV, 57
effect of, IV, 51
excessive, IV, 52
for all-round development, IV, 59, 101
for boyhood, IV, 69
for children, IV, 67
for elderly men, IV, 79
for everyone, IV, 66
for girls, IV, 73
for middle-aged men, IV, 77
for women, IV, 76
for young men, IV, 71
for youth, IV, 69
home, IV, 57
regular, IV, 53, 58
results of, IV, 98
without apparatus, IV, 57
EYE, anatomy of the, II, 30
astigmatism of the, II, 26 black, II, 14
catarrhal inflammation of the, II, 18
cinder in the, I, 76
cross, II, 33
diseases of the, II, 13
farsighted II, 21
foreign bodies in the, I, 76; II, 13
hyperopic, II, 22
lens of the, II, 30
muscles of the, II, 30
nearsighted, II, 25
pink, II, 19
retina of the, II, 30
sore, II, 16
strain, II, 21
wounds and burns of the, II, 16
Eyelid, congestion of the, II, 17
stye on the, II, 15
twitching of the, II, 15
Eye muscles, weakness of the, II, 28
Eye-strain, II, 21
Facial, neuralgia, III, 28
paralysis, III, 25
FAINTING, I, 185; III, 45
Farsightedness, II, 21
Fat as a food, IV, 35
Fatigue, causes of, IV, 50
Felon, I, 74, 75
FEVER, bilious, I, 247
black water, I, 256
Chagres, I, 256
chills and, I, 247
enteric, I, 221
gastric, III, 179
intermittent, I, 247
marsh, I, 247
remittent, I, 247
rheumatic, II, 169
scarlet, I, 192
swamp, I, 247
typhoid, I, 221
yellow, I, 261
Fever blister, II, 147
[Pg 11]Fevers, eruptive contagious, I, 191
Fish as food, IV, 188
Finger, fracture of, I, 101
FIT, I, 188
Flea bites, I, 162
Fly bites, I, 164
Food, adulteration of, V, 87
containing parasites, I, 152
elements of, IV, 29
for babies, III, 132; IV, 261
for the sick, IV, 261
infected, I, 150
laws, V, 88
poisoning, I, 147
preparation of, IV, 171
pure, selection of, V, 89
Foods, advertised, IV, 116
Foot gear, IV, 24
Forearm fracture, I, 94
FOREIGN BODIES, in the ear, I, 78; II, 39
in the eye, I, 76; II, 13
in the nose, I, 79; II, 53
Foreskin, adhering, III, 141
Fourth-of-July accidents, I, 56
FRACTURE (See Broken Bone)
Colles', I, 99
compound, I, 80, 116
how to tell a, I, 81
simple, I, 80
Freckles, II, 150
Freezing, I, 178
FROSTBITE, I, 178, 180
Gallstone colic, III, 261
Ganglion, I, 75
Garbage, disposal of, V, 171
Gastric fever, III, 179
Genito-urinary diseases, II, 199
Germs (See Bacteria)
Girls, exercises for, IV, 73
physical training for, IV, 72; VI, 39
Glands, enlarged, III, 149
Gonorrhea, II, 199
in women, II, 203; III, 90
Gout, common, II, 183
rheumatic, II, 177
Grippe, la, II, 56, 108
Growing pains, III, 146
Hair, the, IV, 21
Hallucinations, II, 232
Hand, anatomy of the, III, 30
arteries of the, III, 30
fracture of the, I, 101
nerves of the, III, 30
tendons of the, III, 30
HEADACHE, constant, II, 120
due to disease, II, 117
due to eye strain, II, 29
due to heat stroke, II, 120
due to indigestion, II, 115
due to poisoning, II, 118
nervous, II, 117
neuralgic, II, 117
sick, II, 113
sympathetic, II, 116
Head gear, IV, 24, 160
Head injuries, III, 46
HEART, anatomy of the, III, 167, 168
enlargement of the, III, 169
palpitation of the, III, 171
Heart disease, III, 167
Heat exhaustion, I, 39, 40
Heating, cost of, V, 254
methods of, V, 161
HEAT STROKE, I, 39, 41
Hemorrhage (See Bleeding)
Hemorrhoids, II, 135
Heredity, III, 57
in consumption, II, 97
Hernia, II, 128 (See Rupture)
strangulated, II, 129
umbilical, II, 128
ventral, II, 128
Hiccough or hiccup, III, 21
Hip disease, III, 161
Hip, dislocation of, I, 129
fracture of, I, 104
Hives, II, 143
[Pg 12]Hoarseness, II, 80
Hornet stings, I, 158
"Horrors," the, III, 50
House, proper construction of, V, 141
Housemaid's knee, I, 72
Hypodermic syringe, the, IV, 250
Hysteria, VI, 20
INDIGESTION, acute, III, 178
a result of errors, IV, 130
chronic, III, 185
intestinal, III, 202
not disease, IV, 134
Infants, bathing, III, 109
care of, III, 108
clothing for the, III, 110
feeding of, III, 118
Infection, V, 238
in erysipelas, I, 244
in malaria, I, 247
in typhoid fever, I, 221
in yellow fever, I, 261
INFECTIOUS DISEASES, I, 221
Influenza, II, 108
Ingrowing toe nail, I, 184
Injections, III, 238, 239
INJURED, CARRYING THE, I, Frontispiece
Insane, criminal, II, 234
delusions of the, II, 233
illusions of the, II, 231
sanitariums for the, II, 245
Insanity, II, 229; VI, 164
causes of, II, 239
false ideas regarding, II, 241
physical signs of, II, 235
prevention of, II, 240
types of, II, 236
Insensibility, III, 44
Insomnia, III, 23
Intermittent fever, I, 247
Invalids, care of, VI, 155
Itching, II, 139
Ivy poison, II, 152
Jaundice, III, 180
Jaw, dislocation of, I, 118, 120
fracture of, I, 89
Joint, injury of a, I, 65, 69
Junket, IV, 266
Kerosene, extermination of mosquitoes by, V, 77
Kidneys, inflammation of the, II, 220
Bright's disease of the, II, 219
stone in the, III, 265
Knee, dislocation of, I, 119
sprain of, I, 67, 70
Kneepan fracture, I, 109
Knock knees, III, 163
Laryngitis, II, 80
Larynx, anatomy of the, II, 70
spasm of the, III, 153
Leeches, use of, II, 43
Leg bones, fracture of, I, 111, 116
Leucorrhœa, III, 86
Lice, body, I, 161
clothes, I, 161
crab, I, 162
head, I, 160
Life-saving service, U. S., I, 27
Lightning stroke, I, 43
Limewater, IV, 268
LOCKJAW, I, 56
Long life, rules for (See Contents IV, Part III)
Lotions, II, 145, 151, 152, 155, 166
Lues, II, 206
Lumbago, II, 173
LUNGS, bleeding from the, I, 62
diseases of the, II, 87
inflammation of the, II, 93
tuberculosis of the, II, 96
MALARIA, I, 247
chronic, I, 253
mosquito as cause of, I, 157, 247
pernicious, I, 255
remittent, I, 254
[Pg 13]Malt soup, IV, 267
Marasmus, III, 144
Marketing, hints on, IV, 232
Marriage relations, II, 197
Marsh fever, I, 247
Measles, common, I, 198
German, I, 203
Meat as food, IV, 32
Median nerve, III, 30
Medicine chest, contents of the, IV, 243
MEDICINES, PATENT, II, 245
antiphlogistine, II, 258
belladonna plasters, II, 257
dangers of, II, 260
hamamelis, II, 255
headache powders, II, 262
Listerine, II, 256
Platt's Chlorides, II, 259
Pond's Extract, II, 255
proprietary, II, 246
Scott's Emulsion, II, 257
vaseline, II, 254
witch-hazel, II, 255
Medulla oblongata, III, 22
Membranous croup, II, 79
Menopause, the, III, 70
Menstruation, III, 67
absence of, III, 75
arrest of, III, 79
cessation of, III, 78
delayed, III, 79
painful, III, 71
scanty, III, 79
Metals, poisoning by, I, 141
Miliaria, II, 148
MILK, as food, IV, 33
curd, IV, 266
mixtures, III, 124
peptonized, IV, 264
poisoning, III, 209, 211
porridge, IV, 267
Mind cure, VI, 31
disorder of the, II, 229
Miscarriage, danger of, III, 80
MOSQUITO bites, I, 155, 158; V, 71
destruction of the, I, 258; V, 75
exterminating the, V, 70
malaria due to the, I, 248
yellow fever due to the, I, 261; V, 70
Motor nerve, III, 38
Mouth-breathing, II, 60
Mouth, inflammation of the, II, 64
sore, II, 64
Mumps, I, 235
Muscular action, IV, 48
development, by will power, IV, 63
MUSHROOM POISONING, V, 112
Mushrooms, edible, V, 115
how to tell, V, 114
poisonous, V, 124
Mutton broth, IV, 261
Myalgia, II, 173
Myopia, II, 25
Narcotics, poisoning by, I, 142
Nasal cavity, II, 54
Navel, sore, III, 142
Nearsightedness, II, 25
Nervous debility, III, 13
diseases, III, 13
exhaustion, III, 13; VI, 70, 167
NERVOUSNESS (See Contents VI)
remedy for, VI, 70, 167; III, 20
Nervous system, reflex action of the, III, 38
Nettlerash, II, 143
Neuralgia, III, 27
facial, III, 28
of the chest, III, 29
Neurasthenia, III, 13
NOSE, anatomy of the, II, 54
bleeding from the, II, 51
catarrh of the, II, 55
diseases of the, II, 51
foreign bodies in the, I, 79; II, 53
obstructions in the, II, 60
septum of the, II, 51, 54, 61
[Pg 14]Nosebleed, I, 61; II, 51
Nostrum, II, 248
Nurse and patient (See Contents VI)
Nurse, selection of the, VI, 150
Nursing, VI, 146
Oatmeal water, IV, 263
Olfactory nerves, III, 22
Oozing of blood, I, 54, 55
Optic nerves, III, 22
OUTDOOR LIFE (See Contents VI)
for consumption, VI, 72
for nervous exhaustion, VI, 70, 167
Overworked, hints for the, VI, 91
Oyster broth, IV, 267
Palmar arch, III, 30
Pains, growing, III, 146
Palpitation of the heart, III, 171
Paralysis, facial, III, 25
Paranoia, II, 237
Parasites, malarial, I, 247
yellow fever, I, 261
Paresis, II, 237
Patent medicines, II, 247
Peritonitis, III, 252
Petit mal, III, 40
Pharyngitis, II, 69
Phthisis, II, 96
Pigeon breast, II, 63
Piles, external, II, 135
internal, II, 136
Pimples, II, 145
Pink eye, II, 19
Plumbing, connections, V, 194
defects in, V, 231
drains, V, 206
fixtures, V, 216
joints, V, 194
pipes, V, 191, 206
tests, 233
traps, V, 198
Pneumonia, II, 93
POISONING (See Poisons)
by canned meats, I, 150
by fish, I, 148
by meat, I, 148, 150, 151
by milk, I, 148, 150, 151
food, bacterial, I, 147
food, containing parasites, I, 152
food, infected, I, 150
mushroom, V, 112
potato, I, 154
Poison ivy, II, 152
POISONS, acetanilid, I, 146
acid, carbolic, I, 140
acid, nitric, I, 140
acid, oxalic, I, 140
acid, sulphuric, I, 140
acids, I, 140
aconite, I, 142
alcohol, I, 143
alkalies, I, 140
ammonia, I, 141
antidotes, I, 139
antimony, I, 142
arsenic, I, 141
belladonna, I, 142
bichloride of mercury, I, 141
blue vitriol, I, 141
bug poison, I, 141
camphor, I, 142
caustic soda, I, 141
chloral, I, 143
cocaine, I, 145
copper, I, 141
corrosive sublimate, I, 141
digitalis, I, 142
ergot, I, 142
Fowler's solution, I, 141
headache powders, I, 146
hellebore, I, 142
ivy, II, 152
knockout drops, I, 143
laudanum, I, 144
lobelia, I, 142
lye, I, 141
matches, I, 142
mercury, I, 141
[Pg 15]metals, I, 141
morphine, I, 144
narcotics, I, 142
nux vomica, I, 145
opium, I, 144
paregoric, I, 144
Paris green, I, 141
phenacetin, I, 146
phosphorus, I, 142
potash, I, 141
"rough on rats," I, 141
silver nitrate, I, 141
sleeping medicines, I, 143
soothing sirup, I, 144
strychnine, I, 145
tartar emetic, I, 142
tobacco, I, 144
unknown, I, 139
verdigris, I, 141
washing soda, I, 141
white precipitate, I, 141
Polypi, II, 54, 62
Pons Varolii, III, 22
Pott's disease, III, 157
Poultry as food, IV, 201
Pox, II, 206
Pregnancy, III, 91
diet during, III, 91
exercise during, III, 91
mental state during, III, 95
signs of, III, 80, 93
Prickly heat, II, 148
Proprietary medicines, II, 248
Pruritus, II, 139
Pulse, how to feel the, IV, 247
Punctured wound, bleeding from, a, I, 52, 53
Pure food bill, II, 249
PURE FOOD, SELECTION OF, V, 89–111
canned articles, V, 107
cereals, V, 98
chocolate, V, 107
cocoa, V, 107
coffee, V, 104
flavoring extracts, V, III
meat, V, 92
meat products, V, 95
olive oil, V, 110
shellfish, V, 94
spices, V, 108
sugar, V, 108
tea, V, 104
vegetables, V, 96
vinegar, V, 110
Purifying water supply, V, 52
Quinsy, II, 75
Radial nerve, III, 30
Recipes, for babies, IV, 261
for the sick, IV, 261
Reflex action illustrated, III, 38; IV, 49
Remittent fever, I, 247
Renal colic, III, 263
Respiration, to produce artificial, I, 28, 34, 43, 178, 186
Respirations, counting the, IV, 248
Rest cure, III, 20
Reversion, III, 59
Rheumatic fever, II, 169
gout, II, 177
RHEUMATISM, acute, II, 169
chronic, II, 175
effect on the heart, II, 170
inflammatory, II, 169
muscular, II, 173
of the chest, II, 174
Rhinitis, II, 77
Rib, broken, I, 83
Rice water, IV, 264
Rickets, III, 151
Ringworm, of body, II, 149
of scalp, II, 149
RUN-AROUND, I, 73
Rupture, II, 128
Salt rheum, II, 163
Sanitariums for the insane, II, 245
SANITATION (See Contents V)
Sarcoma, II, 124
[Pg 16]SCALDS, I, 171
Scalp wounds, I, 60
Scarlatina, I, 192
Scarlet fever, I, 192
Sciatica, III, 31
Scorpion sting, I, 164
Scrofula, III, 149
Scurvy, common, II, 180
infantile, II, 182
Seasickness, III, 195
Self-abuse, II, 192
Semicircular canals, II, 46
Sensory nerve, III, 38
Septum, II, 54
deviation of the, II, 60
Serum, antivenomous, I, 169
Sewage, V, 170
disposal of, V, 172
Sewer gas, V, 187
Sewers, V, 182
Sexual organs, care of the, II, 191
diseases of the, II, 199
Sexual relations, II, 194
Shingles, III, 29
Shoulder, dislocation of, I, 122
sprain of, I, 67
Shoulder-blade fracture, I, 91
Sick, food for the, IV, 261
Sick room, the, VI, 150
SKIN, callus of the, II, 156
chafing of the, II, 142
chapping of the, II, 142
cracks in the, II, 156
discolorations of the, II, 150
diseases of the, II, 139
irritation of the, II, 142
itching of the, II, 139
Sleeplessness, III, 23
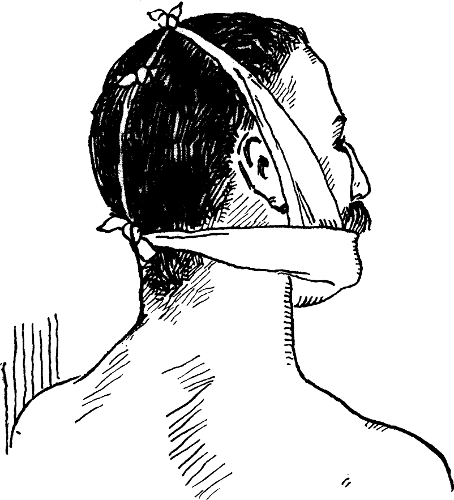
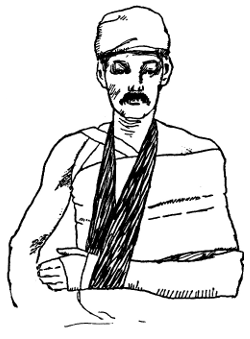
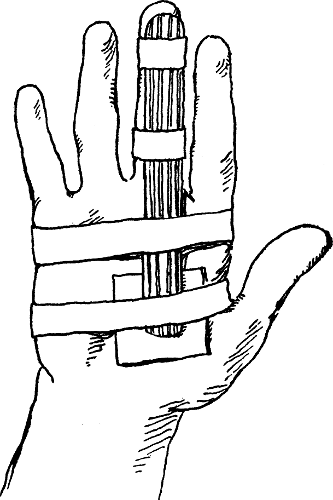
Sling, how to make a, 87, 88
Smallpox, I, 206
Snake bite, I, 166, 168
Soap, use of, IV, 32
Soil, bacteria in, V, 135
constituents of, V, 131
contamination of, V, 136
diseases due to, V, 139
Soil, improving the, V, 140
influence of, V, 137
Sore mouth, aphthous, II, 66
gangrenous, II, 67
simple, II, 65
ulcerous, II, 67
Sore eyes, II, 16
Sore throat, II, 69
Soup, malt, IV, 267
Soups, IV, 207
Spider bite, I, 164, 165
Spinal cord, III, 38
Spine, curvature of, III, 157, 159
Spleen, enlargement of, II, 254
Splinters, removing, I, 54
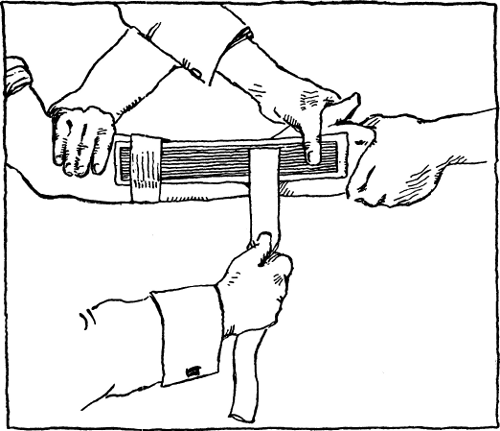
Splints, I, 61, 71, 93, 97, 102, 107, 110, 111, 114, 128
SPRAINS, bandages for, I, 65, 67
treatment of, 65, 66
Sprue, II, 66
Squint, II, 33
St. Vitus's Dance, III, 155
Stiff neck, II, 174
STINGS, bee, I, 158
centipede, I, 164
hornet, I, 158
scorpion, I, 164
wasp, I, 158
Stitching a wound, I, 58
STOMACH, bleeding from the, I, 62
catarrh of the, III, 185, 209
diseases of the, III, 178
neuralgia of the, III, 251
Stomachache, III, 247
Stone, in the bladder, III, 265
in the kidney, III, 263
Strabismus, II, 33
Stye, II, 15
SUFFOCATION, from gas, I, 186
Sunstroke, I, 40
Surgical dressings, I, 131
Swamp fever, I, 247
SYNOVITIS, I, 69
Syphilis, II, 206, 212
Syringe, the bulb, III, 239
[Pg 17]the fountain, III, 238
the hypodermic, IV, 250
Tan, II, 150
Tapeworm, I, 152
Tarantula bite, I, 164
Tea, use of, IV, 43
Teeth, artificial, IV, 119
care of the, IV, 26
Teething, III, 113
Temperature, how to tell the, IV, 246
proper, IV, 161, 162
Tetter, II, 163
Thermometer, clinical, use of the, IV, 246
Thigh-bone fracture, I, 106
THROAT, diseases of the, II, 51,
sore, II, 69
Thrush, II, 66
Tic douloureux, III, 28
Toe nail, ingrowing, I, 184
Tongue, noting appearance of the, IV, 249
Tonsilitis, II, 71
Tonsils, enlarged, II, 63
Tooth, ulcerated, II, 58
Toothache, II, 58
Training, physical, IV, 124; VI, 38
Trichiniasis, I, 153
Truss, use of the, II, 130
Tuberculin, II, 101
Tuberculosis of the bones, III, 157
of the lungs, II, 96
TUMORS, II, 123
Turbinates, enlarged, II, 60
Typhoid fever, I, 221
complications of, I, 228
Ulcerated tooth, II, 58
Ulnar nerve, III, 30
UNCONSCIOUSNESS, III, 44
due to drunkenness, III, 47
due to epilepsy, III, 48
due to fainting, III, 45
due to head injuries, III, 46
Unconsciousness, due to kidney disease, III, 48
due to opium poisoning, III, 48
due to sunstroke, III, 48
Underclothing, proper, IV, 22
URINE, incontinence of, II, 213
involuntary passage of, II, 213
painful passage of, III, 141
retention of, II, 218; III, 141
stoppage of, II, 218
suppression of, II, 218
Urticaria, II, 143
Vaccination, I, 211–215
Varicocele, II, 134
Varicose veins, II, 132
Varioloid, I, 211
Veal broth, IV, 261
Vegetables as food, IV, 34, 223
Vein, bleeding from a, I, 51, 52
Veins, systemic, III, 168
VENTILATION, artificial, V, 157
forces of, V, 148
methods of, V, 150
natural, V, 151
Ventricles of the heart, III, 168
Vision, defects of, II, 21–33
Vocal cords, II, 70
VOMITING, III, 194
of blood, III, 200
of indigestion, III, 199
of pregnancy, III, 196
Wakefulness, III, 23
Warming, V, 160
Warts, flat, II, 154
moist, II, 154
seed, II, 153
threadlike, II, 153
Wasp stings, I, 158
Wasting, III, 144
WATER, barley, IV, 263
egg, IV, 262
lake, V, 27
lime, IV, 268
oatmeal, IV, 263
[Pg 18]pure, V, 21, 52
rain, V, 26
rice, IV, 264
spring, V, 29
well, V, 31–37
wheat, IV, 264
Water cure, for nervous exhaustion, III, 20
Water distribution, V, 39
engines for, V, 42
hydraulic rams for, V, 40
pressure systems for, V, 47
storage tanks for, V, 46
windmills for, V, 41
Water supply, laws of, V, 37
plants which pollute, V, 54
pollution of, V, 22
purifying the, V, 52
sources of, V, 19
system for country, V, 47
Wax in the ear, II, 34
Wear and tear (See Contents VI)
Weaning, III, 117
WEEPING SINEW, I, 75
Wen, II, 126
Wheat water, IV, 264
Whey, mixtures, IV, 265
wine, IV, 266
Whites, III, 87
Whitlow, I, 74, 75
Whooping cough, I, 238
Womb, hemorrhage from the, III, 82
Women, exercises for, IV, 76
Wood tick, bite of, I, 159
WORMS, pin, III, 243
round, III, 242
tape, III, 245
WOUNDS, I, 50
about the eyes, II, 16
caused by pistols, I, 56
caused by firecrackers, I, 56
cleansing, I, 59
foreign bodies in, I, 54, 56
scalp, I, 60
stitching, I, 58
treatment of, I, 50, 57
Wrist, fracture of the, I, 99
sprain of the, I, 65, 67
Yellow fever, I, 261
mosquito as cause of, I, 157, 261, 265
[Pg 19]
Preface
Medicine, as the art of preserving and restoring health, is the
rightful office of the great army of earnest and qualified American
physicians. But their utmost sincerity and science are hampered by
trying restrictions with three great classes of people: those on whom
the family physician cannot call every day; those on whom he cannot
call in time; and those on whom he cannot call at all.
To lessen these restrictions, thus assisting and extending the
healer's work, is the aim of the pages that follow.
Consider first the average American household, where the family
physician cannot call every day. Not a day finds this household
without the need of information in medicine or hygiene or sanitation.
More efforts of the profession are thwarted by ignorance than by
epidemic. Not to supplant the doctor, but to supplement him, carefully
prepared information should be at hand on the hygiene of
health—sanitation, diet, exercise, clothing, baths, etc.; on the
hygiene of disease—nursing and sick-room conduct, control of the
nervous and insane, emergency resources, domestic remedies; above all,
on the prevention of disease, emphasizing the folly of self-treatment;
pointing out the danger of delay in seeking skilled medical advice
with[Pg 20] such troubles as cancer, where early recognition may bring
permanent cure; showing the benefit of simple sanitary precautions,
such as the experiment-stations method of exterminating the
malaria-breeding mosquito. The volumes treating of these subjects
cannot be made too clear, nontechnical, fundamental, or too well
guarded by the supervision of medical men known favorably to the
profession.
Again, the physician cannot come on time to save life, limb, or
looks to the victim of many a serious accident. And yet some bystander
could usually understand and apply plain rules for inducing
respiration, applying a splint, giving an emetic, soothing a burn or
the like, so as to safeguard the sufferer till the doctor's
arrival—if only these plain rules were in such compact form that no
office, store, or home in the land need be without them.
Finally, the doctor cannot come at all to hundreds of thousands of
sailors, automobilists, and other travelers, to ranchers, miners, and
country dwellers of many sorts. This third class has had, hitherto,
little choice between some "Practice of Medicine," too technical to be
helpful, on the one hand, and on the other, the dubious literature of
unsanctioned "systems"; or the startling "cure-all" assertions
emanating from many proprietors of remedies; or "Complete Family
Physicians," which offer prescriptions as absurd for the layman as
would be dynamite in the hands of a child, with superfluous and
loathsome pictures ap[Pg 21]pealing only to morbid curiosity, and with a
general inaccuracy utterly out of touch with twentieth-century
knowledge. What such people need, much more than the dwellers in
settled communities, is to learn the views of modern medicine upon the
treatment of the ever-present common ailments—the use of standard
remedies, cautions against the abuse of narcotics, lessons of
discrimination against harmful, useless, or expensive "patent
medicines," and proper rules of conduct for diet, nursing, and general
treatment.
Authentic health literature existed abundantly before the preparation
of these volumes, but it was scattered, expensive, and in most cases
not arranged for the widest use. Not within our knowledge has the body
of facts, most helpful to the layman on Sanitation and Hygiene, First
Aid, and Domestic Healing, been brought together as completely, as
clearly, as concisely, with a critical editing board so qualified, and
with special contributions so authoritative as this work exhibits.
"Utmost caution" has been a watchword with the editors from the start.
Those to whom the doctor cannot come every day have been repeatedly
warned of the follies of self-treatment, and reminded that to-day it
is the patient that is treated—not the disease. Those to whom the
doctor cannot come in time are likewise warned that the "First-aid
Rules" of this Library are for temporary treatment only, in all
situations where it is possible to get a physician. And the utmost[Pg 22]
conservatism has been striven for by the author and the several
revisers in every part of the work that appeals particularly to
dwellers in localities so removed that the doctor cannot come at
all. Especial delicacy was also sought in the treatment of a chapter
which, it is hoped, will aid parents to guide their children in sexual
matters. The illustrations represent helpful, normal conditions (with
the exception of some necessary representations of fracture, etc.)
with instructive captions aimed to make them less a sensation than a
real benefit; and no pictures appear of a sort to stimulate mere
morbid curiosity.
The greatest sympathy and appreciation of this work have been shown by
the progressive and recognized practitioners who have seen early
copies. They recognize it as a timely attempt to create and compile
health literature in a form most complete within its limits of space,
and in a manner most helpful and sane. The eager curiosity regarding
themselves that has been sweeping over the American people has been
diverted into frivolous and harmful channels by much reckless talk and
writing. A prominent newspaper, in its Sunday editions, recently took
up the assertion, in a series of articles, that appendicitis
operations resulted from a gigantic criminal conspiracy on the part of
surgeons; that a sufficient cure for appendicitis, "as any honest
doctor would tell you," is an injection of molasses and water! The
endless harm done by such outright untruth is swelled by a joining
stream of slapdash mis[Pg 23]information and vicious sensation, constantly
running through the press.
Education is sorely needed from authority. People will read about
their bodies. They have a right to information from the highest
accredited source. And to apply such knowledge Dr. Winslow has labored
for many years during his practicing experience, condensing and
setting into clear order the most vitally important facts of domestic
disease and treatment; an eminently qualified staff of practicing
specialists has coöperated, with criticism and supervision of
incalculable value to the reader; and the accepted classics in their
field follow: Dr. Weir Mitchell's elegant and inspiring essays on
Nerves, Outdoor Life, etc.; Sir Henry Thompson's "precious documents
of personal experience" on Diet and Conduct for Long Life; Dr. Dudley
A. Sargent's scientific and long-prepared system of exercises without
apparatus; Gerhard's clear principles of pure water supply; Dr.
Darlington's notes and editing from the unequaled opportunity of a New
York City Health Commissioner—and many other "special contributions."
It is the widely accepted modern medicine, and no school or "system,"
that is reflected here. While medicine, as a science, is far from
being perfect, partly because of faulty traditions and misinterpreted
experience, yet the aim of the modern school is to base practice on
facts. For example, for many years physicians were aware that
quinine cured malaria, in some unex[Pg 24]plainable way. Now they not only
know that malaria is caused by an animal parasite living and breeding
in the blood and that quinine destroys the foe, but they know about
the parasite's habits and mode of development and when it most readily
succumbs to the drug. Thus a great discovery taught them to give
quinine understandingly, at the right time, and in the right doses.
An educated physician has at his command all knowledge, past and
present, pertaining to medicine. He is free to employ any means to
better his patient. Now it is impossible to cure, or even better, all
who suffer from certain disease by any one method, and a follower of a
special "system" thus ignores many agencies which might prove
efficient in his case. While there is a germ of good and truth in the
various "systems" of medical practice, their representatives possess
no knowledge unknown to science or to the medical profession at large.
Many persons are always attracted by "something new." But newness in a
medical sect is too often newness in name only. These systems rise and
fall, but scientific, legitimate medicine goes ever onward with an eye
single to the discovery of new facts.
That these volumes will result in an impetus to saner, quieter,
steadier living, and will prove a helpful friend to many a physician
and many a layman, is the earnest wish of
The Publishers.
[Pg 25]
Part I
FIRST AID IN EMERGENCIES
BY
KENELM WINSLOW
AND
ALBERT WARREN FERRIS
[Pg 26]
Introductory Note
With the exception of the opening chapter, which contains the valuable
Life-saving Service Rules verbatim, the Editors have adopted the
plan of beginning each article in Part I of this volume with a few
simple, practical instructions, telling the reader exactly what to do
in case of an accident. For the purpose of distinguishing them from
the ordinary text, and making them easy of reference, these
"First-aid Rules" are printed in light-faced type.
[Pg 27]
CHAPTER I
Restoring the Apparently Drowned
As Practiced in the United States Life-Saving Service
Note.—These directions differ from those given in the last
revision of the Regulations by the addition of means for securing
deeper inspiration. The method heretofore published, known as the
Howard, or direct method, has been productive of excellent results
in the practice of the service, and is retained here. It is,
however, here arranged for practice in combination with the
Sylvester method, the latter producing deeper inspiration than any
other known method, while the former effects the most complete
expiration. The combination, therefore, tends to produce the most
rapid oxygenation of the blood—the real object to be gained. The
combination is prepared primarily for the use of life-saving crews
where assistants are at hand. A modification of Rule III, however,
is published as a guide in cases where no assistants are at hand
and one person is compelled to act alone. In preparing these
directions the able and exhaustive report of Messrs. J. Collins
Warren, M.D., and George B. Shattuck, M.D., committee of the
Humane Society of Massachusetts, embraced in the annual report of
the society for 1895–96, has been availed of, placing the
department under many obligations to these gentlemen for their
valuable suggestions.
IF SEVERAL ASSISTANTS ARE AT HAND.
Rule I. Arouse the Patient.—Do not move the patient unless in
danger of freezing; instantly expose the face to the air, toward the
wind if there be any; wipe dry the mouth and nostrils; rip the
clothing so as to expose the chest and waist; give two or three quick,
smarting slaps on the chest with the open hand.
[Pg 28]If the patient does not revive, proceed immediately as follows:
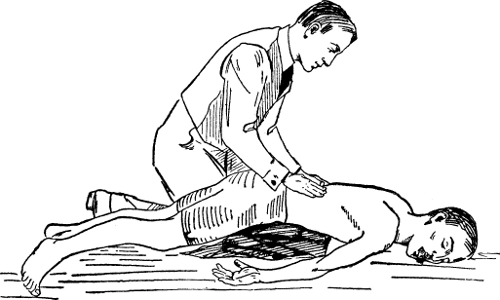
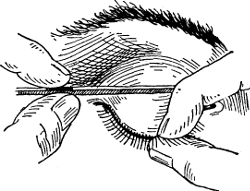
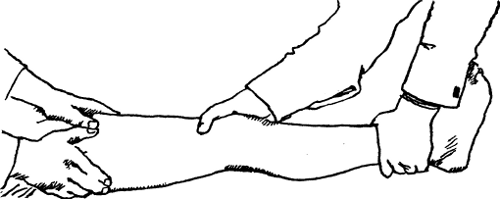
Rule II. To Expel Water from the Stomach and Chest (see Fig.
1).—Separate the jaws and keep them apart by placing between the
teeth a cork or small bit of wood, turn the patient on his face, a
large bundle of tightly rolled clothing being placed beneath the
stomach; press heavily on the back over it for half a minute, or as
long as fluids flow freely from the mouth.
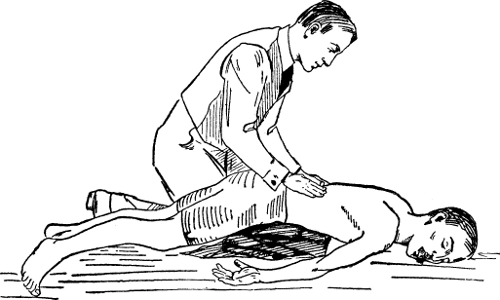 Fig. 1.
Fig. 1.
TO EXPEL WATER FROM STOMACH AND CHEST.
Patient lying face downward; roll of clothes beneath stomach; jaws
separated by piece of wood or cork; note rescuer pressing on back to
force out water.
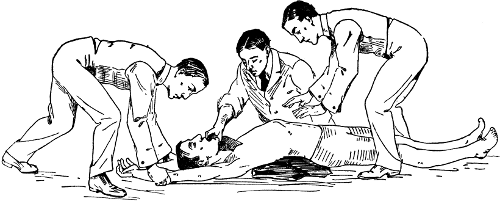
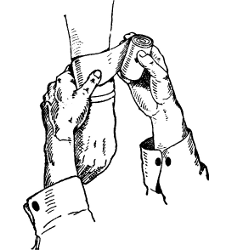
Rule III. To Produce Breathing (see Figs. 2 and 3).—Clear the mouth
and throat of mucus by[Pg 29] introducing into the throat the corner of a
handkerchief wrapped closely around the forefinger; turn the patient
on the back, the roll of clothing being so placed as to raise the pit
of the stomach above the level of the rest of the body. Let an
assistant, with a handkerchief or piece of dry cloth, draw the tip of
the tongue out of one corner of the mouth (which prevents the tongue
from falling back and choking the entrance to the windpipe), and keep
it projecting a little beyond the lips. Let another assistant grasp
the arms, just below the elbows, and draw them steadily upward by the
sides of the patient's head to the ground, the hands nearly meeting
(which enlarges the capacity of the chest and induces inspiration).
(Fig. 2.) While this is being done let a third assistant take position
astride the patient's hips with his elbows resting upon his own knees,
his hands extended ready for action. Next, let the assistant standing
at the head turn down the patient's arms to the sides of the body, the
assistant holding the tongue changing hands if necessary[1] to let the
arms pass. Just before the patient's hands reach the ground the man
astride the body will grasp the body with his hands, the balls of the
thumb resting on either side of the pit of the stomach, the fingers
falling into the grooves between the short ribs. Now, using his knees
as a pivot, he will, at the moment the patient's hands touch the
ground, throw (not too suddenly)[Pg 30]
[Pg 31]
[Pg 32] all his weight forward on his
hands, and at the same time squeeze the waist between them, as if he
wished to force something in the chest upward out of the mouth; he
will deepen the pressure while he slowly counts one, two, three, four
(about five seconds), then suddenly let go with a final push, which
will spring him back to his first position.[2] This completes
expiration. (Fig. 3.)
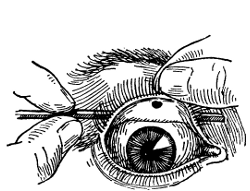
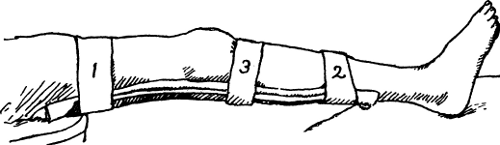
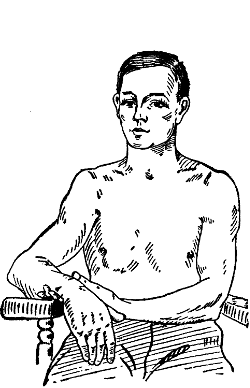
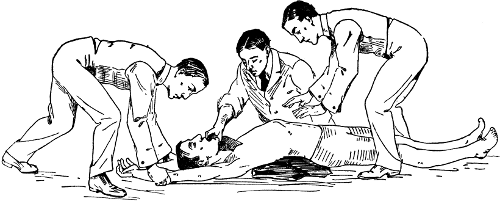 Fig. 2.
Fig. 2.
TO PRODUCE BREATHING.
First Position: Patient lying face upward; roll of clothes under back;
tongue pulled out of mouth with handkerchief; note rescuer drawing
arms upward to sides of head to start act of breathing in.
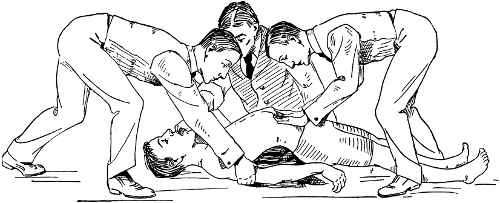
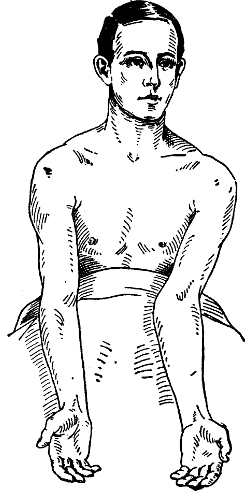
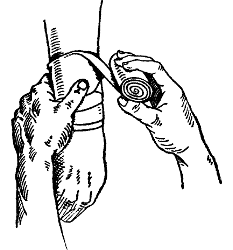
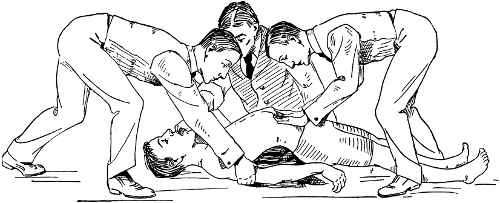 Fig. 3.
Fig. 3.
TO PRODUCE BREATHING.
Second Position: Forcing patient to breathe out; note rescuer with
thumbs on pit of stomach, pressing against front of chest over lower
ribs; also, assistant drawing down arms to body.
At the instant of his letting go, the man at the patient's head will
again draw the arms steadily upward to the sides of the patient's head
as before (the assistant holding the tongue again changing hands to
let the arms pass if necessary), holding them there while he slowly
counts one, two, three, four (about five seconds).
Repeat these movements deliberately and perseveringly twelve to
fifteen times in every minute—thus imitating the natural motions of
breathing.
If natural breathing be not restored after a trial of the bellows
movement for the space of about four minutes, then turn the patient a
second time on the stomach, as directed in Rule II, rolling the body
in the opposite direction from that in which it was first turned, for
the purpose of freeing the air passage from any remaining water.
Continue the artificial respiration from one to four hours, or until
the patient breathes, according to Rule III; and for a while, after[Pg 33]
the appearance of returning life, carefully aid the first short gasps
until deepened into full breaths. Continue the drying and rubbing,
which should have been unceasingly practiced from the beginning by
assistants, taking care not to interfere with the means employed to
produce breathing. Thus the limbs of the patient should be rubbed,
always in an upward direction toward the body, with firm-grasping
pressure and energy, using the bare hands, dry flannels, or
handkerchiefs, and continuing the friction under the blankets, or over
the dry clothing. The warmth of the body can also be promoted by the
application of hot flannels to the stomach and armpits, bottles or
bladders of hot water, heated bricks, etc., to the limbs and soles of
the feet.
Rule IV. After Treatment. Externally.—As soon as breathing is
established let the patient be stripped of all wet clothing, wrapped
in blankets only, put to bed comfortably warm, but with a free
circulation of fresh air, and left to perfect rest. Internally: Give
whisky or brandy and hot water in doses of a teaspoonful to a
tablespoonful, according to the weight of the patient, or other
stimulant at hand, every ten or fifteen minutes for the first hour,
and as often thereafter as may seem expedient. Later Manifestations:
After reaction is fully established there is great danger of
congestion of the lungs, and if perfect rest is not maintained for at
least forty-eight hours, it sometimes occurs that the patient is
seized with great diffi[Pg 34]culty of breathing, and death is liable to
follow unless immediate relief is afforded. In such cases apply a
large mustard plaster over the breast. If the patient gasps for breath
before the mustard takes effect, assist the breathing by carefully
repeating the artificial respiration.
IF ONE PERSON MUST WORK ALONE.
MODIFICATION OF RULE III
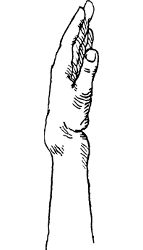
[To be used after Rules I and II in case no assistance is at hand]
To Produce Respiration.—If no assistance is at hand, and one person
must work alone, place the patient on his back with the shoulders
slightly raised on a folded article of clothing; draw forward the
tongue and keep it projecting just beyond the lips; if the lower jaw
be lifted, the teeth may be made to hold the tongue in place; it may
be necessary to retain the tongue by passing a handkerchief under the
chin and tying it over the head.[3]
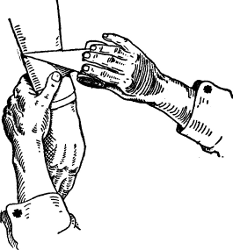
Grasp the arms just below the elbows and draw them steadily upward by
the sides of the patient's head to the ground, the hands nearly
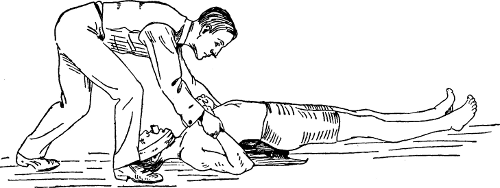
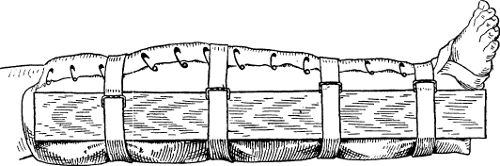
meeting. (See Fig. 4.)
Next lower the arms to the side, and press firmly[Pg 35]
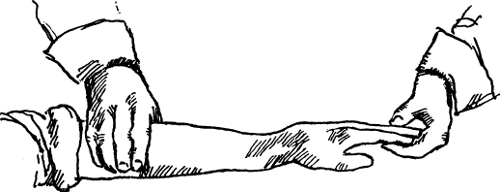
[Pg 36] downward and
inward on the sides and front of the chest over the lower ribs,
drawing arms toward the patient's head. (See Fig. 5.)
Repeat these movements twelve to fifteen times every minute, etc.
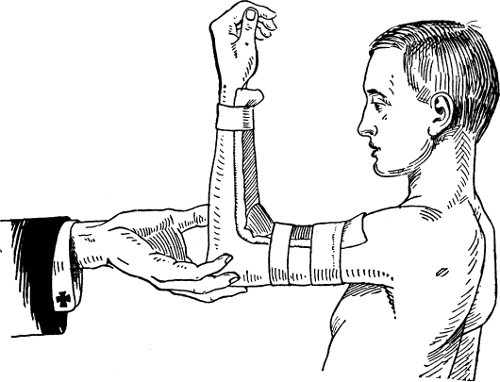
 Fig. 4.
Fig. 4.
ONE PERSON WORKING.
First Position: Note arm movement same as in Fig. 2; also, tongue held
between teeth by handkerchief tied under chin pressing teeth against
wooden plug.
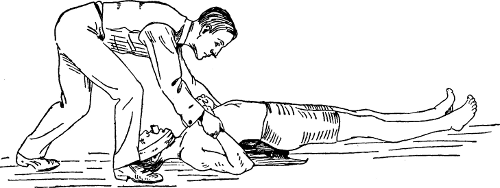 Fig. 5.
Fig. 5.
ONE PERSON WORKING.
Second Position: Note rescuer lowering arms to patient's sides and
pressing downward and inward over lower ribs.
INSTRUCTIONS FOR SAVING DROWNING PERSONS BY SWIMMING TO THEIR RELIEF.
1. When you approach a person drowning in the water, assure him, with
a loud and firm voice, that he is safe.
2. Before jumping in to save him, divest yourself as far and as
quickly as possible of all clothes; tear them off, if necessary; but
if there is not time, loose at all events the foot of your drawers, if
they are tied, as, if you do not do so, they fill with water and drag
you.
3. On swimming to a person in the sea, if he be struggling do not
seize him then, but keep off for a few seconds till he gets quiet, for
it is sheer madness to take hold of a man when he is struggling in the
water, and if you do you run a great risk.
4. Then get close to him and take fast hold of the hair of his head,
turn him as quickly as possible on to his back, give him a sudden
pull, and this will cause him to float, then throw yourself on your
back also and swim for the shore, both hands having hold of his hair,
you on your back, and he also on his, and of[Pg 37] course his back to your
stomach. In this way you will get sooner and safer ashore than by any
other means, and you can easily thus swim with two or three persons;
the writer has even, as an experiment, done it with four, and gone
with them forty or fifty yards in the sea. One great advantage of this
method is that it enables you to keep your head up, and also to hold
the person's head up you are trying to save. It is of primary
importance that you take fast hold of the hair, and throw both the
person and yourself on your backs. After many experiments, it is
usually found preferable to all other methods. You can in this manner
float nearly as long as you please, or until a boat or other help can
be obtained.
5. It is believed there is no such thing as a death grasp; at least,
it is very unusual to witness it. As soon as a drowning man begins to
get feeble and to lose his recollection, he gradually slackens his
hold until he quits it altogether. No apprehension need, therefore, be
felt on that head when attempting to rescue a drowning person.
6. After a person has sunk to the bottom, if the water be smooth, the
exact position where the body lies may be known by the air bubbles,
which will occasionally rise to the surface, allowance being, of
course, made for the motion of the water, if in a tide way or stream,
which will have carried the bubbles out of a perpendicular course in
rising to the surface. Oftentimes a body may be regained from the
bottom, before[Pg 38] too late for recovery, by diving for it in the
direction indicated by these bubbles.
7. On rescuing a person by diving to the bottom, the hair of the head
should be seized by one hand only, and the other used in conjunction
with the feet in raising yourself and the drowning person to the
surface.
8. If in the sea, it may sometimes be a great error to try to get to
land. If there be a strong "outsetting tide" and you are swimming
either by yourself or having hold of a person who cannot swim, then
get on your back and float till help comes. Many a man exhausts
himself by stemming the billows for the shore on a back-going tide,
and sinks in the effort, when, if he had floated, a boat or other aid
might have been obtained.
9. These instructions apply alike to all circumstances, whether as
regards the roughest sea or smooth water.
[Pg 39]
CHAPTER II
Heat Stroke and Electric Shock
How Persons are Overcome by Heat—Treatment of Sunstroke—Peculiar
Cases—Dangers of Electric Shocks—How Death is Caused—Rules and
Precautions.
HEAT EXHAUSTION.
First Aid Rule 1.—Carry patient flat and lay in shade. Loosen
clothes at neck and waist.
Rule 2.—Raise head and give him (a) teaspoonful of essence of ginger
in glass of hot water, or give him (b) half a cup of hot coffee,
clear.
Rule 3.—Put him to bed.
HEAT STROKE.
First Aid Rule 1.—Send for physician.
Rule 2.—Remove quickly to shady place, loosening clothes on the
way.
Rule 3.—Strip naked and put on wire mattress (or canvas cot), if
obtainable.
Rule 4.—Sprinkle with ice water from watering pot, or dash it out of
basin with hand.
Rule 5.—Dip sheet in ice water and tuck it snugly about patient.
Rule 6.—Sprinkle outside of sheet with ice water;[Pg 40] rub body, through
the sheet, with piece of ice. Put piece of ice to nape of neck.
Rule 7.—When temperature falls to 98.5° F. put to bed with ice cap
on head.
SUNSTROKE.—There are two very distinct types of sunstroke: (1) Heat
exhaustion or heat prostration. (2) Heat stroke.
Heat prostration or exhaustion occurs when persons weakened by
overwork, worry, or poor food are exposed to severe heat combined with
great physical exertion. It often attacks soldiers on the march, but
also those not exposed to the direct rays of the sun, as workers in
laundries, in boiler rooms, and in stoke-holes of steamers. The attack
begins more often in the afternoon or evening, in the case of those
exposed to out-of-door heat. Feelings of weakness, dizziness, and
restlessness, accompanied by headache, are among the first symptoms.
The face is very pale, the skin is cool and moist, although the
trouble often starts with sudden arrest of sweating. There is great
prostration, with feeble, rapid pulse, frequent and shallow breathing,
and lowered temperature, ranging often from 95° to 96° F. The patient
usually retains consciousness, but rarely there is complete
insensibility. The pernicious practice of permitting children at
seaside resorts to wade about in cold water while their heads are
bared to the burning sun is peculiarly adapted to favor heat
prostration.
[Pg 41]Heat stroke happens more frequently to persons working hard under the
direct rays of the sun, especially laborers in large cities who are in
the habit of drinking some form of alcohol. It often occurs in
unventilated tenements on stifling nights. Dizziness, violent
headache, seeing spots before the eyes, nausea, and attempts at
vomiting, usher in the attack. Compare it with heat prostration, and
note the marked differences. The patient becomes suddenly and
completely insensible, and falls to the ground, the face is flushed,
the breathing is noisy and difficult, the pulse is strong, and the
thermometer placed in the bowel registers 107°, 108°, or 110° F., or
rarely higher. The muscles are usually relaxed, but sometimes there
are twitchings, or even convulsions. Death often occurs within
twenty-four or thirty-six hours, preceded by failing pulse, deep
unconsciousness, and rapid breathing, often labored or gasping,
alternating with long intermissions. Sometimes delirium and
unconsciousness last for days. Diminution of fever and returning
consciousness herald recovery, but it is a very fatal disorder,
statistics showing a death rate of from thirty to fifty per cent. Even
when the patient lives, bad after effects are common. Peculiar
sensibility to moderate heat is a frequent complaint. Loss of memory,
weakened mental capacity, headache, irritability, fits, other mental
disturbances, and impairment of sight and hearing are among the more
usual sequels, occurring in those who do not subsequently avoid the
direct rays of the sun, as well as an elevated[Pg 42] temperature, and who
indulge in alcoholic stimulants. A high degree of moisture in the air
favors sunstrokes, but it is a curious fact that sunstroke is much
more frequent in certain localities, and in special years than at
other places and times with identical climatic conditions. This has
led observers to suggest a germ origin of the disease, but this is
extremely doubtful.
Treatment.—Treatment for heat exhaustion is given in the "first-aid"
directions. Little need be added to the directions for treatment of
heat stroke. In place of the ice cap suggested in Rule 7, ice in
cloths, or in a sponge bag may be substituted. The friction of the
body, as directed in Rule 6, is absolutely necessary to stimulate the
nervous system and circulation, and to prevent the blood from being
driven into the internal organs by the cold applied externally. The
cold-water treatment is applied until the temperature falls down to
within a few degrees of normal—that is, 98.6° F. Then the patient
should be put into bed, there to remain, with ice to the head, until
fully restored.
It often happens that the fever returns, in which event the whole
process of applying cold water must be repeated. The simplest way of
reducing the fever consists in laying the patient, entirely nude, on a
canvas cot or wire mattress, binding ice to the back of his neck, and
having an attendant stand on a chair near by and pour ice water upon
the patient from a garden watering pot.
[Pg 43]While the patient is insensible no attempt should be made to give
anything by the mouth; but half a pint of milk and two raw eggs with a
pinch of salt may be injected into the rectum every eight hours, after
washing it out with cold water on each occasion. Two tablespoonfuls of
whisky may be added to the injection, if the pulse is weak. If the
urine is not passed spontaneously, it will be necessary to draw it
once in eight hours with a soft rubber catheter which has been boiled
ten minutes and lubricated with glycerin or clean vaseline.
ELECTRIC SHOCK OR LIGHTNING STROKE.
First Aid Rule 1.—Protect yourself from being shocked by the victim.
Grasp victim only by coat tails or dry clothes. Put rubber boots on
your hands, or work through silk petticoat; or throw loop of rubber
suspenders or of dry rope around him to pull him off wire, or pry him
along with dry stick.
Rule 2.—Do not lift, but drag victim away from wire toward the
ground. When free from wire, hold him head downward for two minutes.
Rule 3.—Assist heart to regain its strength. Apply mustard plaster
(mustard and water) to chest over heart; wrap in blanket wrung out of
very hot water; give hypodermic of whisky, thirty minims.
Rule 4.—Induce artificial respiration. Open his mouth and grasp
tongue, pull it forward just beyond lips, and hold it there. Let
another assistant[Pg 44] grasp the arms just below the elbows and draw them
steadily upward by the sides of the patient's head to the ground, the
hands nearly meeting (which enlarges the capacity of the chest and
induces inspiration, Fig. 2). While this is being done, let a third
assistant take position astride the patient's hips with his elbows
resting on his own knees, his hands extended, ready for action. Next,
let the assistant standing at the head turn down the patient's arms to
the sides of the body, the assistant holding the tongue changing
hands, if necessary, to let the arms pass. Just before the patient's
hands reach the ground, the man astride the body will grasp the body
with his hands, the ball of the thumb resting on either side of the
pit of the stomach, the fingers falling into the grooves between the
short ribs. Now, using his knees as a pivot, he will at the moment the
patient's hands touch the ground throw (not too suddenly) all his
weight forward on his hands, and at the same time squeeze the waist
between them, as if he wished to force something in the chest upward
out of the mouth; he will deepen the pressure while he slowly counts
one, two, three, four (about five seconds), then suddenly lets go with
a final push, which will send him back to his first position. This
completes expiration. (A child or delicate person must be more gently
handled.)
At the instant of letting go, the man at the patient's head will
again draw the arms steadily upward to the sides of the patient's
head, as before (the assistant[Pg 45] holding the tongue again changing
hands to let the arms pass, if necessary), holding them there while he
slowly counts one, two, three, four (about five seconds).
Repeat these movements deliberately and perseveringly twelve to
fifteen times in every minute—thus imitating the natural motions of
breathing. Continue the artificial respiration from one to four hours,
or until the patient breathes; and for a while, after the appearance
of returning life, carefully aid the first short gasps until deepened
into full breaths.
Keep body warm with hot-water bottles, hot bricks to limbs and feet,
and blankets over exposed lower part of body.
Rule 5.—Treat burn, if any. If skin is not broken, cover burn with
cloths wet with Carron oil (equal parts of limewater and linseed or
olive oil). If skin is broken, or raw surface is exposed, spread over
it paste of equal parts of boric acid and vaseline, and bandage over
all.
Conditions, Etc.—A shock produced by contact with an electric current
is not of rare occurrence. Lightning stroke is very uncommon;
statistics show that in the United States each year there is one death
from this cause to each million of inhabitants. There are several
conditions which must be borne in mind when considering the accidental
effect of an electric current. The pressure and strength of the
current[Pg 46] (voltage and amperage) are often not nearly so important in
regard to the effects on the body, as the area, duration, and location
of the points of contact with the current, and the resistance offered
by clothing and dry skin to the penetration of the electricity.
When the heart lies in the course of the circuit, the danger is
greatest. A dog can be killed by a current of ten volts pressure when
contacts are made to the head and hind legs, because the current then
flows through the heart, while a current of eighty volts is required
to kill a dog, under the same conditions, if contacts are made to head
and fore leg. In a general way alternating currents of low frequency
are the most injurious to the body, and any current pressure higher
than two hundred volts is dangerous to life. On the other hand, a
current of ninety-five volts has proved fatal to a human being. In
this case the circumstances were particularly unfavorable to the
victim, as he was standing on an iron tank in boots wet with an
alkaline solution, and probably studded on the soles with nails, when
he came in accidental contact with an industrial current. Moreover, he
was an habitual drunkard. In an instance of the contrary sort, a man
received a current of 1,700 volts (periodicity about 130) for fifty
seconds, in one of the early attempts at electro-execution, without
being killed. The personal equation evidently enters into the matter.
A strong physique here, as in other cases, is most favorable in
resisting the effects of electric shock.
[Pg 47]High-pressure alternating currents (1,300 to 2,000 volts) are employed
in electro-executions, and the contacts are carefully made, so that
the current will enter the brain and pass through the heart to the
leg. The two most vital parts are thus affected. In industrial
accidents such nice adjustments are fortunately almost impossible, and
shocks received from high-pressure currents, even of 25,000 volts,
have not proved fatal because both the voltage and amperage have been
greatly lessened through poor contacts and great resistance of
clothing and dry skin, and also because the heart is not usually
included in the circuit.
Death is induced in one of three ways: 1. Currents of enormous voltage
and amperage, as occur in lightning, actually destroy, burst and burn
the tissues through which the stroke passes. 2. Usually death follows
accidents from industrial currents, owing to contraction of the heart,
the effect being the same as observed on other muscles. The heart
instantly ceases beating, and either remains absolutely quiet, or
there is a fine quivering of some of its fibers, as seen on opening
the chest in experiments upon animals. 3. A fatal issue may result
from the passage of the current through the head, so affecting the
nerve centers that govern respiration that the breathing ceases.
Symptoms.—These are generally muscular contractions, faintness, and
unconsciousness (sometimes convulsions, if the current passes through
the head), with failure of pulse and of breathing. For instance, a
man[Pg 48] who was removing a brush from a trolley car touched, with the
other hand, a live rail. His muscles immediately contracted throwing
him back, and disconnecting him from contact with the current (500
volts). He then fainted and became unconscious for a short time. The
pulse was rapid and feeble, and the breathing also at first, but it
later became slower than usual. On regaining sensibility the patient
vomited and got on his feet, although feeling very weak for two hours.
Unconsciousness commonly lasts only a few moments in nonfatal cases,
but may continue for hours, its continuance being rather a favorable
sign of ultimate recovery, if the heart and lungs are acting
sufficiently. Bad after effects are rare. It is not uncommon for the
patient to declare that the accident had improved his general
feelings. Occasionally there is temporary loss of muscular power, and
a case has been reported of nervous symptoms following electric shock
similar to those observed after any accidental violence. Burns of
varying degrees of intensity occur at the point of entrance of the
current, from slight blisters to complete destruction of all the
tissues.
Treatment.—The treatment is completely outlined in the "first-aid"
directions. Should contact be unbroken, an order to shut off the
electric current should at once be telephoned to the station.
Protection of the rescuer with thick rubber gloves is of course the
ideal safeguard.
In fatal cases the heart is instantaneously arrested,[Pg 49] and nothing can
be done to start it into action. If the current passes through the
brain, by contact with the head or neck, then failure of breathing is
more apt to be the cause of death. Theoretically, it is in the latter
event only that treatment, i. e., artificial respiration, will be of
avail.
But as in any individual case the exact condition is always a matter
of doubt, artificial respiration is the most valuable remedial
measure we possess; it should always be practiced for hours in
doubtful cases. Two tablespoonfuls of brandy or whisky in a cup of
warm water may be injected into the bowel, if a hypodermic syringe is
not available and the patient needs decided stimulation.
[Pg 50]
CHAPTER III
Wounds, Sprains and Bruises
Treatment of Wounds—Rules for Checking Hemorrhage—Lockjaw—Bandages
for Sprains—Synovitis—Bunions and Felons—Foreign Bodies in the Eye,
Ear and Nose.
WOUNDS.—A wound is a condition produced by a forcible cutting,
contusing, or tearing of the tissues of the body, and includes, in its
larger sense, bruises, sprains, dislocations, and breaks or fractures
of bones. As ordinarily used, a wound is an injury produced by
forcible separation of the skin or mucous membrane, with more or less
injury to the underlying parts.
The main object during the care of wounds should be to avoid
contamination with anything which is not surgically clean, from the
beginning to the end of the dressing; otherwise, every other step in
the whole process is rendered useless.
Three essentials in the treatment of wounds are:
1. The arrest of bleeding. 2. Absolute cleanliness. 3. Rest of the
injured part. Dangerous bleeding demands immediate relief.
Bleeding is of three kinds: 1. From a large artery. 2. From a vein. 3.
General oozing.
[Pg 51]BLEEDING FROM LARGE ARTERY IN SPURTS OF BRIGHT BLOOD.
First Aid Rule 1.—Speed increases safety. Put patient down flat.
Make pressure with hands between the wound and the heart till surgeon
arrives, assistants taking turns.
Rule 2.—If arm or leg, tie rubber tubing or rubber suspenders tight
about limb between wound and heart, or tie strap or rope over
handkerchief or folded shirt wrapped about limb. If arm, put baseball
in arm pit, and press arm against this. Or, for arm or leg, tie folded
cloth in loose noose around limb, put cane or umbrella through noose
and twist up the slack very tight, so as to compress the main artery
with knot.
Rule 3.—Keep limb and patient warm with hot-water bottles till
surgeon arrives.
This treatment is of course only a temporary expedient, as it is
essential for a surgeon to tie the bleeding vessel itself; therefore a
medical man should be summoned with all dispatch.
BLEEDING FROM VEIN; STEADY FLOW OF DARK BLOOD.
First Aid Rule 1.—Make firm pressure with pad of cloth directly over
wound, also with hands between wound and extremity, that is, on side
of cut away from the heart.
[Pg 52]Rule 2.—Tie tight bandage about limb at this point, with rubber
tubing or suspenders.
Rule 3.—Keep limb and patient warm with hot-water bottles till
surgeon arrives.
In the cases of bleeding from a vein, the flow of blood is continuous,
and is of a dark, red hue, and does not spurt in jets, as from an
artery. This kind of bleeding is not usually difficult to stop, and it
is not necessary that the vein itself be tied—unless very
large—provided that the wound be snugly bandaged after it is dressed.
After the first half hour, release the limb and see if the bleeding
has stopped. If so, and the circulation is being interfered with,
owing to the tightness of the bandage, reapply the bandage more
loosely.
In the case of an injured artery of any considerable size, the amount
of pressure required to stop the bleeding will arrest all circulation
of blood in the limb, so that great damage, as well as pain, will
ensue if it be continued more than an hour or two, and during this
time the limb should be kept warm by thick covering and hot-water
bags, if they can be obtained.
Bleeding from a deep puncture may be stopped by plugging the cavity
with strips of muslin which have been boiled, or with absorbent
cotton, similarly treated, keeping the plug in place by snug
bandaging.
[Pg 53]BLEEDING FROM PUNCTURED WOUND.
First Aid Rule 1.—Extract pin, tack, nail, splinter, thorn, or
bullet, IF YOU CAN SEE BULLET; do not probe.
Rule 2.—Pour warm water on wound and squeeze tissue to encourage
bleeding. Send for small hard-rubber syringe.
Rule 3.—If deep, plug it with absorbent cotton, and put tight
bandage over plug. If shallow, cover with absorbent cotton wet with
boric-acid solution (one dram to one-half pint of water), or
carbolic-acid solution (one teaspoonful to the pint of hot water).
Rule 4.—When syringe comes, remove dressing, and clean wound by
forcibly syringing carbolic solution directly into wound. Replace
dressing.
A small punctured wound should be squeezed in warm water to encourage
bleeding and, if pain and swelling ensue, absorbent cotton soaked in a
boric-acid solution (containing as much boric acid as the water will
dissolve) or in carbolic-acid solution (one teaspoonful of pure acid
to the pint of warm water) should be applied over the wound and
covered with oil silk or rubber or enamel cloth for a few days, or
until the soreness has subsided. The dressing should be wet with the
solution as often as it becomes dry. Punctures by nails, especially if
deep, should be washed out with a syringe, using one of the solutions
just mentioned. A medicine dropper, minus the rubber part, attached to
a fountain syringe, makes a good nozzle[Pg 54] for this purpose. A moist
dressing, like the one described, should then be applied, and the limb
kept in perfect rest for a few days.
When a surgeon's services are available, however, self-treatment is
attended with too much danger, as a thorough opening up of such wounds
with proper cleansing and drainage will afford a better prospect of
early recovery, and avert the risk of serious inflammation and
lockjaw, which sometimes follow punctured wounds of the hands and
feet. Foreign bodies, as splinters, may be removed with tweezers or a
needle, being careful not to break the splinter in the attempt. If a
part remains in the flesh, or if the foreign body is a needle that
cannot be found or removed at once, the continuous application of a
hot flaxseed or other poultice will lead to the formation of "matter,"
with which the splinter or needle will often escape after a few days.
Splinters finding their way under the nail may be removed by scraping
the nail very thin over the splinter and splitting it with a sharp
knife down to the point where the end of the splinter can be grasped.
BLEEDING IN FORM OF OOZING.
First Aid Rule 1.—Apply water as hot as hand can bear.
Rule 2.—Elevate the part, and drench with carbolic solution (one
teaspoonful of carbolic acid to one pint of hot water).
[Pg 55]Rule 3.—Bandage snugly while wet.
Rule 4.—Keep patient warm with hot-water bottles.
GENERAL OOZING happens in the case of small wounds or from abraded
surfaces, and is caused by the breaking of numerous minute vessels
which are not large enough to require the treatment recommended for
large arteries or veins. It is rarely dangerous, and usually stops
spontaneously. When the loss of blood has been considerable, so that
the patient is pale, faint, and generally relaxed, with cold skin, and
perhaps nausea and vomiting, he should be stripped of all clothing and
immediately wrapped in a blanket wrung out of hot water, and then
covered with dry blankets. Heat should also be applied to the feet by
means of hot-water bags or bottles, with great care not to burn a
semiconscious patient's skin. The head should be kept low, and two
tablespoonfuls of brandy, whisky, or other alcoholic liquor should be
given in a half cup of hot water by the mouth, if the patient can
swallow. If much blood has been lost a quart of water, as hot as the
hand can readily bear, and containing a teaspoonful of common salt,
should be injected by means of a fountain syringe into the rectum.
Somewhat the condition just described as due to loss of blood may be
caused simply by shock to the nervous system following any severe
accident, and not attended by bleeding. The treatment of shock is,
however, practically the same as that for hemorrhage, and[Pg 56] improvement
in either case is shown by return of color to the face and strength in
the pulse. Bleeding is apt to be much less in badly torn than in
incised wounds, even if large vessels are severed, as when the legs
are cut off in railroad accidents, for the lacerated ends of the
vessels become entangled with blood and favor clotting.
LOCKJAW.—In the lesser injuries, where bleeding is not an important
feature, and in all wounds as well, after bleeding has been stopped,
the main object in treatment consists in cleansing wounds of the germs
which cause "matter" or pus, general blood poisoning, and lockjaw. The
germs of the latter live in the earth, and even the smallest wounds
which heal perfectly may later give rise to lockjaw if dirt has not
been entirely removed from the wound at the time of accident. Injuries
to the hands caused by pistols, firecrackers, and kindred explosives,
seem especially prone to produce lockjaw, and fatalities from this
disorder are deplorably numerous after Fourth-of-July celebrations in
the United States.
The wounds producing lockjaw usually occur in children who explode
blank cartridges in the palm of the hand. In this way the germs of the
disease are forced in with parts of the dirty skin and more or less of
the wad from the shell. Since lockjaw is so frequent after these
accidents, and so fatal, it is impossible to exert too much care in
treatment. The wound should at once be thoroughly opened with a knife
to the very[Pg 57] bottom, under ether, by a surgeon, and not only every
particle of foreign matter removed, but all the surrounding tissue
should be cut out or cauterized. In addition, it is wise to use an
injection under the skin of tetanus-antitoxin, to prevent the disease.
Proper restriction of the sale of explosives alone will put a stop to
this barbarous mode of exhibiting patriotism.
Treatment.—It is not essential to use chemical agents or antiseptics
to rid wounds of germs and so secure uninterrupted healing. The person
who is to dress the wound should prepare to do so at the earliest
possible moment after giving first aid. He should proceed promptly to
boil some pieces of absorbent cotton, as large as an egg, together
with a nail brush in water. Some strips of clean cotton cloth may be
used in the absence of absorbent cotton. The boiling should be
conducted for five minutes, when the basin or other utensil in which
the brush and cotton are boiled should be taken off the fire and set
aside to cool. Then the attendant should scrub his own hands for five
minutes in hot water with soap and brush.
He next takes the brush, which has been boiled, out of the water and
cleans the patient's skin for a considerable distance about the wound.
When this is done, and the water and cotton which have been boiled are
sufficiently cool, the wound should be bathed with the cotton and
boiled water until all foreign matter has been removed from the wound;
not only dirt which can be seen, but germs which cannot be seen. Some[Pg 58]
of the boiled cotton cloth or absorbent cotton, wet as it is, should
be placed over the wound and the whole covered by a bandage. Large
gaping wounds are of course more properly closed by stitches, but very
deep wounds should be left partly open, so that the discharge may
drain away freely. Small, deep, punctured wounds are not to be closed
at all, but should be sedulously kept open by pushing in strips of
boiled cotton cloth, in order to secure drainage.
If the attendant has the requisite confidence, there is no reason why
he should not attempt stitching a wound, providing the patient is
willing, and a surgeon cannot be obtained within twenty-four hours. In
this case a rather stout, common sewing needle or needles are threaded
with black or white thread, preferably of silk, and, together with a
pair of scissors and a clean towel, are boiled in the same utensil
with the cotton and the nail brush. After the operator has scrubbed
his hands and cleansed the wound, he places the boiled towel about the
wound so that the thread will fall on it during his manipulations and
not on the skin. The needle should be thrust into and through the
skin, but no lower than this, and should enter and leave the skin
about a quarter of an inch from either edge of the wound. The stitches
are placed about one-half inch apart, and are drawn together and tied
tightly enough to join the two edges of the wound. The ends of the
thread should be cut about one-half inch from the knot, being careful
while using the needle[Pg 59] and scissors not to lay them down on anything
except the boiled towel. The wound is then covered with cotton, which
has been boiled as described above, bandaged and left undisturbed for
a week, if causing no pain. At the end of this time the stitches are
taken out after the attendant has washed his hands carefully, and
boiled his scissors as before.
Court plaster or plaster of any kind is a bad covering or dressing for
wounds, as it may be itself contaminated with germs. It effectually
keeps in any with which the wound is already infected, and prevents
proper drainage.
It is impossible in a work of this kind to describe the details of the
after treatment of wounds, as this can only be properly undertaken by
a surgeon, owing to the varying conditions which may arise. In general
it may be stated that the same cleanliness and care should be followed
during the whole course of healing as has been outlined for the first
attempt at treatment.
If the wound is small, and there is no discharge from it, it may be
painted with collodion or covered with boric-acid ointment (sixty
grains of boric acid to the ounce of vaseline) after the first day. If
large, it should be covered with cotton gauze or cloth which have been
boiled or specially prepared for surgical purposes. If pus ("matter")
forms, the wound must be cleansed daily of discharge (more than once
if it is copious) with boiled water, or best with hydrogen[Pg 60] dioxide
solution followed by a washing with a solution of carbolic acid (one
teaspoonful to the pint of hot water), or with a solution of mercury
bichloride, dissolving one of the larger bichloride tablets, sold for
surgical uses, in a quart of water.
It is a surgical maxim never to be neglected that wounds should not be
allowed to close at the top before healing is completed at the bottom.
As to close at the surface is the usual tendency in wounds that heal
slowly and discharge pus, it is necessary at times to enlarge the
external opening by cutting or stretching with the blades of a pair of
scissors, or, and this is much more rational and comfortable for the
patient, by daily packing the outlet of the wound with gauze to keep
it open.
BLEEDING FROM SCALP.
First Aid Rule 1.—Cut hair off about wound, and clean thoroughly
with carbolic-acid solution (one teaspoonful to pint of hot water).
Rule 2.—Put pad of gauze or muslin directly over wet wound, and make
pressure firmly with bandage.
In case of wounds of the scalp, or other hairy parts, the hair should
be cut, or better shaved, over an area very much larger than the
wounded surface, after which the cleansing should be done. To stop
bleeding of the scalp, water is applied as hot as can be borne, and
then a wad of boiled cotton should be placed in the[Pg 61] wound and
bandaged down tightly into it for a time. Closing the wound with
stitches will stop the bleeding much more effectively, however, and is
not very painful if done immediately after the accident. The stitches
should be tied loosely, and not introduced nearer to each other than
half an inch, to allow drainage of discharge from the wound.
General Remarks.—All wounds should be kept at rest after they are
dressed. This is accomplished in the case of the lower limbs by
keeping the patient in bed with the leg raised on a pillow.
The same kind of treatment applies in severe injuries of the hands. In
less serious cases a sling may be employed, and the patient may walk
about. When the injury is near a joint, as of the fingers, knee,
wrist, or elbow, a splint made of thin board or tin (and covered with
cotton wadding and bandaged) should be applied by means of surgeon's
adhesive plaster and bandage after the wound has been dressed. In
injuries of the hand the splint should be applied to the palm side,
and reach from the finger tips to above the wrist. Use a splint also.
NOSEBLEED.
First Aid Rule 1.—Seat patient erect and apply ice to nape of neck.
Rule 2.—Put roll of brown paper under upper lip, and press lip
firmly against it. Press facial artery against lower jaw of bleeding
side, till bleeding stops.[Pg 62] This artery crosses lower edge of jawbone
one inch in front of angle of jaw.
Rule 3.—Plug nostril with strip of thin cotton or muslin cloth.
Rule 4.—Do not wash away clots; encourage clotting to close
nostril.
BLEEDING FROM LUNGS; BRIGHT BLOOD COUGHED UP.
BLEEDING FROM STOMACH; DARK BLOOD VOMITED.
First Aid Rule for both. Let patient lie flat and swallow small
pieces of ice, and also take one-quarter teaspoonful of table salt in
half a glass of cold water.
BRUISE.
First Aid Rule 1.—Bandage from tips of fingers, or from toes, making
same pressure with bandage all the way up as you do over the injury.
Rule 2.—Apply heat through the bandage, over the injury, with
hot-water bottles.
Cause, Etc.—A bruise is a hidden wound; the skin is not broken. It is
an injury caused by a blunt body so that, while the tougher skin
remains intact, the parts beneath are torn and crushed to a greater or
lesser extent. The smaller blood vessels are torn and blood escapes
under the skin, giving the "black and blue" appearance so common in
bruises of any severity.[Pg 63] Sometimes, indeed, large collections of
blood form beneath the skin, causing a considerable swelling.
Use of the bruised part is temporarily limited. Pain, faintness, and
nausea follow severe bruises, and, in case of bad bruises of the
belly, death may even ensue from damage to the viscera or to the
nerves. Dangerous bleeding from large blood vessels sometimes takes
place internally, and collections of blood may later break down into
abscesses. Furthermore, the bruise may be so great that the injury to
muscle and nerve may lead to permanent loss of use of the part. For
these reasons a surgeon's advice should always be sought in cases of
bad bruises. Pain is present in bruises, owing to the tearing and
stretching of the smaller nerve fibers, and to pressure on the nerves
caused by swelling. The swelling is produced by escape of blood and
fluid from the torn blood vessels.
Treatment.—Even slight and moderate bruises should be treated by rest
of the injured part. A splint insures the rest of a limb (see
treatment of Fractures, p. 80). One of the best modes of treatment is
the snug application of a flannel bandage which secures a certain
amount of rest of the part to which it is applied, and aids in
preventing further swelling. Where bandaging is not feasible, as in
certain parts of the body, or before bandaging in any kind of a
bruise, the use of a cold compress is advisable. One layer of thin
cotton or linen cloth should be wet in ice water, and should be put on
the bruised part and continually[Pg 64] changed for newly moistened pieces
as soon as the first grows warm. Alcohol and water, of each equal
parts, may be used in the same manner to advantage.
When cold is unavailable or unpleasant to the patient, several layers
of cotton cloth may be wrung out in very hot water and applied to the
part with frequent renewal. The value attributed to witch-hazel and
arnica is mainly due to the alcohol contained in their preparations.
Cataplasma Kaolini (U. S. P.) is an excellent remedy for simple
bruises when spread thickly on the part and covered with a bandage. An
ointment containing twenty-five per cent of ichthyol is also a useful
application. Following severe bruises, the damaged parts should be
kept warm by the use of hot-water bags, or by covering a limb with
cotton wool and bandage, until such time as surgical advice may be
obtained.
When the pain and swelling of bruises begin to subside, treatment
should be pursued by rubbing with liniment of ammonia or chloroform,
or vaseline if these are not obtainable. Moderate exercise of the part
is desirable.
ABRASIONS.—When the surface skin is scraped off, as often happens to
the shin, knee, or head, an ointment containing sixty grains of boric
acid to the ounce of vaseline makes a good application, and this may
be covered with a bandage. The same ointment is useful to apply to
small wounds and cuts after the first bandage is removed.
[Pg 65]SPRAIN; NO DISPLACEMENT OF BONES.
First Aid Rule 1.—Immerse in water, hot as hand can bear, for half
an hour.
Rule 2.—Dry and strap with adhesive plaster, if you know how. If
not, bandage snugly, beginning with tips of fingers or with toes, and
make same pressure all the way up that you do over injury.
Rule 3.—Rest. If ankle or knee is hurt, patient must go to bed.
Conditions, Etc.—A sprain is an injury caused by a sudden wrench or
twist of a joint, producing a momentary displacement of the ends of
the bones to such a degree that they are forced against the membrane
and ligaments surrounding the joint, tearing one or both to a greater
or less extent. The wrist and ankle are the joints more commonly
sprained, and this injury is more likely to occur in persons with
flabby muscles and relaxed ligaments, as in the so-called
"weak-ankled." The damage to the parts holding the joint in place may
be of any degree, from the tearing of a few fibers of the membrane
enwrapping the joint to its complete rupture, together with that of
the ligaments, so that the bones are no longer in place, the joint
loses its natural shape and appearance, and we have a condition known
as dislocation. In a sprain then, the twist of the joint produces only
a temporary displacement of the bones forming the joint, sufficient to
damage the soft structures around it, but not suffi[Pg 66]cient to cause
lasting displacement of the bones or dislocation.
It will be seen that whether a sprain or dislocation results, depends
upon the amount of injury sustained. Since it often happens that the
bone entering into the joint is broken, it follows that whenever what
appears to be a severe sprain occurs, with inability to move the joint
and great swelling, it is important to secure surgical aid promptly.
Since the discovery of the X-ray many injuries of the smaller bones of
the wrist and ankle joint, formerly diagnosed as sprains by the most
skillful surgeons, have, by its use, been discovered to be breaks of
the bones which were impossible of detection by the older methods of
examination.
Symptoms.—The symptoms of sprain are sudden, severe pain, often
accompanied by faintness and nausea, swelling, tenderness, and heat of
the injured parts. The sprained joint can be only moved with pain and
difficulty. The swelling is due not so much to leaking of blood from
broken blood vessels as to filling up of the joint with fluid caused
by the inflammation, although in a few days after a severe sprain the
skin a little distance below the injury becomes "black and blue" from
escape of blood caused by the injury.
Treatment.—Since the treatment of severe sprains means first the
discrimination between dislocation, a break of bone, and a rupture of
muscle, ligament, or tendon, it follows that the methods herein
described for treatment should only be employed in slight
unmis[Pg 67]takable sprains, or until a surgeon can be secured, or when one
is unavailable. Nothing is better than immediate immersion of the
sprained joint in as hot water as the hand can bear for half an hour.
Following this, an elastic bandage of flannel cut on the bias about
three and one-half inches wide should be snugly applied to the limb,
beginning at the finger tips or at the toes and carrying the bandage
some distance above the injured joint.
In bandaging a part there is always danger of applying the bandage too
tightly, especially if the parts swell under the bandage. If this
happens, there is increase of pain which may be followed by numbness
of the limb and, what is still more significant, coldness and blueness
of the extremities below the bandage, particularly of the fingers and
toes. In such cases the bandage must be removed and reapplied with
less force. If the ankle or knee be sprained the patient must go to
bed for at least twenty-four hours, and give the limb a complete rest.
When the wrist or shoulder is sprained the arm should be confined in a
sling. In the more serious cases the injured joint should be fixed in
a splint before bandaging. An injured elbow joint is held at a right
angle by a pasteboard splint, a bandage, and a sling, while the knee
and wrist are treated with the limb in a straight line, as far as
possible.
In the case of the knee, the splint is applied to the back of the leg;
in sprained wrist, to the palm of the[Pg 68] hand and same side of the
forearm. Sheet wadding, which may be bought at any drygoods store, is
torn into strips about two inches wide and sewed together forming a
bandage ten or fifteen feet long, and this is first wound about the
sprained joint. Then pieces of millboard or heavy pasteboard are
soaked in water and applied while wet in long strips about three
inches wide over the wadding, and the whole is covered with bandage.
In the case of the knee it is better to use a strip of wood for the
splint, reaching from the lower part of the calf to four inches above
the knee. It should be from a quarter to half an inch thick, a little
narrower than the leg, and be padded thickly with sheet wadding. It is
held in place by strips of surgeon's adhesive plaster, about two
inches wide, passed around the whole circumference of the limb above
and below the knee joint, and covered with bandage.
In ordinary sprains of the ankle, uncomplicated by broken bone or
ligament, it is possible for the patient, after resting in bed for a
day, to go about on crutches, without bearing any weight on the foot
until the third day after the accident. The treatment in the meanwhile
consists in immersing the sprained ankle alternately, first in hot
water for five minutes and then in cold water for five minutes,
followed by rubbing of the parts about the injured joint with
chloroform liniment for fifteen minutes, but not at the beginning
touching the joint itself. The rubbing should be done by an assistant
very gently the first day, with gradual[Pg 69] increase in vigor as the days
pass, not only kneading the ankle but moving the joint.
This treatment should be pursued once daily, and followed by bandaging
with a flannel bandage cut on the bias three and a half inches wide.
With this method it is possible for the patient to regain the moderate
use of the ankle in about two or three weeks.
The same general line of treatment applies to the other joints;
partial rest and daily bathing in hot and cold water, rubbing and
movements of the joint by an assistant. Since sprains vary in severity
it follows that some may need only the first day's preliminary
treatment prescribed to effect a cure, while others may require
fixation by a surgeon in a plaster-of-Paris splint for some time, with
additional treatment which only his special knowledge can supply.
This picture shows an excellent method of fixing a
sprained joint, used by Prof. Virgil P. Gibney, M.D., Surgeon-in-Chief
of the N. Y. Hospital for Ruptured and Crippled. It consists of
strapping the joint by means of long, narrow strips of adhesive
plaster incasing it immovably in the normal position. This procedure
may be followed by anyone who has seen a surgeon practice it.
SYNOVITIS—Severe Injury.—Generally of ankle or knee from fall, or
shoulder from blow.
First Aid Rule 1.—Provide large pitcher of hot water and large
pitcher of cold water and basin. Hold[Pg 70] joint over basin; pour hot
water slowly over joint. Return this water to pitcher. Pour cold water
over joint. Return water to pitcher. Repeat with hot water again, and
follow with cold. Continue this alternation for half an hour.
Rule 2.—Put to bed, with hot-water bottles about joint, and wedge
immovably with pillows.
Rule 3.—When tenderness and heat subside, strap with adhesive
plaster in overlapping strips.
Conditions, Etc.—This condition, which may affect almost any freely
movable joints, as the knee, elbow, ankle, and hip, is commonly caused
by a wrench, blow, or fall. Occasionally it comes on without any
apparent cause, in which case there is swelling and but slight pain or
inflammation about the joint. We shall speak of synovitis of the knee
("water on the knee"), as that is the most common form, but these
remarks will apply almost as well to the other joints. In severe cases
there are considerable pain, redness and heat, and great swelling
about the knee. The swelling is seen especially below the kneepan, on
each side of the front of the joint, and also often above the kneepan.
Frequently the only signs of trouble are swelling with slight pain,
unless the limb is moved.
Treatment.—If the knee is not red, hot, or tender to the touch, it
will not be necessary for the patient to remain in bed, but when these
symptoms are present a splint of some sort must be applied so that the
leg[Pg 71] is kept nearly straight, and the patient must keep to his bed
until the heat, redness, and tenderness have subsided. In the meantime
either an ice bag, hot poultice, cloths wrung out in hot water, or a
hot-water bag should be kept constantly upon the knee.
A convenient splint consists of heavy pasteboard wet and covered with
sheet wadding (or cotton batting) shaped and affixed to the back of
the leg, from six inches below to four inches above the joint, by
strips of adhesive plaster, as shown in the illustration, and then by
bandage, leaving the knee uncovered for applications. A wooden splint
well padded may be used instead.
In mild cases without much inflammation, and in others after the
tenderness and heat have abated, the patient may go about if the knee
is treated as follows: a pad of sheet wadding or cotton batting about
two inches thick and five inches long and as wide as the limb is
placed in the hollow behind the knee, and then the whole leg is
encircled with sheet wadding from six inches below to four inches
above the knee, covering the joint as well as the pad. Beginning now
five inches below the joint, strips of surgeon's adhesive plaster, an
inch wide and long enough to more than encircle the limb, are affixed
about the leg firmly like garters so as to make considerable pressure.
Each strip or garter overlaps the one below about one-third of an
inch, and the whole limb is thus incased in plas[Pg 72]ter from five inches
below the knee to a point about four inches above the joint.
An ordinary cotton bandage is then applied from below over the entire
plaster bandage. When this arrangement loosens, the plaster should be
taken off and new reapplied, or a few strips may be wound about the
old plaster to reënforce it. The patient may walk about with this
appliance without bending the knee.
When the swelling has nearly departed, the plaster may be removed and
the knee rubbed twice daily about the joint and the joint itself moved
to and fro gently by an attendant, and then bandaged with a flannel
bandage. Painting the knee with tincture of iodine in spots as large
as a silver dollar is also of service at this time. The knee should
not be bent in walking until it can be moved by another person without
producing discomfort.
Such treatment may be applied to the other joints in a general way.
The elbow must be fixed by a splint as recommended for dislocation of
the joint (p. 128). The ankle is treated as advised for sprain of that
joint (p. 68). When a physician can be obtained no layman is justified
in attempting to treat a case of water on the knee or similar
affection of other joints.
BUNION AND HOUSEMAID'S KNEE.—Bunion is a swelling of the bursa, or
cushion, at the first joint of the great toe where it joins the foot.
It may not give much trouble, or it may be hot, red, tender, and very
painful. It is caused by pressure of a tight[Pg 73] boot which also forces
the great toe toward the little toe, and thus makes the great toe
joint more prominent and so the more readily injured.
A somewhat similar swelling, often as large as an egg, is sometimes
seen over the kneepan, more often in those who work upon their knees,
hence the name housemaid's knee. The swelling may come on suddenly and
be hot, tender, and painful, or it may be slow in appearing and give
little pain.
Treatment.—The treatment for the painful variety of bunion and
housemaid's knee is much the same: absolute rest with the foot kept
raised, and application of cloths kept constantly wet with ice or cold
water; or a thick covering of Cataplasma Kaolini (U. S. P.) may be
applied until the inflammation has subsided. If the trouble is
chronic, or the acute inflammation does not soon abate under the
treatment advised, the case is one for the surgeon, and sometimes
requires the knife for abscess formation. In the milder cases of
bunion, wearing proper shoes whose inner border forms almost a
straight line from heel to toe, so that the great toe is not pushed
over toward the little toe, and painting the bunion every few days
with tincture of iodine, until the skin begins to become sore, will
often be sufficient to secure recovery.
RUN-AROUND; WHITLOW OR FELON.—"Run-around" consists in an
inflammation of the soft parts about the finger nail. It is more
common in the weak, but may occur in anyone, owing to the entrance[Pg 74] of
pus germs through a slight prick or abrasion which may pass unnoticed.
The condition begins with redness, heat, tenderness, swelling, and
pain of the flesh at the root of the nail, which extends all about the
nail and may be slight and soon subside, or there may be great pain
and increased swelling, with the formation of "matter" (pus), and
result in the loss of the nail, particularly in the weak.
Whitlow or felon is a much more serious trouble. It begins generally
as a painful swelling of one of the last joints of the fingers on the
palm side. Among the causes are a blow, scratch, or puncture. Often
there is no apparent cause, but in some manner the germs of
inflammation gain entrance. The end of the finger becomes hot and
tense, and throbs with sometimes almost unbearable pain. If the
inflammation is chiefly of the surface there may be much redness, but
if mainly of the deeper parts the skin may be but little reddened or
the surface may be actually pale. There is usually some fever, and the
pain is made worse by permitting the hand to hang down. If the felon
is on the little finger or thumb the inflammation is likely to extend
down into the palm of the hand, and from thence into the arm along the
course of the tendons or sinews of the muscles. Death of the bone of
the last finger joint necessitating removal of this part, stiffness,
crippling, and distortion of the hand, or death from blood poisoning
may ensue if prompt surgical treatment is not obtained.
[Pg 75]Treatment.—At the very outset it may be possible to stop the progress
of the felon by keeping the finger constantly wet by means of a
bandage continually saturated with equal parts of alcohol and water,
at night keeping it moist by covering with a piece of oil silk or
rubber. Tincture of iodine painted all over the end of the finger is
also useful, and the hand should be carried in a sling by day, and
slung above the head to the headboard of the bed by night. If after
twenty-four hours the pain increases, it is best to apply hot
poultices to the finger, changing them as often as they cool. If the
felon has not begun to abate by the end of forty-eight hours, the end
of the finger must be cut lengthwise right down to the bone by a
surgeon to prevent death of the bone or extension of the inflammation.
Poultices are then continued.
"Run-around" is treated also by iodine, cold applications, and, if
inflammation continues, by hot poulticing and incision with a knife;
but poulticing is often sufficient. Attention to the general health by
a physician will frequently be of service.
WEEPING SINEW; GANGLION.—This is a swelling as large as a large bean
projecting from the back or front of the wrist with an elastic or hard
feeling, and not painful or tender unless pressed on very hard. After
certain movements of the hand, as in playing the piano or, for
example, in playing tennis, some discomfort may be felt. Weeping sinew
sometimes interferes with some of the finer movements of the hand.
The[Pg 76] swelling is not red or inflamed, but of the natural color of the
skin. It does not continue to increase after reaching a moderate size,
but usually persists indefinitely, although occasionally disappearing
without treatment. The swelling contains a gelatinous substance which
is held in a little sac in the sheath of the tendon or sinew, but the
inside of the sac does not communicate with the interior of the sheath
surrounding the tendon.
Treatment.—This consists in suddenly exerting great pressure on the
swelling with the thumb, or in striking it a sharp blow with a book by
which the sac is broken. Its contents escape under the skin, and in
most cases become absorbed. If the swelling returns a very slight
surgical operation will permanently cure the trouble.
CINDERS AND OTHER FOREIGN BODIES IN THE EYE.[4]—Foreign bodies are
most frequently lodged on the under surface of the upper lid, although
the surface of the eyeball and the inner aspect of the lower lid
should also be carefully inspected. A drop of a two per cent solution
of cocaine will render painless the manipulations. The patient should
be directed to continue looking downward, and the lashes and edge of
the lid are grasped by the forefinger and thumb of the right hand,
while a very small pencil is gently[Pg 77] pressed against the upper part of
the lid, and the lower part is lifted outward and upward against the
pencil so that it is turned inside out. The lid may be kept in this
position by a little pressure on the lashes, while the cinder, or
whatever foreign body it may be, is removed by gently sweeping it off
the mucous membrane with a fold of a soft, clean handkerchief. (See
Figs. 6 and 7.)
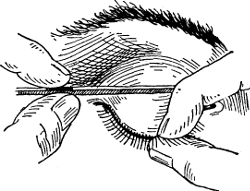 Fig. 6.
Fig. 6.
|
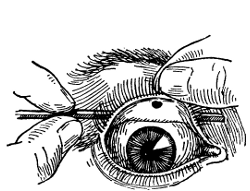 Fig. 7.
Fig. 7.
|
REMOVING A FOREIGN BODY FROM THE EYE.
In Fig. 6 note how lashes and edge of lid are grasped by forefinger
and thumb, also pencil placed against lid; in Fig. 7 lid is shown
turned inside out over pencil.
Hot cinders and pieces of metal may become so deeply lodged in the
surface of the eye that they cannot be removed by the method
recommended, or by using a narrow slip of clean white blotting-paper.
All such cases should be very speedily referred to a physician, and
the use of needles or other instruments should not be attempted by a
layman, lest permanent damage be done to the cornea and opacity
result. Such procedures[Pg 78] are, of course, appropriate for an oculist,
but when it is impossible to secure medical aid for days it can be
attempted without much fear, if done carefully, as more harm will
result if the offending body is left in place. It is surprising to see
what a hole in the surface of the eye will fill up in a few days. If
the foreign body has caused a good deal of irritation before its
removal, it is best to drop into the eye a solution of boric acid (ten
grains to the ounce of water) four times daily.
FOREIGN BODIES IN THE EAR.—Foreign bodies, as buttons, pebbles,
beans, cherry stones, coffee, etc., are frequently placed in the ear
by children, and insects sometimes find their way into the ear passage
and create tremendous distress by their struggles. Smooth,
nonirritating bodies, as buttons, pebbles, etc., do no particular harm
for a long time, and may remain unnoticed for years. But the most
serious damage not infrequently results from unskillful attempts at
their removal by persons (even physicians unused to instrumental work
on the ear) who are driven to immediate and violent action on the
false supposition that instant interference is called for. Insects, it
is true, should be killed without delay by dropping into the ear sweet
oil, castor, linseed, or machine oil or glycerin, or even water, if
the others are not at hand, and then the insect should be removed in
half an hour by syringing as recommended for wax (Vol. II, p. 35).
To remove solid bodies, turn the ear containing the body downward,
pull it outward and backward, and[Pg 79] rub the skin just in front of the
opening into the ear with the other hand, and the object may fall out.
Failing in this, syringing with warm water, as for removal of wax,
while the patient is sitting, may prove successful. The essentials of
treatment then consist, first, in keeping cool; then in killing
insects by dropping oil or water into the ear, and, if syringing
proves ineffective, in using no instrumental methods in an attempt to
remove the foreign body, but in awaiting such time as skilled medical
services can be obtained. If beans or seeds are not washed out by
syringing, the water may cause them to swell and produce pain. To
obviate this, drop glycerin in the ear which absorbs water, and will
thus shrivel the seed.
FOREIGN BODIES IN THE NOSE.—Children often put foreign bodies in
their noses, as shoe buttons, beans, and pebbles. They may not tell of
it, and the most conspicuous symptoms are the appearance of a thick
discharge from one nostril, having a bad odor, and some obstruction to
breathing on the same side. If the foreign body can be seen, the
nostril on the unobstructed side should be closed and the child made
to blow out of the other one. If blowing does not remove the body it
is best to secure medical aid very speedily.
[Pg 80]
CHAPTER IV
Fractures
How to Tell a Broken Bone—A Simple Sling—Splints and Bandage,—A
Broken Rib—Fractures of Arm, Shoulder, Hand, Hips Leg and Other
Parts.
BROKEN BONE; FRACTURE.[5]
First Aid Rule 1.—Be sure bone is broken. If broken, patient can
scarcely (if at all) move the part beyond the break, while attendant
can move it freely in his hands. If broken, grating of rough edges of
bone may be felt by attendant but should not be sought for. If broken,
limb is generally shortened.
Rule 2.—Do not try to set bone permanently. Send at once for
surgeon.
COMPOUND FRACTURE.
Important. If there is opening to the air from the break, because of
tearing of tissues by end of bone, condition is very dangerous; first
treatment may save life, by preventing infection. Before reducing
fracture,[Pg 81] and without stirring the patient much, after scrubbing your
hands very clean, note:
First Aid Rule 1.—If hairy, shave large spot about wound.
Rule 2.—Clean large area about wound with soap and water, very
gently. Then wash most thoroughly again with clean water, previously
boiled and cooled. Flood wound with cool boiled water.
Rule 3.—Cover wound with absorbent cotton (or pieces of muslin)
which has been boiled. Then attend to broken bone, as hereafter
directed, in the case of each variety of fracture.
After the bone is set, according to directions, then note:
Rule 4.—Renew pieces of previously boiled muslin from time to time,
when at all stained with discharges. Every day wash carefully about
wound, between the splints, with cool carbolic-acid solution (one
teaspoonful to a pint of hot water) before putting on the fresh
cloths.
BROKEN BONES OR FRACTURES.[6]—It frequently happens that the first
treatment of fracture devolves upon the inexperienced layman.
Immediate treatment is not essential, in so far as the repair of the[Pg 82]
fracture is directly concerned, for a broken bone does not unite for
several weeks, and if a fracture were not seen by the surgeon for a
week after its occurrence, no harm would be done, provided that the
limb were kept quiet in fair position until that time. The object of
immediate care of a broken bone is to prevent pain and avoid damage
which would ensue if the sharp ends of the broken bone were allowed to
injure the soft tissues during movements of the broken limb.
Fractures are partial or complete, the former when the bone is broken
only part way through; simple, when the fracture is a mere break of
the bone, and compound, when the end of one or both fragments push
through the skin, allowing the air with its germs to come in contact
with the wound, thus greatly increasing the danger. To be sure that a
bone is broken we must consider several points. The patient has
usually fallen or has received a severe blow upon the part. This is
not necessarily true, for old people often break the thigh bone at the
hip joint by simply making a false step.
Inability to use the limb and pain first call our attention to a
broken bone. Then when we examine the seat of injury we usually notice
some deformity—the limb or bone is out of line, and there may be an
unusual swelling. But to distinguish this condition from sprain or
bruise, we must find that there is a new joint in the course of the
bone where there ought not[Pg 83] to be any; e. g., if the leg were broken
midway between the knee and ankle, we should feel that there was
apparently a new joint at this place, that there was increased
capacity for movement in the middle of the leg, and perhaps the ends
of the fragments of bones could be heard or felt grating together.
These, then, are the absolute tests of a broken bone—unusual mobility
(or capacity for movement) in the course of the bone, and grating of
the broken fragments together. The last will not occur, of course,
unless the fragments happen to lie so that they touch each other and
should not be sought for. In the case of limbs, sudden shortening of
the broken member from overlapping of the fragments is a sure sign.
SPECIAL FRACTURES.
BROKEN RIB.—First Aid Rule.—Patient puts hands on head while
attendant puts adhesive-plaster band, one foot wide, around injured
side from spine over breastbone to line of armpit of sound side. Then
put patient to bed.
A rib is usually broken by direct violence. The symptoms are pain on
taking a deep breath, or on coughing, together with a small, very
tender point. The deformity is not usually great, if, indeed, any
exists, so that nothing in the external appearance may call the
attention to fracture. Grating between the fragments may be heard by
the patient or by the ex[Pg 84]aminer, and the patient can often place his
finger on the exact location of the break.
When it is a matter of doubt whether a rib is broken or not the
treatment for broken rib should be followed for relief of pain.
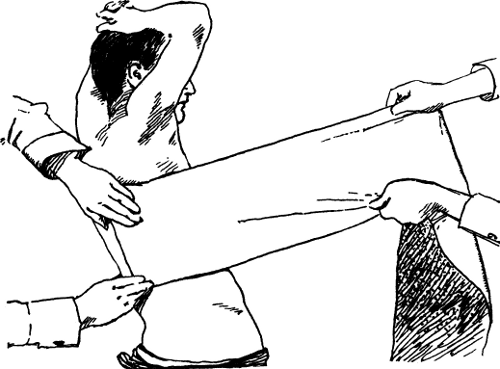 Fig. 8.
Fig. 8.
METHOD OF BANDAGING BROKEN RIB (Scudder).
Note manner of sticking one end of wide adhesive plaster along
backbone; also assistant carrying strip around injured side.
Treatment consists in applying a wide band of surgeon's adhesive
plaster, to be obtained at any drug shop. The band is made by
overlapping strips four or five inches wide, till a width of one foot
is obtained.[Pg 85] This is then applied by sticking one end along the back
bone and carrying it forward around the injured side of the chest over
the breastbone as far as a line below the armpit on the uninjured side
of the chest, i. e., three-quarters way about the chest. These four-
or five-inch strips of plaster may be cut the right length first and
laid together, overlapping about two inches, and put on as a whole,
or, what is easier, each strip may be put on separately, beginning at
the spine, five inches below the fracture, and continuing to apply the
strips, overlapping each other about two inches, until the band is
made to extend to about five inches above the point of fracture, all
the strips ending in the line of the armpit of the uninjured side.
(Fig. 8.)
If surgeon's plaster cannot be obtained, a strong unbleached cotton or
flannel bandage, a foot wide, should be placed all around the chest
and fastened as snugly as possible with safety pins, in order to limit
the motion of the chest wall. The patient will often be more
comfortable sitting up, and should take care not to be exposed to cold
or wet for some weeks, as pleurisy or pneumonia may follow. Three
weeks are required for firm union to be established in broken ribs.
COLLAR-BONE FRACTURE.
First Aid Rule.—Put patient flat on back, on level bed, with small
pillow between his shoulders; place forearm of injured side across
chest, and retain it so with bandage about chest and arm.
[Pg 86]
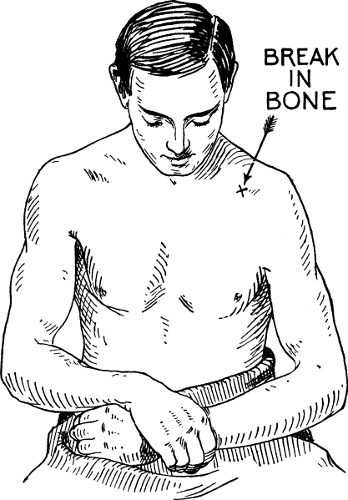 Fig. 9.
Fig. 9.
A BROKEN COLLAR BONE (Scudder).
Usual attitude of patient with a fracture of this kind; note lowering
and narrowed appearance of left shoulder.
[Pg 87]Fracture of the collar bone is one of the commonest accidents. The
bone is usually broken in the middle third. A swelling often appears
at this point, and there is pain there, especially on lifting the arm
up and away from the body. It will be noticed that the shoulder, on
the side of the injury, seems narrower and also lower than its fellow.
The head is often bent toward the injured side, and the arm of the
same side is grasped below the elbow by the other hand of the patient
and supported as in a sling. (See Fig. 9.) In examining an apparently
broken bone the utmost gentleness may be used or serious damage may
result.
Treatment.—The best treatment consists in rest in bed on a hard
mattress; the patient lying flat on the back with a small pillow
between the shoulders and the forearm of the injured side across the
chest. This is a wearisome process, as it takes from two to three
weeks to secure repair of the break. On the other hand, if the forearm
is carried in a sling, so as to raise and support the shoulder, while
the patient walks about, a serviceable result is usually obtained; the
only drawback being that an unsightly swelling remains at the seat of
the break. To make a sling, a piece of strong cotton cloth a yard
square should be cut diagonally from corner to corner, making two
right-angled triangles. Each of these will make a properly shaped
piece for a sling. (See Figs. 10 and 11.)
Fracture of the collar bone happens very often in[Pg 88] little children,
and is commonly only a partial break or splitting of the bone, not
extending wholly through the shaft so as to divide it into two
fragments, but causing little more than bending of the bone (the
"green-stick fracture").
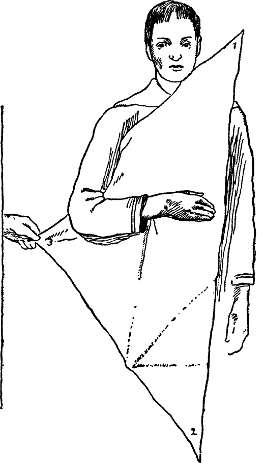 Fig. 10.
Fig. 10.
|
 Fig. 11.
Fig. 11.
The above illustration shows sling in position. It is made of cotton
cloth a yard square cut diagonally from corner to corner.
|
HOW TO MAKE A SLING (Scudder).
In Fig. 10 note three-cornered bandage; No. 2 end is carried over
right shoulder, No. 1 over left, then both fastened behind neck; No. 3
brought over and pinned.
A fall from a chair or bed is sufficient to cause the accident. A
child generally cries out on movement of[Pg 89] the arm of the injured side,
or on being lifted by placing the hands under the armpits of the
patient. A tender swelling is seen at the point of the injury of the
collar bone. A broad cotton band, with straps over the shoulders to
keep it up, should encircle the body and upper arm of the injured
side, and the hand of the same side should be supported by a narrow
sling fastened above behind the neck.
LOWER-JAW FRACTURE.
First Aid Rule.—Put fragments into place with your fingers, securing
good line of his teeth. Support lower jaw by firmly bandaging it
against upper jaw, mouth shut, using four-tailed bandage. (Fig. 12.)
Fracture of the lower jaw is caused by a direct blow. It involves the
part of the jaw occupied by the lower teeth, and is more apt to occur
in the middle line in front, or a short distance to one side of this
point. The force causing the break usually not only breaks the bone,
but also tears the gum through into the mouth, making a compound
fracture. There is immediate swelling of the gum at the point of
injury, and bleeding. The mouth can be opened with difficulty.
The condition of the teeth is the most important point to observe.
Owing to displacement of the fragments there is a difference in the
level of the teeth or line of the teeth, or both, at the place where
the fracture occurs. Also one or more of the teeth are usually
loos[Pg 90]ened at this point. In addition, unusual movement of the
fragments may be detected as well as a grating sound on manipulation.
Treatment.—The broken fragments should be pressed into place with the
fingers, and retained temporarily with a four-tailed bandage, as shown
in the cut. Feeding is done through a glass tube, using milk, broths,
and thin gruels. A mouth wash should be em[Pg 91]ployed four times daily, to
keep the mouth clean and assist in healing of the gum. A convenient
preparation consists of menthol, one-half grain; thymol, one-half
grain; boric acid, twenty grains; water, eight ounces.
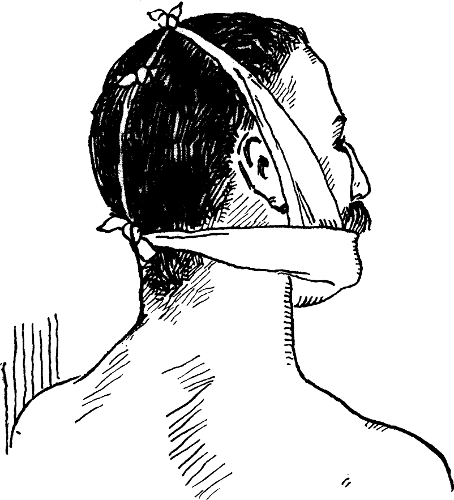 Fig. 12.
Fig. 12.
BANDAGE FOR A BROKEN JAW (American Text-Book).
Above cut shows a four-tailed bandage; note method of tying; one strip
supports lower jaw; the other holds it in place against upper jaw.
SHOULDER-BLADE FRACTURE.
First Aid Rule.—There is no displacement. Bandage fingers, forearm,
and arm of affected side, and put this arm in sling. Fasten slung arm
to body with many turns of a bandage, which holds forearm against
chest and arm against side.
Shoulder-blade fracture occasions pain, swelling, and tenderness on
pressure over the point of injury. On manipulating the bone a grating
sound may be heard and unnatural motion detected. The treatment
consists in bandaging the forearm and arm on the injured side from
below upward, beginning at the wrist; slinging the forearm bent at a
right angle across the front of the body, suspended by a narrow sling
from the neck, and then encircling the body and arm of the injured
side from shoulder to elbow with a wide bandage applied under the
sling, which holds the arm snugly against the side. This bandage is
prevented from slipping down by straps attached to it and carried over
each shoulder.
ARM FRACTURE.
First Aid Rule.—Pad two pieces of thin board nine by three inches
with handkerchiefs. Carefully[Pg 92] pull fragments of bone apart, grasping
lower fragment near elbow while assistant pulls gently on upper
fragment near shoulder. Put padded boards (splints) one each side of
the fracture, and wind bandage about their whole length, tightly
enough to keep bony fragments firm in position. Put forearm and hand
in sling.
In fracture of the arm between the shoulder and elbow, swelling and
shortening may give rise to deformity. Pain and abnormal motion are
symptoms, while a grating sound may be detected, but manipulation of
the arm for this purpose should be avoided. The surface is apt soon to
become black and blue, owing to rupture of the blood vessels beneath
the skin.
The hand and forearm should be bandaged from below upward to the
elbow. The bone is put in place by grasping the patient's elbow and
pulling directly down in line with the arm, which is held slightly
away from the side of the patient, while an assistant steadies and
pulls up the shoulder. Then a wedge-shaped pad, long enough to reach
from the patient's armpit to his elbow (made of cotton wadding or
blanketing sewed in a cotton case) and about four inches wide and
three inches thick at one end, tapering up to a point at the other, is
placed against the patient's side with the tapering end uppermost in
the armpit and the thick end down. This pad is kept in place by a
strip of surgeon's adhesive plaster, or bandage passing through[Pg 93] the
small end of the wedge, and brought up and fastened over the shoulder.
 Fig. 13.
Fig. 13.
|
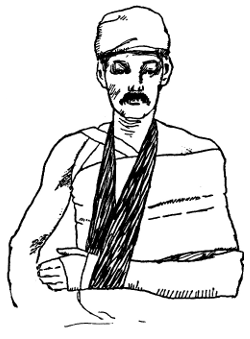 Fig. 14.
Fig. 14.
|
BANDAGE FOR BROKEN ARM (Scudder).
In Fig. 13 note splints secured by adhesive plaster; also pad in
armpit; in Fig. 14 see wide bandage around body; also sling.
While the arm is pulled down from the shoulder, three strips of
well-padded tin or thin board (such as picture-frame backing) two
inches wide and long enough to reach from shoulder to elbow, are laid
against the front, outside, and back of the arm, and secured by
encircling strips of surgeon's plaster or bandage. The arm is then
brought into the pad lying against the side under the armpit, and is
held there firmly by a wide bandage surrounding the arm and[Pg 94] entire
chest, and reaching from the shoulder to elbow. It is prevented from
slipping by strips of cotton cloth, which are placed over the
shoulders and pinned behind and before to the top of the bandage. The
wrist is then supported in a sling, not over two inches wide, with the
forearm carried in a horizontal position across the front of the body.
Firm union of the broken arm takes place usually in from four to six
weeks. (See Figs. 13 and 14.)
FOREARM FRACTURE.
First Aid Rule.—Set bones in proper place by pulling steadily on
wrist while assistant holds back the upper part of the forearm. If
unsuccessful, leave it for surgeon to reduce after "period of
inaction" comes, a few days later, when swelling subsides. If
successful, put padded splints (pieces of cigar box padded with
handkerchiefs) one on each side, front and back, and wind a bandage
about whole thing to hold it immovably.
Two bones enter into the structure of the forearm. One or both of
these may be broken. The fracture may be simple or compound,[7] when
the soft parts are damaged and the break of the bone communicates with
the air, the ends of the bone even projecting through the skin.
[Pg 95]In fracture of both bones there is marked deformity, caused by
displacement of the broken fragments, and unusual motion may be
discovered; a grating sound may also be detected but, as stated
before, manipulation of the arm should be avoided.
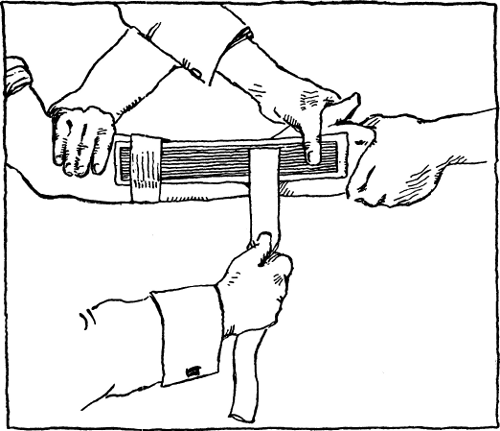 Fig. 15.
Fig. 15.
SETTING A BROKEN FOREARM (Scudder).
See manner of holding arm and applying adhesive plaster strips; one
splint is shown, another is placed back of hand and forearm.
When only one bone is broken the signs are not so marked, but there is
usually a very tender point at the seat of the fracture, and an
irregularity of the sur[Pg 96]face of the bone may be felt at this point. If
false motion and a grating sound can also be elicited, the condition
is clear. The broken bones are put into their proper place by the
operator who pulls steadily on the wrist, while an assistant grasps
the upper part of the forearm and pulls the other way. The ends of the
fragments are at the same time pressed into place by the other hand of
the operator, so that the proper straight line of the limb is
restored.
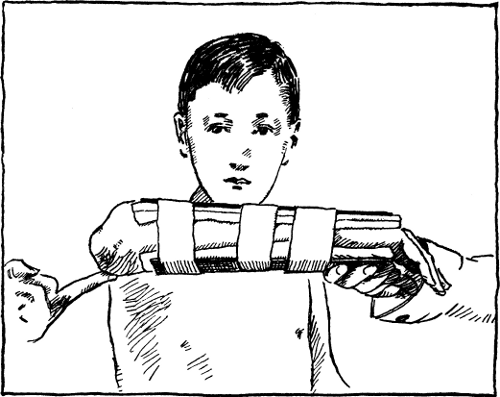 Fig. 16.
Fig. 16.
FRACTURE OF BOTH BONES IN FOREARM (Scudder).
This cut shows the position and length of the two padded splints; also
method of applying adhesive plaster.
[Pg 97]After the forearm is set, it should be held steadily in the following
position while the splints are applied. The elbow is bent so that the
forearm is held at right angles with the arm horizontally across the
front of the chest with the hand extended, open palm toward the body
and thumb uppermost. The splints, two in number, are made of wood
about one-quarter inch thick, and one-quarter inch wider than the
forearm. They should be long enough to reach from about two inches
below the elbow to the root of the fingers. They are covered smoothly
with cotton wadding, cotton wool, or other soft material, and then
with a bandage. The splints are applied to the forearm in the
positions described, one to the back of the hand and forearm, and the
other to the palm of the hand and front of the forearm.
Usually there are spaces in the palm of the hand and front of the
wrist requiring to be filled with extra padding in addition to that on
the splint. The splints are bound together and to the forearm by three
strips of surgeon's adhesive plaster or bandage, about two inches
wide. One strip is wound about the upper ends of the splints, one is
wrapped about them above the wrist, and the third surrounds the back
of the hand and palm, binding the splints together below the thumb.
The splints should be held firmly in place, but great care should be
exercised to use no more force in applying the adhesive plaster or
bandage than is necessary to accomplish this end, as it is easy to
stop the cir[Pg 98]culation by pressure in this part. There should be some
spring felt when the splints are pressed together after their
application. A bandage is to be applied over the splints and strips of
plaster, beginning at the wrist and covering the forearm to the elbow,
using the same care not to put the bandage on too firmly. The forearm
is then to be held in the same position by a wide sling, as shown
above. (See Figs. 15, 16, 17.)
 Fig. 17.
Fig. 17.
DRESSING FOR BROKEN FOREARM (Scudder).
Proper position of arm in sling; note that hand is unsupported with
palm turned inward and thumb uppermost.
[Pg 99]Four weeks are required to secure firm union after this fracture. When
the fracture is compound the same treatment should be employed as
described under Compound Fracture of Leg, p. 116.
FRACTURE OF THE WRIST; COLLES'S FRACTURE.—This is a break of the
lower end of the bone on the thumb side of the wrist, and much the
larger bone in this part of the forearm. The accident happens when a
person falls and strikes on the palm of the hand; it is more common in
elderly people. A peculiar deformity results. A hump or swelling
appears on the back of the wrist, and a deep crease is seen just above
the hand in front. The whole hand is also displaced at the wrist
toward the thumb side.
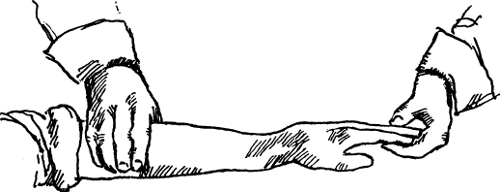 Fig. 18.
Fig. 18.
A BROKEN WRIST (Scudder).
Characteristic appearance of a "Colles's fracture"; note backward
displacement of hand at wrist; also fork-shaped deformity.
It is not usual to be able to detect abnormal motion in the case of
this fracture, or to hear any grating sound on manipulating the part,
as the ends of the[Pg 100]
[Pg 101] fragments are generally so jammed together that
it is necessary to secure a surgeon as soon as possible to pull them
apart under ether, in order to remedy the existing "silver-fork"
deformity. (See Figs. 18, 19, 20, 21, 22.)
Treatment.—Until medical aid can be obtained the same sort of splints
should be applied, and in the same way as for the treatment of
fractured forearm. If the deformity is not relieved a stiff and
painful joint usually persists. It is sometimes impossible for the
most skillful surgeon entirely to correct the existing deformity, and
in elderly people some stiffness and pain in the wrist and fingers are
often unavoidable results.
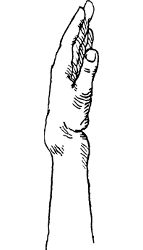 Fig. 19.
Fig. 19.
|
 Fig. 20.
Fig. 20.
|
| |
|
 Fig. 21.
Fig. 21.
|
 Fig. 22.
Fig. 22.
|
FRACTURE OF THE WRIST (Scudder).
Above illustrations show deformities resulting from a broken wrist;
Figs. 19 and 20 the crease at base of thumb; Fig. 21 hump on back of
wrist; Fig. 22 twisted appearance of hand.
FRACTURE OF BONE OF HAND, OR FINGER.
First Aid Rule.—Set fragments of bone in place by pulling with one
hand on finger, while pressing fragments into position with other
hand. Put on each side of bone a splint made of cigar box, padded with
folded handkerchiefs, and retain in place with bandage wound about
snugly. Put forearm and hand in sling.
This accident more commonly happens to the bones corresponding to the
middle and ring finger, and occurs between the knuckle and the wrist,
appearing as a swelling on the back of the hand. On looking at the
closed fist it will be seen that the knuckle corresponding to the
broken bone in the back of the hand has ceased to be prominent, and
has sunken down below[Pg 102] the level of its fellows. The end of the
fragment nearer the wrist can generally be felt sticking up in the
back of the hand.
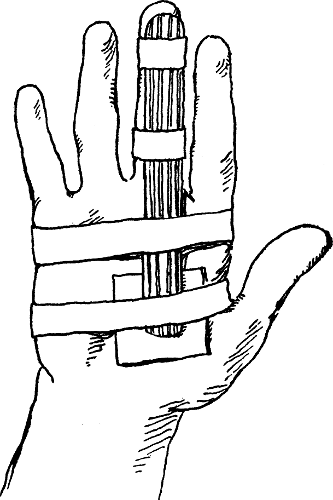 Fig. 23.
Fig. 23.
A BROKEN FINGER (Scudder).
Note splint extending from wrist to tip of finger; also manner of
applying adhesive plaster strips and pad in palm.
If the finger corresponding to the broken bone in the back of the hand
be pulled on forcibly, and the fragments be held between the thumb and
forefinger of the other hand of the operator, pain and abnormal
mo[Pg 103]tion may be detected, and the ends of the broken bone pressed into
place. A thin wooden splint, as a piece of cigar box, about an inch
wide at base and tapering to the width of the finger should be applied
to the palm of the hand extending from the wrist to a little beyond
the finger tip, secured by strips of adhesive plaster, as in the cut,
and covered by a bandage. The splint should be well padded, and an
additional pad should be placed in the palm of the hand over the point
of fracture. Three weeks are required for firm union, and the hand
should not be used for a month.
It is usually easy to recognize a broken bone in a finger, unless the
break is near a joint, when it may be mistaken for a dislocation.
Pain, abnormal motion, and grating between the fragments are observed.
If there is deformity, it may be corrected by pulling on the injured
finger with one hand, while with the other the fragments are pressed
into line. A narrow, padded wooden or tin splint is applied, as in the
cut (p. 102), reaching from the middle of the palm to the finger tip.
Any existing displacement of the broken bone can be relieved by using
pressure with little pads of cotton held in place by narrow strips of
adhesive plaster where it is needed to keep the bone in line. The
splint may be removed in two weeks and a strip of adhesive plaster
wound about the finger to support it for a week or two more.
In fracture of the thumb, the splint is applied along the back instead
of on the palm side.
[Pg 104]HIP FRACTURE.
First Aid Rule.—Put patient flat on back in bed, with limb wedged
between pillows till surgeon arrives.
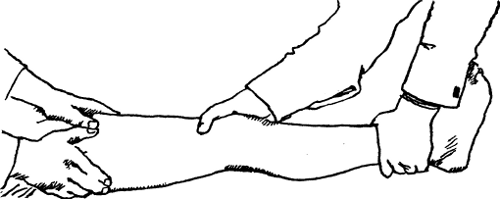 Fig. 24.
Fig. 24.
TREATING A BROKEN HIP (Scudder).
Note the manner of straightening leg and getting broken bone into
line; also assistant carefully steadying the thigh.
A fracture of the hip is really a break of that portion of the thigh
bone which enters into the socket of the pelvic bone and forms the hip
joint. It occurs most commonly in aged people as a result of so slight
an accident as tripping on a rug, or in falling on the floor from the
standing position, making a misstep, or while attempting to avoid a
fall. When the accident has occurred the patient is unable to rise or
walk, and suffers pain in the hip joint. When he has been helped to
bed it will be seen that the foot of the injured side is turned out,
and the leg is perhaps apparently shorter than its fellow. There is
pain on movement of the limb,[Pg 105] and the patient cannot raise his heel,
on the injured side, from the bed. Shortening is an important sign.
With the patient lying flat on the back and both legs together in a
straight line with the body, measurements from each hip-bone are made
with a tape to the bony prominence on the inside of each ankle, in
turn. One end of the tape is held at the navel and the other is swung
from one ankle to the other, comparing the length of the two limbs.
Shortening of less than half an inch is of no importance as a sign of
fracture. The fragments of broken bone are often jammed together
(impacted) so that it is impossible to get any sound of grating
between them, and it is very unwise to manipulate the leg or hip
joint, except in the gentlest manner, in an attempt to get this
grating. If the ends of the fragments become disengaged from each
other it often happens that union of the break never occurs.
 Fig. 25.
Fig. 25.
TREATMENT FOR FRACTURED HIP (Scudder).
Note method of holding splints in place with muslin strips; one above
ankle, one below and one above knee, one in middle and one around
upper part of thigh.
The treatment simply consists in keeping the pa[Pg 106]tient quiet on a hard
mattress, with a small pillow under the knee of the injured side and
the limb steadied on either side by pillows or cushions until a
surgeon can be obtained. (See Thigh-bone Fracture.)
THIGH-BONE FRACTURE.
First Aid Rule.—Prepare long piece of thin board which will reach
from armpit to ankle, and another piece long enough to reach from
crotch to knee, and pad each with folded towels or blanket.
While one assistant holds body back, and another assistant pulls on
ankle of injured side, see that the fragments are separated and
brought into good line, and then apply the splints, assistants still
pulling steadily, and fasten the splints in place with bandage, or by
tying several cloths across at three places above the knee and two
places below the knee.
Finally, pass a wide band of cloth about the body, from armpit to
hips, inclosing the upper part of the well-padded splint, and fasten
it snugly. The hollow between splint and waist must be filled with
padding before this wide cloth is applied.
In fracture of the thigh bone (between the hip and knee), there is
often great swelling about the break. The limb is helpless and
useless. There is intense pain and abnormal position in the injured
part, besides deformity produced by the swelling. The foot of the
injured limb is turned over to one side or the other,[Pg 107] owing to a
rolling over of the portion of the limb below the break. With both
lower limbs in line with the body, and the patient lying on the back,
measurements are made from each hip-bone to the prominence on the
inside of either ankle joint. Shortening of the injured leg will be
found, varying from one to over two inches, according to the
overlapping and displacement of the fragments.
Treatment.—To set this fracture temporarily, a board about five
inches wide and long enough to reach from the armpit to the foot
should be padded well with towels, sheets, shawls, coats, blanket, or
whatever is at hand, and the padding can best be kept in place by
surgeon's adhesive plaster, bicycle tape, or strips of cloth.[8]
Another splint should be provided as wide as the thigh and long enough
to reach along the back of the leg from the middle of the calf to the
buttock, and also padded in the same way. A third splint should be
prepared in the same manner to go inside the leg, reaching from the
crotch to the inside of the foot. Still a fourth splint made of a thin
board as wide as the thigh, extending from the upper part of the thigh
to just above the knee, is padded for application to the front of the
thigh.
When these are made ready and at hand, the leg should be pulled on
steadily but carefully straight away from the body to relax the
muscles, an assistant hold[Pg 108]ing the upper part of the thigh and pulling
in the opposite direction. Then, when the leg has been straightened
out and the thigh bone seems in fair line, the splints should be
applied; the first to the outside of the thigh and body, the second
under the calf, knee, and thigh; the third to the inside of the whole
limb, and the fourth to the front of the thigh.
Wide pads should be placed over the ribs under the outside splint to
fill the space above the hips and under the armpit. Then all four
splints are drawn together and held in place by rubber-plaster straps
or strips of strong muslin applied as follows: one above the ankle;
one below the knee; one above the knee; one in the middle of the
thigh, and one around the upper part of the thigh. A wide band of
strong muslin or sheeting should then be bound around the whole body
between the armpits and hips, inclosing the upper part of the outside
splint. The patient can then be borne comfortably upon a stretcher
made of boards and a mattress or some improvised cushion. (See Figs.
24 and 25.)
When the patient can be put immediately to bed after the injury, and
does not have to be transported, it is only necessary to apply the
outer, back, and front splints, omitting the inner splint. It is
necessary for the proper and permanent setting of a fractured thigh
that a surgeon give an anæsthetic and apply the splints while the
muscles are completely relaxed. It is also essential that the muscles
be kept from contracting[Pg 109] thereafter by the application of a fifteen-
or twenty-pound weight to the leg, after the splints are applied, but
it is possible to outline here only the proper first-aid treatment.
KNEEPAN FRACTURE.
First Aid Rule.—Pain is immediate and intense. Separated fragments
may be felt at first. Swelling prompt and enormous. Even if not sure,
follow these directions for safety.
Prepare splint: thin board, four inches wide, and long enough to
reach from upper part of thigh to just above ankle. Pad with folded
piece of blanket or soft towels. Place it behind leg and thigh;
carefully fill space behind knee with pad; fasten splint to limb with
three strips of broad adhesive plaster, one around upper end of
splint, one around lower end, one just below knee.
Lay large flat, dry sponge over knee thus held, and bandage this in
place. Keep sponge and bandage wet with ice water. If no sponge is
available, half fill rubber hot-water bottle with cracked ice, and lay
this over knee joint. Put patient to bed.
Fracture of kneepan is caused either by direct violence or muscular
strain. It more frequently occurs in young adults. Immediate pain is
felt in the knee and walking becomes impossible; in fact, often the
patient cannot rise from the ground after the acci[Pg 110]dent. Swelling at
first is slight, but increases enormously within a few hours.
Immediately after the injury it may be possible to feel the separate
broken fragments of the kneepan and to recognize that they are
separated by a considerable space if the break is horizontally across
the bone.
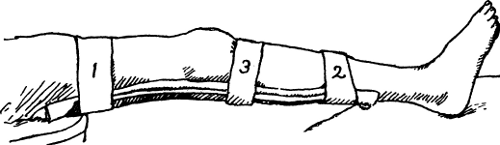 Fig. 26.
Fig. 26.
A BROKEN KNEEPAN (Scudder).
A padded splint, supporting knee, is shown reaching from ankle to
thigh. Note number and location of adhesive plaster strips.
Nothing can be done to set the fracture until the swelling about the
joint has been reduced, so that the first treatment consists in
securing immediate rest for the kneejoint, and immobility of the
fragments. A splint made of board, about a quarter of an inch thick
and about four inches wide for an adult, reaching from the upper part
of the thigh above to a little above the ankle below, is applied to
the back of the limb and well padded, especially to fill the space
behind the knee. The splint is attached to the limb by straps of
adhesive plaster two inches and a half wide; one around the lower end
of the splint, one around the upper part, and the third placed just
below the knee. To prevent and[Pg 111] arrest the swelling and pain, pressure
is then made on the knee by bandaging.
One of the best methods (Scudder's) is to bind a large, flat, dry
sponge over the knee and then keep it wet with cold water; or to apply
an ice bag directly to the swollen knee; a splint in either case being
the first requisite. The patient should of course be put to bed as
soon as possible after the accident, and should lie on the back with
the injured leg elevated on a pillow with a cradle to keep the clothes
from pressing on the injured limb. (See cut, p. 110.)
FRACTURE OF LEG BONES, BETWEEN KNEE AND ANKLE.
First Aid Rule.—Handle very carefully; great danger of making
opening to surface. Special painful point, angle or new joint in bone,
disability, and grating felt will decide existence of break. Let
assistant pull on foot, to separate fragments, while you examine part
of supposed break. If only one bone is broken, there may be no
displacement.
Put patient on back. While two assistants pull, one on ankle and one
on thigh at knee, thus separating fragments, slide pillow lengthwise
under knee, and, bringing its edges up about leg, pin them snugly
above leg.
Prepare three pieces of thin wood, four inches wide and long enough
to reach from sole of foot to a point four inches above knee. While
assistants pull on limb[Pg 112] again, as before, put one splint each side
and third behind limb, and with bandage or strips of sticking plaster
fasten these splints to the leg inclosed in its pillow as tight as
possible.
In fracture of the leg between the knee and ankle we have pain,
angular deformity or an apparent false joint in the leg, swelling and
tenderness over the seat of fracture, together with inability to use
the injured leg. Two bones form the framework of the leg; the inner,
or shinbone, the sharp edge of which can be felt in front throughout
most of its course, being much the larger and stronger bone. When both
bones are broken, the displacement of the fragments, abnormal motion
and consequent deformity, are commonly apparent, and a grating sound
may be heard, but should not be sought for.
 Fig. 27.
Fig. 27.
FRACTURE OF BOTH LEG BONES (Scudder).
This cut shows the peculiar deformity in breaks of this kind; see
position of kneepan; also prominence of broken bone above ankle.
An open wound often communicates with the break, making the fracture
compound, a much more serious condition. To avoid making the fracture
a compound[Pg 113] one, during examination of the leg, owing to the sharp
ends of the bony fragments, the utmost gentleness should be used.
Under no circumstances attempt to move the fragments from side to
side, or backward and forward, in an effort to detect the grating
sound often caused by the ends of broken bones. The greatest danger
lies in the desire to do too much. We again refer the reader to First
Aid Rule 1.
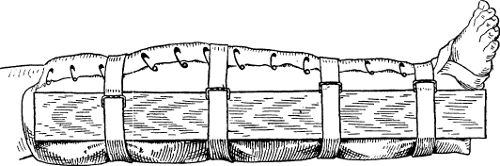 Fig. 28.
Fig. 28.
BANDAGE FOR BROKEN LEG (Scudder).
Note the pillow brought up around leg and edges pinned together; also
length and method of fastening splint with straps.
When one bone is broken there may be only a point of tenderness and
swelling about the vicinity of the break and no displacement or
grating sound. When in doubt as to the existence of a fracture always
treat the limb as if a fracture were present. "Black and blue"
discoloration of the skin much more extensive than that following
sprain will become evident over the whole leg within twenty-four
hours.
Treatment.—When a surgeon cannot be obtained,[Pg 114] the following
temporary pillowdressing, recommended by Scudder in his book on
fractures, is one of the best. With the patient on his back, the leg
having been straightened and any deformity removed as far as possible
by grasping the foot and pulling directly away from the body while an
assistant steadies the thigh, a large, soft pillow, inclosed in a
pillowcase, is placed under the leg. The sides of the pillow are
brought well up about the leg and the edges of the pillowcase are
pinned together along the front of the leg.
Then three strips of wood about four inches wide, three-sixteenths to
a quarter of an inch thick, and long enough to reach from the sole of
the foot to about four inches above the knee, are placed outside of
the pillow along the inner and outer aspects of the leg and beneath
it. The splints are held in place, with the pillow as padding beneath,
by four straps of webbing (or if these cannot be obtained, by strips
of stout cloth, adhesive plaster, or even rope); but four pads made of
folded towels should be put under the straps where they cross the
front of the leg where little but the pillowcase overlaps. These
straps are applied thus: one above the knee, one above the ankle, and
the other two between these two points, holding all firmly together.
This dressing may be left undisturbed for a week or even ten days if
necessary. (See Figs. 27 and 28.)
The leg should be kept elevated after the splints are applied, and
steadied by pillows placed either side[Pg 115] of it. From one to two months
are required to secure union in a broken leg in adults, and from three
to five months elapse before the limb is completely serviceable. In
children the time requisite for a cure is usually much shorter.
ANKLE-JOINT FRACTURE.
First Aid Rule.—One or both bones of leg may be broken just above
ankle. Foot is generally pushed or bent outward. Prepare two pieces of
thin wood, four inches wide and long enough to go from sole of foot to
just below knee:—the splints. Pad them with folded towels or pieces
of blanket.
While assistants pull bones apart gently, one pulling on knee, other
pulling on foot and turning it straight, apply the splints, one each
side of the leg.
A fracture of the ankle joint is really a fracture of the lower
extremities of the bones of the leg. There are present pain and great
swelling, particularly on the inner side of the ankle at first, and
the whole foot is pushed and bent outward. The bony prominence on the
inner side of the ankle is unduly marked. The foot besides being bent
outward is also displaced backward on the leg. This fracture might be
taken for a dislocation or sprain of the ankle. Dislocation of the
ankle without fracture is very rare, and when the foot is returned to
its proper position it will stay there, while in fracture the foot
drops back to its former displaced[Pg 116] state. In sprained ankle there are
pain and swelling, but not the deformity caused by the displacement of
the foot.
This fracture may be treated temporarily by returning the foot to its
usual position and putting on side splints and a back splint, as
described for the treatment of fracture of the leg.
COMPOUND OR OPEN FRACTURE OF THE LEG.—This condition may be produced
either by the violence which caused the fracture also leading to
destruction of the skin and soft parts beneath, or by the end of a
bony fragment piercing the muscles and skin from within. In either
event the result is much more serious than that of an ordinary simple
fracture, for germs can gain entrance through the wound in the skin
and cause inflammation with partial destruction or death of the part.
Treatment.—Immediate treatment is here of the utmost value. It is
applicable to open or compound fracture in any part of the body. The
area for a considerable distance about the wound, if covered with
hair, should be shaved. It should then be washed with warm water and
soap by means of a clean piece of cotton cloth or absorbent cotton.
Then some absorbent cotton or cotton cloth should be boiled in water
in a clean vessel for a few minutes, and, after the operator has
thoroughly washed his hands, the boiled water (when sufficiently cool)
should be applied to the wounded area and surrounding parts with the
boiled[Pg 117] cotton, removing in the most painstaking way all visible and
invisible dirt. By allowing some of the water to flow over the wound
from the height of a few feet this result is favored. Finally some of
the boiled cotton, which has not been previously touched, is spread
over the wound wet, and covered with clean, dry cotton and bandaged.
Splints are then applied as for simple fracture in the same locality
(p. 113). If a fragment of bone projects through the wound it may be
replaced after the cleansing just described, by grasping the lower
part of the limb and pulling in a straight line of the limb away from
the body, while an assistant holds firmly the upper part of the limb
and pulls in the opposite direction. During the whole process neither
the hands of the operator nor the boiled cotton should come in contact
with anything except the vessel containing the boiled water and the
patient.
[Pg 118]
CHAPTER V
Dislocations
How to Tell a Dislocation—Reducing a Dislocated Jaw—Stimson's
Method of Treating a Dislocated Shoulder—Appearance of Elbow when Out
of Joint—Hip Dislocations—Forms of Bandages.
DISLOCATIONS; BONES OUT OF JOINT.
JAW.—Rare. Mouth remains open, lower teeth advanced forward.
First Aid Rule 1.—Protect your thumbs. Put on thick leather gloves,
or bind them with thick bandage.
Rule 2.—Assistant steadies patient from behind, with hands both
sides of his head, operator presses downward and backward with his
thumbs on back teeth of patient, each side of patient's jaw, while the
chin is grasped between forefingers and raised upward. Idea is to
stretch the ligament at jaw joint, and swing jaw back while pulling on
this ligament. (Fig. 29.)
Rule 3.—Tie jaw with four-tailed bandage up against upper jaw for a
week. (Fig. 12, p. 90.)
SHOULDER.—Common accident. No hurry. See p. 122.
ELBOW.—Rare. No hurry. See p. 125.
[Pg 119]HIP.—No hurry. See p. 129.
KNEE.—Rare. Easily reduced. Head of lower bone (tibia) is moved to
one side; knee slightly bent.
First Aid Rule 1.—Put patient on back.
Rule 2.—Flex thigh on abdomen and hold it there.
Rule 3.—Grasp leg below knee and twist it back and forth, and
straighten knee.
DISLOCATIONS.—A dislocation is an injury to a joint wherein the ends
of the bones forming a joint are forced out of place. A dislocation is
commonly described as a condition in which a part (as the shoulder) is
"out of joint" or "out of place." A dislocation must be distinguished
from a sprain, and from a fracture near a joint. In a sprain, as has
been stated (p. 65), the bones entering into the formation of the
joint are perhaps momentarily displaced, but return into their proper
place when the violence is removed. But, owing to greater injury, in
dislocation the head of the bone slips out of the socket which should
hold it, breaks through the ligaments surrounding the joint, and
remains permanently out of place. For this reason there is a peculiar
deformity, produced by the head of the bone's lying in its new and
unnatural situation, which is not seen in a sprain.
Also, the dislocated joint cannot be moved by the patient or by
another person, except within narrow limits, while a sprained joint
can be moved, with the production of pain it is true, but without any
mechan[Pg 120]ical obstacle. In the case of fracture near a joint there is
usually increased movement in some new direction. When a dislocated
joint is put in proper place it stays in place, whereas when a
fractured part is reduced there is nothing to keep it in place and, if
let alone, it quickly resumes its former faulty position.
Only a few of the commoner dislocations will be considered here, as
the others are of rare occurrence and require more skill than can be
imparted in a book intended for the laity. The following instructions
are not to be followed if skilled surgical attendance can be secured;
they are intended solely for those not so fortunately situated.
DISLOCATION OF THE JAW.—This condition is caused by a blow on the
chin, or occurs in gaping or when the mouth is kept widely open during
prolonged dental operations. The joint surface at the upper part of
the lower jaw, just in front of the entrance to the ear, is thrown out
of its socket on one side of the face, or on both sides. If the jaw is
put out of place on both sides at once, the chin will be found
projecting so that lower front teeth jut out beyond the upper front
teeth, the mouth is open and cannot be closed, and the patient is
suffering considerable pain. When the jaw is dislocated on one side
only, the chin is pushed over toward the uninjured side of the face,
which gives the face a twisted appearance; the mouth is partly open
and fixed in that position. A depression is seen on the injured side
in front of the[Pg 121] ear, while a corresponding prominence exists on the
opposite side of the face, and the lower front teeth project beyond
the upper front teeth.
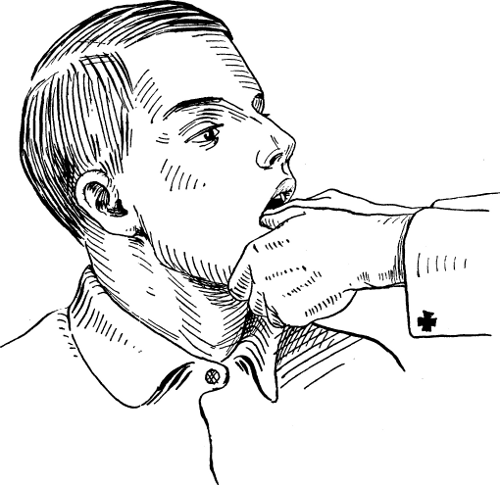 Fig. 29.
Fig. 29.
REDUCING DISLOCATION OF JAW (American Text-Book).
Thumbs placed upon last molar teeth on each side; note jaw grasped
between fingers and thumbs to force it into place.
Treatment.—A dislocation of one side of the jaw is treated in the
same manner as that of both sides.
The dislocation may sometimes be reduced by[Pg 122] placing a good-sized cork
as far back as possible between the back teeth of the upper and lower
jaws (on one or both sides, according as the jaw is out of place on
one or both sides), and getting the patient to bite down on the cork.
This may pry the jaw back into place.
The common method is for the operator to protect both thumbs by
wrapping bandage about his thumbs, or wearing leather gloves, and
then, while an assistant steadies the head, the operator presses
downward and backward on the back teeth of the patient on each side of
the lower jaw with both thumbs in the patient's mouth, while the chin
is grasped beneath by the forefingers of each hand and raised upward.
When the jaw slips into place it should be maintained there by a
bandage placed around the head under the chin and retained there for a
week. During this time the patient should be fed on liquids through a
tube, so that it will not be necessary for him to open his mouth to
any extent. (See Fig. 29.)
DISLOCATION OF THE SHOULDER.—This is by far the most common of
dislocations in adults, constituting over one-half of all such
accidents affecting any of the joints. It is caused by a fall or blow
on the upper arm or shoulder, or by falling upon the elbow or
outstretched hand. The upper part (or head) of the bone of the arm
(humerus) slips downward out of the socket or, in some cases, inward
and forward. In either case the general appearance and treatment[Pg 123]
[Pg 124] of
the accident are much the same. The shoulder of the injured side loses
its fullness and looks flatter in front and on the side. The arm is
held with the elbow a few inches away from the side, and the line of
the arm is seen to slope inwardly toward the shoulder, as compared
with the sound arm.
The injured arm cannot be moved much by the patient, although it can
be lifted up and away from the side by another person, but cannot be
moved so that, with the elbow against the front of the chest, the hand
of the injured arm can be laid on the opposite shoulder. Neither can
the arm, with the elbow at a right angle, be made to touch the side
with the elbow, without causing great pain.
Treatment.—One of the simplest methods (Stimson's) of reducing this
dislocation consists in placing the patient on his injured side on a
canvas cot, which should be raised high enough from the floor on
chairs, and allowing the injured arm to hang directly downward toward
the floor through a hole cut in the cot, the hand not touching the
floor. Then a ten-pound weight is attached to the wrist. The gradual
pull produced by this means generally brings the shoulder back into
place without pain and within six minutes. (Fig. 30.)
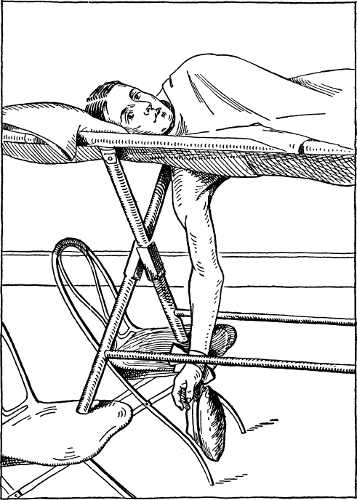 Fig. 30.
Fig. 30.
TREATING A DISLOCATED SHOULDER.
(Reference Handbook.)
Patient lying on injured side; note arm hanging through hole in cot
raised from floor on chairs; also weight attached to wrist.
The more ordinary method consists in putting the patient on his back
on the floor, the operator also sitting on the floor with his
stockinged foot against the patient's side under the armpit of the
injured shoulder and grasping the injured arm at the elbow, he pulls[Pg 125]
the arm directly outward (i. e., with the arm at right angles with the
body) and away from the trunk. An assistant may at the same time aid
by lifting the head of the arm bone upward with his fingers in the
patient's armpit and his thumbs over the injured shoulder.
If the arm does not go into place easily by one of these methods it is
unwise to continue making further attempts. Also if the shoulder has
been dislocated several days, or if the patient is very muscular, it
will generally be necessary that a surgeon give ether in order to
reduce the dislocation. It is entirely possible for a skillful surgeon
to secure reduction of a dislocation of the shoulder several weeks
after its occurrence. After the dislocation has been relieved the arm,
above the elbow, should be bandaged to the side of the chest and the
hand of the injured side carried in a sling for ten days.
DISLOCATION OF THE ELBOW.—This is more frequent in children, and is
usually produced by a fall on the outstretched hand. The elbow is
thrown out of joint, so that the forearm is displaced backward on the
arm, in the more usual form of dislocation. The elbow joint is swollen
and generally held slightly bent, but cannot be moved to any extent
without great pain. The tip of the elbow projects at the back of the
joint more than usual, while at the front of the arm the distance
between the wrist and the bend of the elbow is less than that of the
sound arm. (See cut, p. 126.)
[Pg 126]
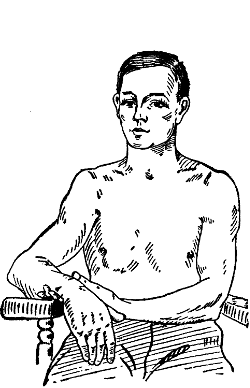 Fig. 31.
Fig. 31.
Above cut shows characteristic appearance of a dislocated shoulder;
note loss of fullness; also elbow held away from side and inward
sloping of arm.
|
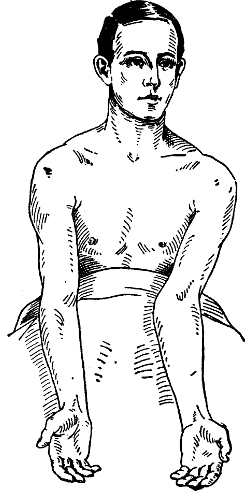 Fig. 32.
Fig. 32.
|
DISLOCATED ELBOW AND SHOULDER.
(American Text-Book.)
Fig. 32 shows dislocation of elbow backward; note swollen condition of
left elbow held slightly bent; also the projection of back of joint.
For further proof that the elbow is out of joint we must compare the
relations of three points in each elbow. These are the two bony
prominences on each side of the joint (belonging to the bone of the
arm above the elbow) and the bony prominence that forms the tip of the
elbow which belongs to the bone of the forearm.
[Pg 127]
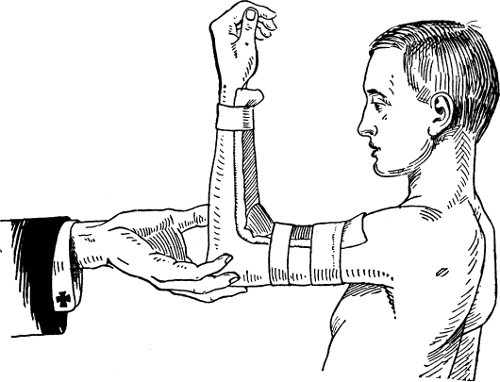 Fig. 33.
Fig. 33.
TREATMENT OF DISLOCATED ELBOW (Scudder).
Note padded right-angled tin splint; also three strips of surgeon's
plaster on arm and forearm.
In dislocation backward of the forearm, the tip of the elbow is
observed to be farther back, in relation to the two bony prominences
at the side of the joint, than is the case in the sound elbow. This is
best ascertained by touching the three points on the patient's elbow
of each arm in turn with the thumb and middle finger on each of the
prominences on the side of the joint, while the forefinger is placed
on the tip of the elbow. The lower end of the bone of the upper[Pg 128] arm
is often seen and felt very easily just above the bend of the elbow in
front, as it is thrown forward (see Fig. 32, p. 126).
Fracture of the lower part of the bone of the arm above the elbow
joint may present much the same appearance as the dislocation we are
describing, but then the whole elbow is displaced backward, and the
relation of the three points described above is the same in the
injured as in the uninjured arm. Moreover in fracture the deformity,
when relieved, will immediately recur when the arm is released, as
there is nothing to hold the bones in place; but in dislocation, after
the bones are replaced in their normal position, the deformity will
not reappear.
Treatment.—The treatment for dislocation consists in bending the
forearm backward to a straight line, or even a little more, and then
while an assistant holds firmly the arm above the elbow, the forearm
should be grasped below the elbow and pulled with great force away
from the assistant and, while exerting this traction, the elbow is
suddenly bent forward to a right angle, when the bones should slip
into place.
The after treatment is much the same as for most fractures of the
elbow. The arm is retained in a well-padded right-angled tin splint
which is applied with three strips of surgeon's plaster and bandage to
the front of the arm and forearm (see Fig. 33) for two or three weeks.
The splint should be removed every few days, and the elbow joint
should be moved to and[Pg 129] fro gently to prevent stiffness, and the
splint then reapplied.
DISLOCATION OF THE HIP.—This occurs more commonly in males from
fifteen to forty-five years of age, and is due to external violence.
In the more ordinary form of hip dislocation the patient stands on the
sound leg with the body bent forward, the injured leg being greatly
shortened, with the toes turned inward so much that the foot of the
injured limb crosses over the instep of the sound foot. The injured
limb cannot be moved outward and but slightly inward, yet may be bent
forward. Walking is impossible. Pain and deformity of the hip joint
are evident.
The only condition with which this would be likely to be confused is a
fracture of bone in the region of the hip. Fracture of the hip is
common in old people, but not in youth or middle adult life. In
fracture there is usually not enough shortening to be perceived with
the eye; the toes are more often turned out, and the patient can often
bear some weight on the limb and even walk.
Treatment.—The simplest treatment is that recommended by Stimson, as
follows: the patient is to be slung up in the air in a vertical
position by means of a sheet or belt of some sort placed around the
body under the armpits, so that the feet dangle a foot or so from the
floor, and then a weight of about ten or fifteen pounds, according to
the strength of the pa[Pg 130]tient's muscles, is attached to the foot of the
injured leg (bricks, flatirons, or stones may be used), and this
weight will usually draw the bone down into its socket within ten or
fifteen minutes.
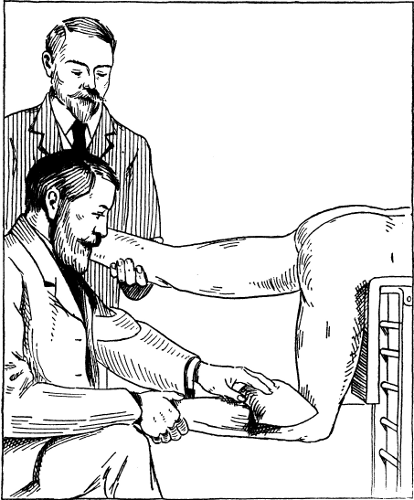 Fig. 34.
Fig. 34.
REDUCING DISLOCATION OF HIP (Reference Handbook).
Patient lying on table; uninjured leg held by assistant; leg of
dislocated side at right angles; note weight at bend of knee.
[Pg 131]Or the patient may assume the position shown in the accompanying cut,
lying prone upon a table with the uninjured leg held horizontally by
one person, while another, with the injured thigh held vertically and
leg at right angles, grasps the patient's ankle and moves it gently
from side to side after placing a five-to ten-pound sand bag, or
similar weight of other substance, at the flexure of the knee. When
the dislocation has been overcome the patient should stay in bed for a
week or two and then go about gradually on crutches for two weeks
longer.
SURGICAL DRESSINGS.—Sterilized gauze is the chief surgical dressing
of the present day. This material is simply cheese cloth, from which
grease and dirt have been removed by boiling in some alkaline
preparation, usually washing soda, and rinsing in pure water. The
gauze is sterilized by subjecting it to moist or dry heat. Sterilized
gauze may be bought at shops dealing in surgeons' supplies and
instruments, and at most drug stores. Gauze or cheese cloth may be
sterilized (to destroy germs) by baking in a slow oven, in tin boxes,
or wrapped in cotton cloth, until it begins to turn brown. It is well
to have a small piece of the gauze in a separate package, which may be
inspected from time to time in order to see how the baking is
progressing, as the material to be employed for surgical purposes
should not be opened until just before it is to be used, any remainder
being immediately covered again. Cut the gauze into pieces as large as
the hand,[Pg 132]
[Pg 133] before it is sterilized, to avoid cutting and handling
afterwards. Gauze may also be sterilized by steaming in an Arnold
sterilizer, such as is used for milk, or by boiling, if it is to be
applied wet. Carbolized, borated, and corrosive-sublimate gauze have
little special value.
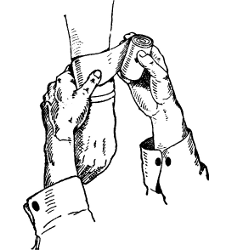 Fig. I.
Fig. I.
|
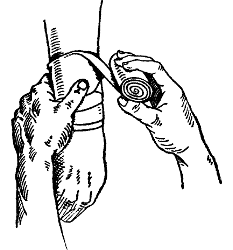 Fig. II.
Fig. II.
|
| |
|
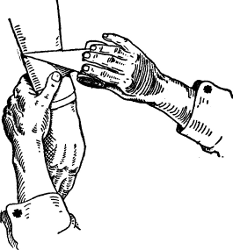 Fig. III.
Fig. III.
|
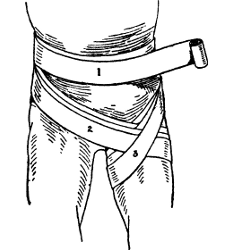 Fig. IV.
Fig. IV.
|
Plate I.
APPLYING A ROLLER BANDAGE (Reference Handbook).
Fig. I shows method of starting a spiral bandage; Fig. II, ready to
reverse; Fig. III, the reverse completed; Fig. IV shows spica bandage
applied to groin.
Absorbent cotton is also employed as a surgical dressing, and should
also be sterilized if it is to be used on raw surfaces. It is not so
useful for dressing wounds as gauze, since it mats down closely, does
not absorb secretions and discharges so well, and sticks to the parts.
When torn into balls as large as an egg and boiled for fifteen minutes
in water, it is useful as sponges for cleaning wounds. Sheet wadding,
or cotton, is serviceable in covering splints before they are applied
to the skin. Wet antiseptic surgical dressings are valuable in
treating wounds which are inflamed and not healing well. They are made
by soaking gauze in solutions of carbolic acid (half a teaspoonful of
the acid to one pint of hot water), and, after application, covering
the gauze with oil silk, rubber dam, or paraffin paper. Heavy brown
wrapping paper, well oiled or greased, will answer the purpose when
better material is not at hand.
BANDAGES.—Bandaging is an art that can only be acquired in any degree
of perfection by practical instruction and experience. Some useful
hints, however, may be given to the inexperienced. Cotton cloth,
bleached or unbleached, is commonly employed for bandages; also gauze,
which does not make so effective a[Pg 134]
[Pg 135] dressing, but is much easier of
application, is softer and more comfortable, and is best adapted to
the use of the novice. A bandage cannot be put on properly unless it
is first rolled. A bandage for the limbs should be about two and a
half inches wide and eight yards long; for the fingers, three-quarters
of an inch wide and three yards long. The bandage may be rolled on
itself till it is as large as the finger, and then rolled down the
front of the thigh, with the palm of the right hand, while the loose
end is held taut in the left hand.
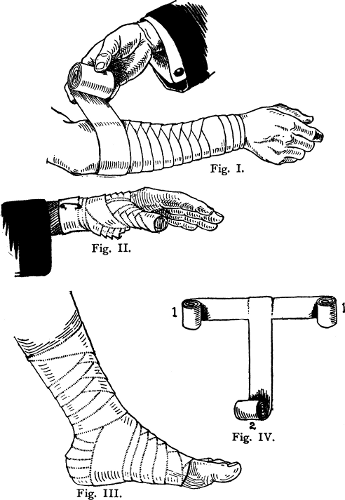
Plate II.
DIFFERENT FORMS OF BANDAGES.
(American Text-Book and Reference Handbook.)
Fig. I shows application of figure-of-eight bandage; Fig. II, a spica
bandage of thumb; Fig. III, a spica bandage of foot; Fig. IV, a
T-bandage.
Two forms of bandages are adapted to the limbs, the figure-of-eight,
and the spiral reversed bandage. In applying a bandage always begin at
the lower extremity of the limb and approach the body. Make a few
circular turns about the limb (see Fig. I, p. 132), then as the limb
enlarges, draw the bandage up spirally, reversing it each time it
encircles the limb, as shown in Fig. I, p. 134. In reversing, hold the
bandage with the left thumb so that it will not slip, and then
allowing the free end to fall slack, turn down as in Fig. II, p. 132.
The T-bandage is used to bandage the crotch between the thighs, or
around the forehead and over the top of the skull. (See Fig. IV, p.
134.) In the former case, the ends 1–1 are put about the body as a
belt, and the end 2 is brought from behind, in the narrow part of the
back, down forward between the thighs, over the crotch, and up to the
belt in the lower part of the belly. The figure-of-eight bandage is
used on various parts, and is illustrated in the bandage called spica
of the[Pg 136]
[Pg 137]
[Pg 138] groin, Fig. IV, p. 132. Beginning with a few circular turns
about the body in the direction of 1, the bandage is brought down in
front of the body and groin, as in 2, and then about the back of the
thigh up around the front of the thigh, as in 3, across the back and
once around the body and down again as in 2. Other bandages
appropriate to various parts of the body are also illustrated that by
their help the proper method of their application may be understood.
See pages 132, 134, 136, 137. The triangular bandage (see p. 88) made
from a large handkerchief or piece of muslin a yard square, cut or
folded diagonally from corner to corner, will be found invaluable in
emergency cases. It is easily and quickly adjusted to almost any part
of the body, and may be used for dressing wounds, or as a bandage for
fractures, etc.
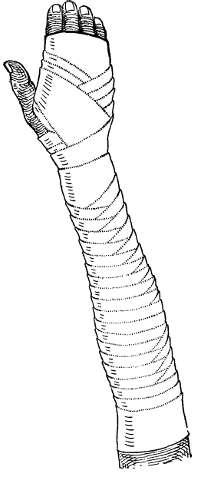 Fig. I.
Fig. I.
|
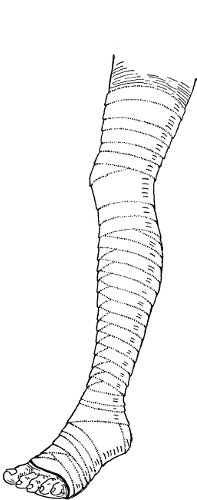 Fig. II.
Fig. II.
|
Plate III.
BANDAGES FOR EXTREMITIES (American Text-Book).
Fig. I shows a spiral reversed bandage of arm and hand, requiring
roller 21/2 inches wide and 7 yards long; Fig. II shows a spiral
reversed bandage of leg and foot, requiring roller 21/2 inches wide and
14 yards long.
 Fig. I.
Fig. I.
|
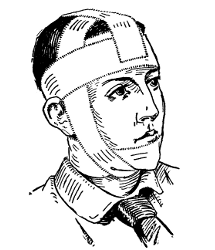 Fig. II.
Fig. II.
|
| |
|
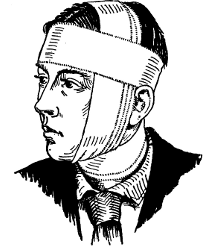 Fig. III.
Fig. III.
|
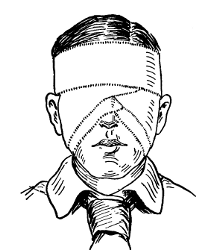 Fig. IV.
Fig. IV.
|
Plate IV.
BANDAGES FOR HEAD AND HAND.
(American Text-Book.)
Fig. I shows a gauntlet bandage; Fig. II, a circular bandage for the
jaw; Fig. III, a circular bandage for the head; Fig. IV, a
figure-of-eight bandage for both eyes.
[Pg 139]
CHAPTER VI
Ordinary Poisons
Unknown Poisons—Antidotes for Poisoning by Acids and Alkalies—The
Stomach Pump—Emetics—Symptoms and Treatment of Metal
Poisoning—Narcotics.
First Aid Rule 1.—Send at once for physician.
Rule 2.—Empty stomach with emetic.
Rule 3.—Give antidote.
In most cases of poisoning emetics and purgatives do the most good.
UNKNOWN POISONS.—Act at once before making inquiry or investigation.
First Aid Rule.—Give two teaspoonfuls of chalk (or whiting, or
whitewash scraped from the wall or a fence) mixed with a wineglass of
water. Beat four eggs in a glass of milk, add a tablespoonful of
whisky, and give at once.
Meanwhile, turn to p. 186, and be prepared to follow Rule 2 under
Suffocation, in case artificial respiration may be necessary, in spite
of the stimulant and antidotes. After having taken the first steps,
try to ascertain the exact poison used, but waste no time[Pg 140] at the
start. If you can find out just what poison was swallowed, give the
treatment advised under that poison, excepting what you may already
have given.
ACIDS.—Symptoms: Corrosion or bleeding of the parts with which they
come in contact, followed by intense pain, and then prostration from
shock. Nitric acid stains face yellow; sulphuric blackens; carbolic
whitens the mucous membrane, and also causes nausea and stupor.
Treatment.—Carbolic: Give a tablespoonful of alcohol or wineglass
of whisky or brandy at once; or one tablespoonful of castor oil, also
a half pint of sweet oil, also a pint of milk. Put to bed, and apply
hot-water bottles.
Nitric and Oxalic: Chalk, lime off walls, whitewash scraped off
fence or wall, one teaspoonful mixed with a quarter of a glass of
water. Give one tablespoonful castor oil, and half a pint of sweet
oil. Inject into the rectum one tablespoonful of whisky in two of
water.
Sulphuric: Soapsuds, half a glass; a pint of milk.
Other Acids: Limewater, or two teaspoonfuls of aromatic spirit of
ammonia diluted with a glass of water. One tablespoonful of castor
oil.
ALKALIES.—Symptoms: Burning and destruction of the mucous membrane of
mouth, severe pain, vomiting and purging of bloody matter, rapid death
by shock.
[Pg 141]Ammonia; Potash; Lye; Caustic Soda; Washing Soda: Give half a glass
of vinegar mixed with half a glass of water; also juice of four lemons
in two glasses of water. One teaspoonful of castor oil in half a glass
of olive oil. If prostrated, give tablespoonful of whisky in a quarter
of a glass of hot water.
METALS.—Symptoms: Great irritation, cramps and purging, suppression
of urine, delirium or stupor, collapse, and generally death.
Arsenic; Paris Green; Fowler's Solution; "Rough on Rats": Intense
pain, thirst, griping in bowels, vomiting and bloody purging, shock,
delirium. Patient picks at the nose. Send to druggist's for two ounces
hydrated sesquioxide of iron, the best antidote, and give
tablespoonful every quarter hour in half a glass of water. Meanwhile,
or if antidote is not to be had, give a glass or two of limewater,
followed by a teaspoonful of mustard dissolved in a glass of water,
followed by warm water in any quantity.
Copper; Blue Vitriol; Verdigris: Give one tablespoonful of mustard
in a glass of warm water. After vomiting, give whites of three eggs,
one pint of milk.
Mercury; Corrosive Sublimate; Bug Poison; White Precipitate;
Bichloride of Mercury: Give whites of four eggs for every grain of
mercury suspected; cause vomiting by giving a tablespoonful of mustard
mixed with a glass of warm water, or thirty grains of powdered ipecac
mixed with half a glass of water.
Silver Nitrate: Give two teaspoonfuls of table salt[Pg 142] dissolved in
two glasses of hot water. After half an hour give a tablespoonful of
castor oil.
Phosphorous; Matches: Give teaspoonful of mustard mixed in a glass
of water. After vomiting has occurred, give a tablespoonful of gum
arabic dissolved in a tumblerful of hot water. An hour later give
tablespoonful of Epsom salts dissolved in a glass of water. Give no
oil.
Antimony; Tartar Emetic: Symptoms as stated for metals. Give thirty
grains of powdered ipecac stirred in wineglass of water, even if
vomiting has occurred. Give three cups of strong tea, or hot infusion
of oak bark, and two teaspoonfuls of whisky in wineglass of hot water.
Use hot-water bottles to keep patient warm.
NARCOTICS.—Aconite; Belladonna; Camphor; Digitalis; Ergot;
Hellebore; Lobelia: These all cause nausea, numbness, stupor,
rapidity of the heart followed by weakness of heart, delirium or
convulsions, coma, and death. There is often an acid taste in mouth,
with dryness of throat and mouth, fever, vomiting and diarrhea, with
severe pain in the bowels. Pupils are dilated.
In either case use the stomach pump at once. If no pump is at hand,
siphon out stomach with rubber tube and funnel. If tube is not
available, give thirty grains of powdered ipecac stirred in a
wineglass of water, followed by two glasses of warm water. As the
patient vomits, give more warm water. When vomit[Pg 143]ing ceases, give two
cups of strong hot coffee, and then a tablespoonful of castor oil.
Keep patient awake by rubbing; do not exhaust him by walking him
about. He must lie flat. If prostration follows, give two teaspoonfuls
of whisky in wineglass of hot water from time to time, if repetition
is necessary.
Alcohol; Liquors Containing It: Symptoms of drunkenness, stupor,
drowsiness, irritability of temper, rapid, weak heart, sleep, coma.
Breath testifies.
If possible, use stomach pump early, or tube and funnel. Or give
thirty grains of powdered ipecac stirred in a wineglass of water, and
when vomiting ceases give thirty drops of aromatic spirit of ammonia
in a wineglass of water every half hour till pulse has become full and
rapid. Then apply cold to the head and heat to the extremities.
Chloral; Patent Sleeping Medicines; "Knock-out Drops." Symptoms:
Nausea, coldness and numbness, stupidity, prostration, often vomiting
and purging, sleep, coma. Heart very weak, with pulse at wrist very
feeble. Constriction of the mouth and throat, with dryness. Pain in
bowels is marked before stupor appears.
Use stomach pump if possible, or empty stomach with rubber tube and
funnel, siphoning fluids out. Or give thirty grains of powdered ipecac
stirred in a wineglass of water. When vomiting ceases, give two
teaspoonfuls of whisky in half a glass of hot water. Give[Pg 144] hypodermic
injection of sulphate of strychnine, one-twentieth of a grain every
two or three hours, till patient is roused and weakness is past.
Rubbing of the surface, application of hot-water bottles to the body
and legs.
If breathing ceases, follow Rule 2 under Suffocation (p. 186) till
breathing is well established again.
Opium; Morphine; Laudanum; Paregoric; Soothing Syrups. Symptoms:
Drowsiness, sleep, stupor when roused, pupils very small—"pin point"
unless patient is used to the drug—constipation, cold skin.
Use stomach pump, if at hand. Or give emetic of thirty grains of
powdered ipecac stirred in a wineglass of water, followed by two
glasses of warm water, as vomiting proceeds. Let the patient inhale
ammonia or smelling salts. Give him half a grain of permanganate of
potash dissolved in a wineglass of water, every half hour. Inject two
ounces of black coffee, at blood heat, into the rectum.
Rub the lower part of the body and legs briskly toward the heart,
while artificial respiration is being carried out. See Rule 2 under
Suffocation (p. 186). Thirty drops of tincture of belladonna to an
adult, every hour, will assist the breathing. Do not exhaust the
patient by walking him around, slapping him with wet towels, or
striking him on the calves; keep him awake by rubbing.
Tobacco when Swallowed: Nausea and vomiting occur, with severe pain
and great prostration; de[Pg 145]lirium or convulsions may follow. The heart,
at first rapid and full, becomes weak and compressible.
Give emetic at once: thirty grains of powdered ipecac stirred in
wineglass of water, followed by two glasses of warm water, by degrees.
Give whisky, two teaspoonfuls in wineglass of hot water. Keep patient
warm.
Nux Vomica; Strychnine. Symptoms: Excitement, rapid heart action,
restlessness, panic of apprehension, twitching of forearms and hands,
possibly convulsions, during consciousness.
Use stomach pump, if possible, or give thirty grains of powdered
ipecac stirred in a wineglass of water. Then, when vomiting has
ceased, give twenty grains of chloral, together with thirty grains of
bromide of sodium in half a glass of water, at blood heat, injected
into the rectum. Give twenty grains of bromide of sodium in a
wineglass of water, every hour, by the mouth.
If convulsions, put chloroform before nose and mouth, as follows: pour
twenty drops of chloroform on a handkerchief and hold it close to the
mouth, letting air pass freely under it. Stop when patient relaxes.
Resume if he becomes rigid again.
Cocaine. Symptoms: General nervousness, irritability of temper,
wakefulness, followed quickly by great pallor, dilatation of the
pupils, unconsciousness, and convulsions.
Give the patient two teaspoonfuls of whisky in a[Pg 146] wineglass of water
every hour. Give, if possible, a hypodermic of a thirtieth of a grain
of strychnine, every two hours, or as he may require it, to keep the
pulse full and strong. Use hot-water bottles to feet and legs.
Phenacetin; Acetanilid; Headache Powders: Give two teaspoonfuls of
whisky in a wineglass of hot water. If the heart flags, give tincture
of digitalis, five minims in tablespoonful of water, every two hours,
or till three doses are given. It is better to use digitalin, one
one-hundredth of a grain hypodermically, if possible.
[Pg 147]
CHAPTER VII
Food Poisoning
Food Containing Bacterial Poisons Resulting from Putrefaction; Food
Infected with Disease Germs; Food Containing
Parasites—Tapeworm—Trichiniasis—Potato Poisoning.
FOOD POISONING.—Much the same symptoms from all meats, fish,
shellfish, milk, cheese, ice cream, and vegetables; namely, vomiting,
cramps, diarrhea, headache, prostration, weak pulse, cold hands and
feet, possibly an eruption.
First Aid Rule 1.—Rid patient of poison. Cause repeated vomiting by
giving three or four glasses of warm water, each containing half a
level teaspoonful of mustard. Put finger down throat to assist. Empty
bowels by giving warm injection of soapsuds and water by fountain
syringe.
Rule 2.—Support heart and rally nerve force. Give teaspoonful of
whisky in tablespoonful of hot water every half hour, as needed. Put
hot-water bottles at feet and about body.
Conditions, Etc.—Bacterial poisons, constituting irritants of the
stomach and bowels, are found in[Pg 148] certain mussels, oysters from
artificial beds, eels out of stagnant ditches—as well as the uncooked
blood of the common river eel—certain fish at all times, certain fish
when spawning, putrefied fish, fermented canned fish, sausages of
which the ingredients have putrefied, putrefied meat, imperfectly
cured bacon, putrefied cheese, milk improperly handled and not cooled
before being transported, ice cream which fermented before freezing,
or ice cream containing putrid gelatin, and mouldy corn meal and the
bread made from it.
These poisons are called toxins, or toxalbumins, or bacterial
proteids. They are no longer called ptomaines, because many ptomaines
are not poisonous. They are formed within the cells of the bacteria,
and result from the combination of certain constituents of the food
material that nourishes the bacteria, in some way not quite
understood. Some decomposition must have taken place in the food
before it can furnish to the bacteria the nourishment it needs. If
this has happened, the bacteria multiply rapidly, and the toxins that
are formed are taken up by the lymphatics and carried away from the
tissues as fast as possible. But so great is their virulence that they
act on several vital organs before they can be antagonized by the
natural elements of the blood.
Symptoms.—The symptoms are much the same in all the cases of
bacterial poisoning mentioned. Sudden and violent vomiting and
diarrhea appear a few hours after eating the spoiled food, or may be
delayed.[Pg 149] There may be headache, colic, and cramps in the muscles.
Marked prostration and weak pulse with cold hands and feet are
characteristic. The appearance of skin eruptions is not uncommon. The
occurrence of such symptoms in several persons, some hours after
partaking of the same food, is sufficient to warrant one in
pronouncing the trouble food poisoning.
Treatment.—The objects of treatment are to rid the patient of the
poison, and to stimulate the heart and general circulation, and draw
on the reserve nerve force. It is best to procure medical aid to wash
out the stomach, but when this is impossible, the patient should be
encouraged to swallow plenty of tepid water and then vomit it. If
there is no natural inclination to do so, vomiting may be brought
about by putting the finger in the back of the throat. The same
process should be repeated a number of times, and the result will be
almost as good as though a physician had used a stomach tube. A
teaspoonful of salt or tablespoonful of mustard in the water will
hasten its rejection. Then the bowels should likewise be emptied. If
vomiting continues this will not be possible by means of drugs given
by the mouth, although calomel may be retained given in half-grain
tablets hourly to an adult, until the bowels begin to move, or till
eight to ten tablets are taken. When vomiting is excessive, emptying
of the bowels may be brought about quickly by giving warm injections
of soapsuds into the bowel with a fountain syringe. Brandy or whisky
in tea[Pg 150]spoonful doses given in a tablespoonful of hot water at
half-hour intervals should follow the emptying of the stomach and
bowels, and the patient must be kept quiet. He must also be kept warm
by means of hot-water bags and blankets.
INFECTED FOOD.—A frequent source of illness is infection by disease
germs transmitted in food. The meat of animals slaughtered when sick
with abscess, pneumonia, kidney disease, diarrhea, or anthrax
(malignant pustule) carries disease germs and causes serious illness;
so does the meat of animals killed after recent birth of their young,
and probably having fever. Oysters may be contaminated with excrement
from typhoid patients, and may then transmit the disease to those who
eat them.
Milk from diseased animals, or contaminated with germs of typhoid
fever, scarlet fever, tuberculosis, diphtheria, etc., is apt to cause
the same disease in the human being who drinks it.
If such infected food is eaten raw, the diseases with which it is
contaminated may be transmitted. If subjected to cooking at a
temperature of at least the boiling point, comparative safety is
secured; but the toxins accompanying the disease germs in the infected
food are not as a rule rendered harmless. Treatment must be directed
to each disease thus transmitted.
Poisoning resulting from eating canned meats has sometimes been
attributed to supposed traces of tin, zinc, or solder, which have
become dissolved in the[Pg 151] fluids of the meat, but in the vast majority
of cases such poisoning is due to toxins accompanying the germs of
putrefaction, the meats having been unfit for canning at the outset.
In such cases the symptoms are the same as in other food poisoning,
and the treatment must be such as is elsewhere directed (see pp. 147
and 149).
While human breast milk is germ free, the cows' milk sold in cities is
a very common source of disease. Scrupulous care of the cows, of the
clothing and hands of the milkers, of the stables at which the herds
are quartered, and of the cans, pails, and pans used, reduces to a
minimum the amount of filth and impurity otherwise mixed with milk. In
the household, as well as during transportation, milk should be kept
cool, with ice if necessary. It should also never be left uncovered,
for it readily absorbs gases, effluvia, and contaminating substances
in the air, and affords an excellent medium for the growth and
propagation of germs. When partially or entirely soured, it should not
be used, except in the preparation of articles of food by cooking, as
directed in cook books. It should never be used if there is any doubt
about its purity. Unless all doubt has been removed, it is best to
subject milk intended for children's consumption to a temperature of
160° F. for ten minutes, and then put it on the ice, especially during
hot weather. Germs are thus rendered harmless, and the nourishing
qualities of the milk remain unimpaired.
[Pg 152]Summer diarrhea of children, also called cholera infantum, occurs as
an epidemic in almost all large cities during the hottest days of
summer. The disease is largely fatal, especially during the first hot
month, because the most susceptible and tender children are the first
affected. It is due to the absorption into the systems of these
children of the toxins formed during the putrefying of milk in the
stomachs and bowels of the little sufferers. Clean, pure sweet milk,
free from bacteria should be used to prevent the occurrence of this
disease. Its treatment is outlined in Vol. III. Exactly what bacteria
cause the disease is not decided. Possibly the milk is infected, but
probably the poisonous results come from toxins.
FOOD CONTAINING PARASITES.—The parasites found in food in this
country are echinococcus, guineaworm, hookworm, trichina, and
tapeworm. Echinococcus cannot be understood or diagnosed by the
layman. Guineaworm is excessively rare in the United States; it gains
access into the body through drinking water which contains the
individuals. Hookworm is the cause of "miners' anæmia," and is
extremely rare in this country.
The entrance of living food parasites can be absolutely prevented by
thorough cooking of meats, especially pork and beef. Heat destroys the
"measles" and the trichina worms.
TAPEWORM.—This is developed in man after eating "measly" beef or
pork. "Measles" are em[Pg 153]bryo tapeworms called, from their appearance,
"bladder worms." In from six to ten weeks after being received into
the intestine of a man, these bladder worms become full grown, and
measure from ten to thirty feet in length—the tapeworms.
Symptoms.—Vertigo, impairment of sight and of hearing, itching of the
nose, salivation, loss of appetite, dyspepsia, emaciation, colic,
palpitation of the heart, and sometimes fainting accompany the
presence of the tapeworm. Generally the condition becomes known
through the passage in the excrement of small sections of the worm.
These sections resemble flat portions of macaroni.
Treatment.—This, to be successful, must be directed by a physician.
When no physician can be procured, the patient may attempt his own
relief. After fasting for twenty-four hours, pumpkin seed, from which
the outer coverings have been removed by crushing, are soaked
overnight in water and taken on an empty stomach in the morning; a
child takes one or two ounces thoroughly mashed and mixed with sirup
or honey, and an adult four ounces (see Vol. III, p. 245).
TRICHINIASIS.—This is a dangerous disease caused by the presence in
the muscles and other tissues of the trichinæ, little worms which are
swallowed in raw or partly cooked pork, ham, or bacon. Nausea,
vomiting, colic, and diarrhea appear early, generally on the second
day after eating the infected meat. Later, stiffness of the muscles
occurs, with great ten[Pg 154]derness, swelling of the face and of the
extremities, sweating, hoarseness, difficult breathing, inability to
sleep, bronchitis, and pneumonia.
There is no treatment for the disease. Many cases which are not fatal
are probably considered to be obscure rheumatism. Many cases of
pneumonia are caused by the worm.
POTATO POISONING.—There remains one variety of food poisoning which
needs mention, since it occurs when least expected, and when proper
food has been subjected to natural growth. As the potato belongs to
the botanical family containing the dangerous belladonna, tobacco,
hyoscyamus, and stramonium, it is not surprising that is should also
contain a powerful poisonous alkaloid, namely, solanine. Solanine is
developed in potatoes, especially during their sprouting stage.
Violent vomiting and diarrhea and inflammation of the stomach and
bowels are caused by it. Careful peeling of sprouting potatoes, and
removal of their eyes, will lessen, if not wholly obviate, the danger
from eating them. This form of food poisoning is rare.
[Pg 155]
CHAPTER VIII
Bites and Stings
Several Kinds of Mosquitoes—Cause of Yellow Fever—Bee, Wasp, and
Hornet Stings—Wood Ticks, Lice, and Fleas—Scorpions and
Centipedes—Poisonous Snakes—Dog and Cat Bites.
MOSQUITOES.—The female mosquito is the offender. During or after
sucking blood she injects a poison into the body which causes itching,
swelling, and, in some susceptible persons, considerable inflammation
of the skin. The bites of the mosquitoes living on the shores of the
Arctic Ocean and in the tropics are the most virulent. The most
important relation of mosquitoes to man was only recently discovered.
They are probably the sole cause of malaria and yellow fever in the
human being. The malarial parasite which lives in the blood of man,
when he is suffering from malaria, first inhabits the body of a
certain kind of mosquito. The mosquito acquires the undeveloped
parasite by biting the human malarial patient, and then acts as a
medium of infection by transmitting the active parasite to some
healthy man, through the bite.
The more common house mosquito, the Culex, does not carry the parasite
of malaria, and it is important to be able to distinguish the
Anopheles which is the source of malaria. The Anopheles is more common
in[Pg 156] the country, while the Culex is a city pest. The Culex has very
short palpi, the name given to the projections parallel to the
proboscis; while those of Anopheles are so large that it appears to
have three probosces. There are no markings on the wings of the
ordinary species of Culex, while the wings of Anopheles are distinctly
mottled. The Culex, sitting on a wall or ceiling, holds its hind legs
above its back and its body nearly parallel to the wall or ceiling,
but the Anopheles carries its hind legs either against the wall or
hanging down (rarely above the back), and its body, instead of lying
parallel to the wall or ceiling, hangs away at an angle of about
forty-five degrees from it.
The Culex lays her eggs in sinks, tanks, cisterns, and water about
houses, but the Anopheles deposits her ova in shallow pools and
sluggish streams, especially those on which is a growth of green scum
or algæ. Such are the main distinguishing features of the
malaria-carrying mosquito, the Anopheles, and the commoner house
variety, the Culex.
To prevent malaria, mosquito bites must be prevented by nettings in
houses, especially for the protection of sleepers. Pools, ponds, and
marshy districts must be drained in order to destroy the breeding
places of Anopheles, and in the malarial season, petroleum (kerosene)
must be poured on the surface of such waters to arrest the development
of the immature insects (larvæ).
The mosquito is believed to be the sole cause of[Pg 157] yellow fever, being
capable of communicating the germ of the disease to man by its bite
two weeks after it has itself been contaminated with the germ in
feeding on the blood of a yellow-fever patient. This invaluable
discovery was made by Dr. Walter Reed, U. S. A., in 1901, as a result
of his labors and those of other members of the yellow-fever
commission of the U. S. Army in Cuba, involving the death of one of
the members of the commission (Dr. Lazear), and utilizing the heroism
of a number of our young soldiers who voluntarily offered themselves
to be bitten by mosquitoes that had previously bitten yellow-fever
patients, and who experimentally occupied premises containing all
sorts of articles infected by yellow-fever patients. The result of
their research proves that yellow fever is not contagious at all, in
the usual sense, but is communicated only through the medium of
mosquitoes. This shows the fallacy of many quarantine rules regarding
yellow-fever patients, and of the fear of nursing the sick, and will
result in controlling the disease.
In the case of malaria or yellow fever, there is a vicious circle into
which man and the mosquito enter; malaria and yellow-fever patients
contaminate the mosquitoes which bite them, and the mosquitoes in
their turn infect man with these diseases. A patient with malaria
coming into a nonmalarial place, and being bitten by mosquitoes, may
lead to an epidemic of the disorder which becomes endemic. To
terminate this condition, it is necessary to prevent the contact of
man[Pg 158] with mosquitoes and to kill these insects. Both malaria and
yellow fever will doubtless be practically eradicated before long
through the result of these scientific discoveries.
Treatment of Mosquito Bites.—To prevent mosquitoes, fleas, lice,
horseflies, etc., from biting, it is necessary merely to dip the clean
hands into a pail of water in which, while hot, one ounce of pure
carbolic acid was dissolved, and while they are thus wet rub the
solution over all the exposed skin and allow it to dry naturally. A
mixture of kerosene (petroleum) and water used in the same way will
also afford protection. All poisons introduced into the body by
insects are of an acid nature, and to this quality are due the pain
and irritation which it is our object to overcome. The best remedy,
naturally, is an alkali of some sort. Water of ammonia, diluted, or a
strong solution of saleratus or baking soda in water, are the two most
successful remedies to apply, either through bathing, or on cloths
saturated in one of the solutions. Clean clay, mixed with water to
make a mud poultice, is a useful application in emergencies.
BEE, WASP, AND HORNET STINGS.—The pain and swelling are produced by
the poison of the insect which leaves the poison bag at the base of
the barb at the instant that the person is stung. The bee stings but
once, as the sting being barbed is broken off, and is retained in the
flesh of the victim. The sting of the wasp and hornet is merely
pointed, and is not[Pg 159] lost during the stinging process so that they can
repeat the act. Bee keepers, after being stung a number of times,
usually become immune, i. e., they are no longer poisoned by bites of
these insects.
It is well to extract the sting of bees before all of the poison has
come away. A fine pair of forceps is useful for this purpose; or, by
pressing the hollow tube of a small key directly down over the
puncture made by the sting, it may be squeezed out.
Ammonia water, as recommended for mosquitoes, is the best remedy to
relieve the pain.
WOOD TICKS.—Ticks inhabit the woods and bushes throughout the
temperate zone, and at certain periods during the summer season attack
passing men and animals.
The common tick is nearly circular in shape, very flat, with a dark,
brown, horny body about one-sixteenth to one-eighth inch in diameter.
Each of its eight legs possesses two claws, and the proboscis incloses
feelers which are similarly armed. The beetle plunges its barbed
proboscis into the flesh of man or animals, and holds on very firmly
with its other members till it is gorged with blood, growing as large
as a good-sized bean, when it drops off. The bite is painless, and it
is not until the insect is engorged with blood that it is perceptible;
if, however, attempts are made to remove the tick before it is ready
to let go, the proboscis may be torn off and left in the skin, when
painful local suppuration will follow.
[Pg 160]Treatment.—As the presence of tick is far from agreeable, the insect
may often be removed by painting it with turpentine, which either
kills it or causes the claws to be relaxed; in either case the tick
loosens its hold and drops to the ground. A tropical variety,
carapato, buries the whole head in the flesh of its host before it is
perceived, and if turpentine does not loosen its hold, the head must
be dug out with a clean needle or knife blade.
LICE (Pediculi).—Head lice are most common. They are gray with
black margins, about one-twenty-fifth to one-twelfth inch long, and
wingless. The color changes with the host, as the lice are black on
the negro, and white in the case of the Eskimos. The female lays fifty
to sixty eggs ("nits"), seen as minute, white specks glued to the side
of a hair; usually not more than one or two on a single hair. The eggs
hatch in six days.
The irritation produced by the presence of the parasites on the head
leads to general itching, more particularly on the lower part of the
back of the head. The constant scratching starts an inflammation of
the skin with the formation of pimples, weeping spots, and crusts,
from the dried discharge, possessing a bad odor. The denuded spots
becoming infected, the neighboring glands enlarge and are felt as
tender lumps beneath the skin at the back of the neck, under the jaw,
or at either side of the neck. Whenever there are persistent itching
and irritation of the scalp, particularly at the[Pg 161] back of the head,
lice or "nits" should be sought for. Sometimes it is more easy to find
them on a fine-tooth comb passed through the hair. Lice are very
common in dirty households, and are occasionally seen on the most
fastidious persons, who accidentally acquire them in public places or
conveyances.
Treatment.—The hair should be cut short when permissible. Any crusts
on the head should be softened by the application of sweet oil, and
then removed by washing in soap and warm water. Petroleum or kerosene
is a good remedy. It must be rubbed on the head two successive nights,
the head being covered by a cap, and washed off each morning with hot
water and soap. The patient must be cautioned not to approach an open
flame after kerosene has been put on his head.
The eggs or "nits" are next to be attacked with vinegar, which is
sponged on the hair and the fine-tooth comb plied daily for a week.
The remaining irritation of the scalp can be cured by washing the head
daily and applying sweet oil.
A simpler plan consists of drenching hair and scalp twice with cold
infusion of (poisonous) larkspur seed, made by steeping for an hour an
ounce of the seed in six ounces of hot water.
This treatment will destroy both insects and eggs. After twenty-four
hours the hair and scalp must be shampooed with warm water thoroughly.
CLOTHES LICE.—These insects are a trifle larger than the head lice,
being one-twelfth to one-[Pg 162]eighth inch long, of a dirty, yellowish-gray
color, and only infesting the most filthy people. The lice are
generally only seen on the clothes, where they live, coming out on the
body only to feed. The visible signs on the body are varying degrees
of irritation from redness to ulceration, due to scratching. The
treatment is simply cleanliness of the body and clothes.
CRAB LICE.—The crab louse or "crab" inhabits the skin covered by hair
about and above the sexual organs most frequently, and from thence
spreads to the hairy region on the abdomen, chest, armpits, beard, and
eye lashes. Itching and scratching first call attention to the
presence of the parasites, which are even more troublesome than the
other species.
Application of kerosene to the part is sufficient to kill the lice,
but this treatment must be repeated several times at intervals of a
week, in order to kill the parasites subsequently hatched.
FLEA.—Flea bites are recognized by the itching caused by the poison
introduced by the insect, and by points of dried blood surrounded for
a little while by a red zone. In the case of children and people with
delicate skins, red or white lumps appear resembling nettlerash.
Generally the skin is simply covered with minute, red points, perhaps
raised a little by swelling above the surface, and when very numerous
may remotely resemble the rash of measles. Fleas, unlike lice, do not
breed on the body, but as soon as they are satiated leave their host.
Their eggs are laid in cracks[Pg 163] in floors, on dirty clothes and similar
spots, and it is only the mature flea which preys upon man. The human
flea may infest the dog and return to man, but the dog flea is a
distinct species, and never remains permanently on the human host. For
these reasons it is not difficult to get rid of fleas after they have
attacked the body, unless continually surrounded by them.
JIGGER OR SAND FLEA.—Also called chique, chigo, and nigua. It is
common in Cuba, Porto Rico, and Brazil. About one-half the size of the
ordinary flea, it is of a brownish-red color with a white spot on the
back. The female lives in the sand and attacks man, on whom she lives,
boring into the skin about the toe nail, usually, and laying her eggs
under the skin, which gives rise to itching at first and then violent
pain. The insect sucks blood and grows as it gorges itself, producing
a white swelling of the skin in the center of which is seen a black
spot, the front part of the flea. The flea after expelling its eggs
drops off and dies. People with habitually sweaty feet are exempt from
attacks of the pest.
Unless the flea is unattached, one must either wait until the insect
comes away of its own free will, or remove it with a red-hot needle in
order to destroy the eggs. The negroes peel the skin from the swelling
with a needle and squeeze out the eggs. Ordinarily the bites do no
permanent injury, but occasionally if numerous, or if the insect is
pressed into the skin in[Pg 164] the efforts to remove it, or if sores
resulting from bites are neglected, then violent inflammation, great
pain, and even death of the part may result. Sound shoes and a night
and morning inspection of the feet will protect against the inroads of
the sand fleas.
FLIES.—The common housefly does not bite, but is constantly inimical
to human health by conveying disease germs of typhoid fever, cholera,
and other disorders from bowel discharges of patients suffering from
these diseases to articles of food on which the insects light. Flies
have been a fruitful source of sickness in military camps, as
evidenced in the recent Spanish-American and Anglo-African campaigns.
The bites of the sandfly, gadfly, and horsefly may be both relieved
and prevented by the same means recommended in the case of mosquitoes
for these purposes.
SCORPION OR CENTIPEDE STING.
First Aid Rule.—Squeeze lemon juice on wound.
SPIDER OR TARANTULA BITE.
First Aid Rule.—Pour water of ammonia on bite. If patient is
depressed, give strong coffee.
SCORPIONS AND CENTIPEDES.—These both inhabit the tropics and
semitropical regions, and lurk in dark corners and out-of-the-way
places, crawling into the boots and clothing during the night.
Scorpions sting with their tails, which are brought over the[Pg 165] head and
back for the purpose, while holding on to the victim with their
lobsterlike claws. The poisonous centipede has a flattened
brownish-yellow body, with a single pair of short legs for each body
segment, and long, many-jointed antennæ.
The wounds made by either of these pests are rarely dangerous, except
in young children and those in feeble health. The stings are usually
relieved by bathing with a two per cent solution of carbolic acid,
with rum, or with lemon juice.
SPIDERS.—Many of the tropical spiders bite the human being. Trapdoor
spiders are among the commonest of these pests. Their bodies grow to
great size, two to two and a half inches long, and are covered with
hair giving them a horrid appearance. They live in holes bored in the
ground, and provided with a trapdoor contrivance which is closed when
the insect is at home.
The trapdoor spider resembles the tarantula, by which name it is
usually known in Cuba and Jamaica, but is somewhat smaller and
commoner. Neither the stings of the trapdoor spider nor true tarantula
are usually dangerous although the wounds caused by the bites may heal
slowly.
Application of water of ammonia and of the other remedies recommended
for mosquito bites (p. 158) are indicated here, and if the patient is
generally depressed by the poison, strong coffee forms a good
antidote.
[Pg 166]SNAKE BITE.
First Aid Rule 1.—Make the wound bleed. Cut slit through the wound,
lengthwise of limb, two inches long and half an inch deep. Squeeze
tissues. Do not suck the wound.
Rule 2.—Keep poison out of general circulation. Tie large cord or
bandage tightly about part between wound and heart. Loosen in fifteen
minutes.
Rule 3.—Use antidote. Wash wound and cut with fresh solution of
chloride of lime (one part to sixty parts of water). Inject
anti-venene with hypodermic syringe, ten cubic centimeters, as on
label. Or, inject with hypodermic syringe thirty minims of solution of
permanganate of potash (five grains to two ounces of water), three
times in different places. If no syringe at hand, pour permanganate
solution into wound.
Rule 4.—Support heart if weak. Inject with hypodermic syringe
one-thirtieth grain of sulphate of strychnine into leg. Repeat as
needed every thirty minutes with caution.
Rule 5.—Give no whisky or other liquor. Do not burn the wound.
SNAKE BITE.—There are many different species of poisonous snakes in
the United States. The more common are the rattlesnake, the moccasin,
the copperhead, and the common viper.
All the venomous snakes have certain characteristics by which they may
be distinguished from their[Pg 167] harmless brethren. The head is generally
broad and flat and of a triangular shape, the wide, heavy jaws
tapering to a point at the lips. There is a depression or pit between
the nostril and eye on the upper lip, hence the name "pit vipers"
given to poisonous snakes. The pupil of the eye is long and vertical,
of an oval or elliptical shape.
Venomous snakes are thicker in proportion to their length than
harmless snakes, the surface of their bodies is rougher, and their
tails are blunt or club-shaped. Conversely, harmless snakes possess
long narrow heads, the pupils of their eyes are round, not vertical
slits, and their bodies are not thick for their length, but long and
slim with pointed tails. The bite of vipers of all kinds is much more
poisonous in tropical regions, and in the North fatal snake bite is a
rare occurrence.
If there is a doubt whether a snake is poisonous, the neck may be
pressed down against the ground between the jaws of a forked stick,
and the poison fangs looked for without danger. These hang directly
down from the front part of the upper jaw, or are thrust horizontally
forward just in front of the upper lip, and may drip saliva and venom.
In Cuba and Porto Rico there is a viper called Juba, or Boaquira,
which is a counterpart of the Northern rattlesnake, and the most
poisonous of the many species in that region. Among venomous species
of the Philippines are two boas and also a viper from nine to ten feet
long, which exceptionally pursues and attacks[Pg 168] man. This snake is
easily killed by a blow on the neck. Another small viper with a
club-shaped tail, inhabiting these islands, is nocturnal in its
habits, and may get into boots at night. Boots, therefore, should
always be inspected before one puts them on in the morning.
Usually it is only the young, old, and weak who succumb to snake bite.
Symptoms.—The symptoms of snake bite of all poisonous species are
similar. At first there is some pain in the wound, which rapidly
increases together with swelling and discoloration until death of the
part may ensue. The vital centers in the brain controlling the heart
and breathing apparatus, are paralyzed by the poison. There is often
drowsiness and stupor, and the breathing is labored and the pulse weak
and irregular, with faintness and cold sweats.
Treatment.—The treatment consists first in keeping the poison out of
the general blood stream. With this purpose in view a handkerchief,
piece of cotton clothing, string, or strap should be immediately wound
about the bitten limb above the wound, between it and the heart. This
will retard absorption of the poison only for a time; it is said
twenty-five minutes. The knife is the most effective means of removing
the poison by making an oval cut on each side of the wound so that the
two incisions meet and remove all the flesh below and around the
wound. Bleeding should be encouraged to drain out the poison. The skin
containing the wound may be lifted up, and[Pg 169] the whole wound cut out by
one snip of the scissors where this is practicable.
Some advocate burning out the wound with a red-hot wire, or darning
needle, instead of cutting, but the treatment is less effective and
more painful. Rambaud forbids burning. As to the general condition: if
stupor is a prominent symptom the patient must be made to move about
and exercise to keep alive his nerve centers. Otherwise one
tablespoonful of whisky may be given in half a cup of hot water
hourly, to sustain the weakened heart and respiration until recovery
ensues.
The most effective treatment, according to Dr. George Rambaud,
Director of the Pasteur Institute of New York City, is thorough
washing of the wound (after it has been opened with the knife) with
freshly prepared solution of chloride of lime, in the proportion of
one part of lime to sixty of water. The burning of a wound is bad
practice. If necessary, chloride-of-lime solution should be injected
into the tissues around the wound. One about to go into a place where
the most venomous snakes are found should inject into himself a dose
of Calmette's antivenomous serum every two or three weeks as a means
of prevention. If the serum is used, whisky should not be given in the
treatment of one who has been bitten, for the anti-venene is a
powerful cell stimulator.
Calmette, the Director of the Pasteur Institute in Lille, France,
several years ago discovered antivenomous serum. That serum is
efficient for the bites[Pg 170] of most of the venomous snakes of different
countries, including the rattlesnake, cobra, python, etc.
It is prepared in the dry form so that it can be carried easily, and
will keep almost indefinitely. The proper course to be followed by
persons going into countries infested by venomous snakes is always to
have on hand a few doses of it. Its value has been positively
demonstrated within the last few years in India, where it is used in
the British Army, as well as in other countries.
In the fluid form it should be used hypodermically, a dose of ten
cubic centimeters being injected within eighty or ninety minutes of
the reception of the poison.
DOG BITE OR CAT BITE. (See Hydrophobia, Vol. V, p. 264.)
First Aid Rule 1.—Make sure animal is mad. Send patient to Pasteur
institute if one is within reach.
Rule 2.—Remove poison from wound. Encourage bleeding by squeezing
tissue about wound. Suck wound, if you have no cracks in lips, and
spit out fluid. Pour hot carbolic solution into wound (a third of a
teaspoonful of carbolic acid to a pint of hot water).
Rule 3.—Cauterize. Dip wooden meat skewer, or lead pencil, into pure
nitric acid, and rub into wound. Or, use red-hot poker, or red-hot
nail grasped by tongs or pincers, or red coal from fire.
Rule 4.—Do not kill the animal. If he is alive and well at the end
of a week, he was not mad.
[Pg 171]
CHAPTER IX
Burns, Scalds, Frostbites, Etc.
Classes of Burns—Treatment—Burns Caused by Acids and
Alkalies—First Aid Rules for Frostbites—Real Freezing—Ingrowing Toe
Nail—Fainting—Suffocation—Fits.
BURNS AND SCALDS.—If slight, skin very red, unbroken.
First Aid Rule.—Cover with cloths wet in strong solution of baking
soda in cold water. Dry gently, and spread with white of egg, thick.
If deeper, blisters, skin broken, thick swelling; there may be some
bleeding.
First Aid Rule 1.—Stop pain quickly. Cut away clothing very gently.
Break no blisters. Cover with Carron oil (equal parts of limewater and
linseed or olive oil) and light bandage. Give fifteen drops of
laudanum[9] every half hour in tablespoonful of water, till relieved
in part or three doses are taken.
Rule 2.—Combat shock. If patient is cold, pulse weak, head confused,
give tablespoonful of whisky in a quarter of a glass of hot water. Put
hot-water bottles at feet.
[Pg 172]Rule 3.—Quench thirst with pieces of ice held in mouth or a swallow
of cold milk.
See page 174 for subsequent treatment.
A burn is produced by dry heat, a scald by moist heat; the effect and
treatment of both are practically identical. Burns are commonly
divided into three classes, according to the amount of damage
inflicted upon the body.
First Class.—There is redness, pain, and some swelling of the skin,
followed, in a few days, by peeling of the surface layer (epidermis)
and recovery. Sunburn and burns caused by slight exposures to gases
and vapors fall into this category.
Treatment.—The immediate immersion of the part in cold water is
followed by relief, or the application of cloths wet with a saturated
solution of saleratus or baking powder is useful. Anything which
protects the burned skin from the irritating effect of the air is
efficacious, and in emergencies any one of the following may be
applied: starch, flour, molasses, white paint, or a mixture of white
of egg and sweet oil, equal parts. Usually after the first pain has
been relieved by bathing with soda and water, or its application on
cloths, the employment of a simple ointment suffices, as cold cream or
vaseline.
Second Class.—In this class of cases the inflammation is more
severe and the deeper layers of the skin are involved. In addition to
the redness and swelling[Pg 173] of the skin there are present blisters which
appear at once or within a few hours. The general condition is
affected according to the size of the burn. If half of the body is
only reddened, death usually results, and a burn of a third of the
body is often fatal. The shock is so great at times that pain may not
be at once intense. Shock is evidenced by general depression, with
weakness, apathy, cold feet and hands, and failure of the pulse. If
the patient rallies from this condition, then fever and pain become
prominent. If steam has been inhaled, there may be sudden death from
swelling of the interior of the throat, or inflammation of the lungs
may follow inhalation of smoke and hot air.
Third Class.—In this class are included burns of so severe a nature
that destruction and death of the tissues follows; not only of the
skin but of the flesh and bones in the worst cases. It is impossible
to tell by the appearance of the skin what the extent of the
destruction may be until the dead parts slough away after a week or
ten days. The skin is of a uniform white color in some cases, or may
be of a yellow, brown, gray, or black hue, and is comparatively
insensitive at first. Pus ("matter") begins to form around the dead
part in a few days, and the dead tissue comes away later, to be
followed by a long course of suppuration, pain, excessive granulations
("proud flesh"), and, unless skillfully treated, by contraction of the
surrounding area, leaving ugly scars and interfering with[Pg 174] the
appearance and usefulness of the parts. The treatment of such cases
after the first care becomes that to be pursued in wounds generally
(p. 50), and belongs within the domain of the surgeon.
Treatment of the More Severe Burns.—If the patient is suffering from
shock he should receive some hot alcoholic drink, as hot water and
whisky, and be put to bed under warm coverings with hot-water bags or
bottles at his feet.
The clothing must be cut away from the burned parts with the greatest
care, and only a portion of the body should be uncovered at a time and
in a warm room. Pain may be subdued by laudanum[10]; fifteen drops may
be given to an adult, and the drug may be repeated at hour intervals
in doses of ten drops until the suffering has been allayed. Lumps of
ice held in the mouth will quench thirst, and the diet should be
liquid, as milk, soups, gruels, white of egg, and water. The bowels
should be moved daily by rectal injections of soap and warm water. As
a matter of local treatment, the surface layer of the skin should be
kept intact if possible. Blisters are not to be disturbed unless they
are large and tense; if so, their bases may be pricked with a needle
sufficiently to let out the fluid contents.
Carron oil (equal parts of olive oil and limewater) has been the
common remedy for burns, and it is an efficient, though very dirty,
dressing, useful if the skin[Pg 175] is generally unbroken. It should be
applied on clean, soft linen or cotton cloth, which is soaked in the
oil, laid over the burned area, and covered with a thick layer of
cotton batting and a bandage. When the skin is denuded, leaving a raw
surface exposed, the burn must be treated on the same plan as wounds,
and should be kept as clean and free from germs as possible. An
ointment made of equal parts of boric acid and vaseline, spread
thickly on clean cloth, is a good antiseptic preparation in cases
where the skin is broken. It is best not to change the dressing
oftener than once in two or three days, unless the discharge or odor
are considerable. Fresh dressing is very painful and often harmful.
When the dressing is removed, warm saline solution (one teaspoonful of
common salt in a quart of water) is allowed to flow over the burn
until all discharge is washed off. Then the raw surface is dusted over
with pure boric acid or aristol, and the boric-acid ointment applied
as before. The cloth upon which the ointment is spread should be made
free from germs by boiling in water, and then drying it in an oven and
keeping it well wrapped in a clean towel except when wanted.
The same care is requisite as that described under wounds (p. 50) in
regard to cleanliness.
Very extensive burns are most satisfactorily treated by complete
immersion of the burned limbs or entire body in salt solution (same
strength as above), which[Pg 176] is kept at a temperature of from 94° to
104° F., according to the feelings of the patient. The patient lies in
a bath tub on horsehair, or better, rubber mattress and rubber
pillows; completely covered with water except the head. The urine and
bowel discharges must be passed in the water, which is then changed,
and the temperature is kept at an even mark by allowing warm water to
continually run into the tub to displace that which runs out. The
latter can be arranged by siphonage with a rubber tube. While this
method requires more care, and running hot and cold water, it is the
most comfortable treatment for these cases, usually attended by awful
suffering, and at the same time it is most favorable to healing.
It is beyond the scope of this work to describe the various
complications and the details of the after treatment in severe burns,
including skin grafting, which may tax all the ingenuity of the
skilled surgeon. It is hoped that the foregoing may give a clear idea
of the treatment to be pursued in emergencies and may prove of some
use to those who may unfortunately be compelled to care for burns
during a considerable time without the aid of a physician.
BURN BY STRONG ACID.
First Aid Rule 1.—Neutralize the acid. Scatter baking soda thickly
over burn, or pour limewater over it.
Rule 2.—Control pain. Wash off soda with stream[Pg 177] of water. Apply
Carron oil (equal parts of limewater and linseed oil or olive oil).
Bandage lightly.
BURN BY STRONG ALKALI.—As ammonia, quicklime, lye.
First Aid Rule 1.—Neutralize the alkali. Pour vinegar over the
burn.
Rule 2.—Control pain. Wash off vinegar with stream of water. Dry
gently. Apply vaseline or cold cream.
BURNS CAUSED BY STRONG MINERAL ACIDS OR BY ALKALIES.—If acids are the
cause, the skin should not be washed at first, but either chalk,
whiting, or some mild alkali, as baking soda, should be strewn over
the burn, and then after the effect of the acid is neutralized, wash
off the soda with stream of warm water. Dry gently with gauze. Apply
Carron oil or paste of boric acid and vaseline, equal parts. If strong
alkalies have been spilled on the skin, as ammonia, potash, or
quicklime, then vinegar is the proper substance to employ, followed by
washing. Then dry gently. Vaseline or cold cream is usually sufficient
as after treatment. Limewater is useful in counteracting the effect of
acids spattered in the eye. In the case of alkalies in the eye, the
vinegar used should be diluted with three parts of water. Albolene or
liquid vaseline is the best agent to drop in the eye after either
accident, in order to relieve the irri[Pg 178]tation and pain, and the
patient should stay in a dark room.
FROSTBITE, REAL FREEZING.—Nose, ears, fingers, toes; insensible to
touch, stiff, pale or blue. Person may be unconscious.
First Aid Rule 1.—Restore circulation. Rub gently, then vigorously,
with snow.
Rule 2.—Restore heat very gradually. Sudden heat is fatal. Keep in
cold room, and rub with cloth wet with very cold water till
circulation is established. Then rub with equal parts of alcohol and
water and expose gradually to heat of living room.
Rule 3.—If person ceases to breathe, resuscitate as if drowned. Open
his mouth, grasp his tongue, and pull it forward and keep it there.
Let another assistant grasp the arms just below the elbows and draw
them steadily upward by the sides of the patient's head to the ground,
the hands nearly meeting (which enlarges the capacity of the chest and
induces inspiration.) (See pp. 30 and 31.) While this is being done,
let a third assistant take position astride the patient's hips with
his elbows resting on his own knees, his hands extended ready for
action. Next, let the assistant standing at the head turn down the
patient's arms to the sides of the body, the assistant holding the
tongue changing hands if necessary to let the arms pass. Just before
the patient's hands reach the ground the man astride the body will
grasp the body with his[Pg 179] hands, the ball of the thumb resting on
either side of the pit of the stomach, the fingers falling into the
grooves between the short ribs. Now, using his knees as a pivot, he
will at the moment the patient's hands touch the ground throw (not too
suddenly) his whole weight forward on his hands, and at the same time
squeeze the waist between them, as if he wished to force something in
the chest upward out of the mouth; he will deepen the pressure while
he slowly counts one, two, three, four (about five seconds), then
suddenly lets go with a final push, which will send him back to his
first position. This completes expiration. (A child or a delicate
person must be more gently handled.)
At the instant of letting go, the man at the head of the patient will
again draw the arms steadily upward to the sides of the patient's head
as before (the assistant holding the tongue again changing hands to
let the arms pass, if necessary), holding them there while he slowly
counts one, two, three, four (about five seconds).
Repeat these movements deliberately and perseveringly twelve or
fifteen times in every minute—thus imitating the natural motions of
breathing. Continue the artificial respiration from one to four hours,
or until the patient breathes; and for a while after the appearance of
returning life carefully aid the first short gasps until deepened into
full breaths.
Keep body warm after this with warm-water bottles.
[Pg 180]FROSTBITE.—The nose, chin, ears, fingers, and toes are the parts
usually frozen, although severe results ending in death of the frozen
part occur more often owing to low vitality of the patient than to the
cold itself. In the milder degree of frostbite there is stiffness,
numbness, and tingling of the frozen member; the skin is of a pale,
bluish hue and somewhat shrunken. Recovery ensues with burning pain,
tingling, redness, swelling and peeling of the epidermis, as after
slight burns. The skin is icy cold, white, and insensitive in severe
forms of frostbite, and, if not skillfully treated, becomes, later,
either swollen and discolored, or shriveled, dry, and black. In either
case the frozen part dies and is separated from the living tissue
after the establishment of a sharp line of inflammation which results
in ulceration and formation of pus, and thus the dead part sloughs
off. It is, however, possible for a part thoroughly frozen to regain
its vitality.
Treatment.—The essential element in the treatment is to secure a very
gradual return of blood to the frozen tissues, and so avoid violent
inflammation. To obtain this result the patient should be cared for in
a cold room, the frozen parts are rubbed gently with snow, or cloth
wet with ice water, until they resume their usual warmth. Then it is
well to rub them with a mixture of alcohol and water, equal parts, for
a time and expose them to the usual temperature of a dwelling room.
Warm drinks are now administered to the patient. The[Pg 181] frozen member,
if hand or foot, is raised high in the air on pillows and covered well
with absorbent cotton and bandage. If much redness, swelling, and pain
result this dressing is removed and the part is wrapped in a single
thickness of cotton cloth kept continually wet with alcohol and water.
Subsequent treatment consists in keeping the damaged parts covered
with vaseline or cold cream, absorbent cotton, and bandage. If
blisters and sores result, the care is similar to that described for
like conditions under burns. If death of the frozen part becomes
inevitable, the hand or foot should be suspended in a nearly vertical
position to keep the blood out, and the part bathed twice daily with a
solution of corrosive sublimate (one 7.7 gr. tablet to pint of water),
dusted well with aristol, and dressed with absorbent cotton and
bandage until the dead tissue separates and comes away. If the frozen
part is large it may be necessary to remove it with a knife, but this
is not essential when the tips of the fingers or toes are frozen.
General Effect of Cold.—Sudden exposure to severe cold causes sleep,
stupor, and death. Persons found apparently frozen to death should be
brought into a cold room, which should be gradually heated, and the
body rubbed with snow or ice water, and artificial respiration
employed, as just directed. Attempts at resuscitation ought to be
persistent, as recoveries have been reported after several hours of
unconsciousness and apparent death from freezing.
[Pg 182]CHILBLAINS AND MILD FROSTBITES.—The effects of severe cold on the
body are very similar to those of intense heat, though they are very
much slower in making their appearance. After a person has frozen a
finger or toe he may not notice much inconvenience for days, when
suddenly violent inflammation may set in. The fingers, ears, nose, and
toes are the members which suffer most frequently from the effects of
cold. Similar symptoms of inflammation, described under burns, also
result from cold, that is, redness and swelling of the skin, blisters
with more severe and deeper inflammatory involvement, or, in case the
parts are thoroughly frozen, local death and destruction of the
tissues. But it is not essential that the body be exposed to the
freezing temperature or be frozen at all, in order that some harm may
result, for chilblains often follow when the temperature has not been
lower than 40° F., or thereabouts.
The effect of cold is to contract the blood vessels, with the
production of numbness, pallor, and tingling of the skin. When the
cold no longer acts then the blood vessels dilate to more than their
usual and normal state, and more or less inflammation results. The
more sudden the return to warmth the greater the inflammatory sequel.
Chilblains represent the mildest morbid effect of cold on the body.
They exist as bluish-red swellings of the skin, usually on the feet or
hands, but may attack the nose or ears, and are attended by burning,
itching,[Pg 183] and smarting. This condition is caused by dilatation of the
vessels following exposure to cold. It is more apt to happen in young,
anæmic women. Chilblains usually disappear during warm weather.
Scratching, friction, or the severity of the attack may lead to the
appearance of blisters and sores. In severe cases the fingers and toes
present a sausage-like appearance, owing to swelling.
Treatment.—Susceptible persons should wear thick, warm (not rough)
stockings and warm gloves. The chilled members must never be suddenly
warmed. Regular exercise and cold shower baths are good to strengthen
the circulation, but the feet and hands must be washed in warm water
only, and thoroughly dried. If sweating of these parts is a common
occurrence, starch or zinc oxide should be dusted on freely night and
morning. Cod-liver oil is an efficacious remedy in these cases; one
teaspoonful of Peter Möller's pure oil three times daily after meals.
The affected parts are bathed twice daily in a solution of zinc
acetate (one dram to one pint of water), and followed by the
application, on soft linen or cotton, of zinc-oxide ointment
containing two per cent of carbolic acid. If this is not curative,
iodine ointment mixed with an equal quantity of lard may be tried.
Exposure to cold will immediately bring on a recurrence of the
trouble. If the affection of the feet is severe the patient must rest
in bed. If the parts become blistered and open sores appear, then the
same treatment as for burns is[Pg 184] indicated. Wash with a weak solution
of corrosive sublimate (one tablet for surgical purposes in two quarts
of warm water) and apply an ointment of boric acid and vaseline, equal
parts, spread on soft, clean cotton or linen. Rest of the part and
existence in a warm atmosphere will complete the cure.
INGROWING TOE NAIL.—This is a condition in which the flesh along the
edges of the great toe nail becomes inflamed, owing either to
overgrowth of the nail or to pressure of the soft parts against it.
Improper footgear is the most common cause, as shoes which are too
narrow across the toes, or not long enough, or those with high heels
which throw the toes forward so that they are compressed by the toe of
the boot, especially in walking downhill.
A faulty mode of cutting the toe nails in a healthy foot may favor
ingrowing toe nails. Toe nails should be cut straight across, and not
trimmed away at the corners to follow the outline of the toes—as then
the flesh crowds in at the corners of the nails, and when the nail
pushes forward in its growth it presses into the flesh. Nails which
have a very rounded surface are more apt to produce trouble, because
then the edges are likely to grow down into the flesh. Inflammation in
ingrowing toe nail usually arises along the outer edge of the nail.
The flesh here becomes red, tender, painful, and swollen so that it
overlaps the nail. After a time "matter" or pus forms and finds its
way under the nail, and the parts[Pg 185] about it ulcerate, and "proud
flesh" or excessive granulation tissue springs up and imbeds the edge
of the nail. Wearing a shoe, or walking, becomes impossible. The
condition may last for months, or even years, if not rightly treated.
Treatment.—Properly fitting footgear must be worn—broad at the toes
with low heels and of sufficient length. If pus ("matter") forms, the
cut edge should be raised up by pushing in a little absorbent cotton
under the nail every day. Hot poultices of flaxseed meal, or other
material will relieve any special pain and inflammation. Soaking the
foot frequently in hot water, and observing especial cleanliness, will
aid recovery. Tannic acid, or some antiseptic powder like nosophen,
should be dusted along the edge of the nail, and the flesh crowded
away from the nail by pushing in a little cotton with some tannic acid
upon it.
If there is a raw surface about the border of the nail, powdered lead
nitrate may be dusted upon it each morning for four or five days, till
the ulcerated tissue shrinks away and the edge of the nail becomes
visible. The toe should be covered with absorbent cotton and a
bandage. As soon as the toe is really inflamed the case becomes
surgical, and as such demands the care of a surgeon when one can be
obtained.
FAINTING.
First Aid Rule 1.—Remove impediments to respiration. Remove collar,
loosen all waist bands and[Pg 186] cords, unhook corset or cut the laces at
person's back.
Rule 2.—Assist heart and brain with blood pressure. Put cushion
under buttocks, wind skirt close about legs, and raise feet in air.
Wait ten seconds.
Rule 3.—Aid respiration. Put mild smelling salts under nose. Spatter
cold water in face.
SUFFOCATION FROM GAS IN WELLS, CISTERNS, OR MINES, OR FROM
ILLUMINATING GAS.
First Aid Rule 1.—Remove quickly into pure air.
Rule 2.—Resuscitate as if drowned. Open his mouth, grasp his tongue,
pull it forward and keep it there. Let another assistant grasp the
arms just below the elbows, and draw them steadily upward by the sides
of the patient's head to the ground, the hands nearly meeting, which
enlarges the capacity of the chest and induces inspiration. (See pp.
30 and 31.) While this is being done, let a third assistant take
position astride the patient's hips with his elbows resting on his own
knees, his hands extended ready for action. Next, let the assistant
standing at the head turn down the patient's arms to the sides of his
body, the assistant holding the tongue, changing hands if necessary to
let the arms pass.
Just before the patient's hands reach the ground, the man astride the
body will grasp the body with his hands, the ball of the thumb resting
on either side of[Pg 187] the pit of the stomach, the fingers falling into
the grooves between the short ribs. Now, using his knees as a pivot,
he will, at the moment the patient's hands touch the ground, throw
(not too suddenly) his whole weight forward on his hands, and at the
same time squeeze the waist between them, as if he wished to force
something in the chest upward out of the mouth; he will deepen the
pressure while he slowly counts one, two, three, four (about five
seconds), then suddenly lets go with a final push, which will send him
back to his first position. This completes expiration. A child or a
delicate person must be more gently handled.
At the instant of letting go, the man at the head of the patient will
again draw the arms steadily upward, to the sides of the patient's
head, as before (the assistant holding the tongue again, changing
hands if necessary to let the arms pass, holding them there while he
slowly counts one, two, three, four (about five seconds)).
Repeat these movements deliberately and perseveringly twelve or
fifteen times in every minute, thus imitating the natural motions of
breathing. Continue the artificial respiration from one to four hours,
or until the patient breathes; and for a while after the appearance of
returning life, carefully aid the first short gasps until deepened
into full breaths.
Keep the body warm with hot-water bottles and blanket.
Rule 3.—Give oxygen to breathe from a cylinder,[Pg 188] for two days, at
short intervals, in the case of illuminating gas.
FIT; CONVULSION.
First Aid Rule 1.—Aid breathing. Loosen collar, waist bands, and
unhook corset, or cut the laces behind.
Rule 2.—Protect from injury. Gently restrain from falling or rolling
against furniture; lay flat on bed.
Rule 3.—Protect tongue from being bitten. Open jaws and put between
teeth rubber eraser tied to stout string, or rubber stopper tied to
stout string.
Rule 4.—Crush pearl of amyl nitrite in handkerchief, and hold close
to patient's nose and mouth, till face is red and patient relaxes.
Rule 5.—Let patient sleep after fit without rousing.
[Pg 189]
Part II
GERM DISEASES
BY
KENELM WINSLOW
[Pg 190]
[Pg 191]
CHAPTER I
Contagious Diseases
Scarlet Fever—Symptoms and Treatment—Precautions
Necessary—Measles—Communicating the
Disease—Smallpox—Vaccination—How to Diagnose Chickenpox.
ERUPTIVE CONTAGIOUS FEVERS (including Scarlet Fever, Measles, German
Measles, Smallpox, and Chickenpox).—These, with the exception of
smallpox, attack children more commonly than adults. As they all begin
with fever, and the characteristic rash does not appear for from one
to four days after the beginning of the sickness, the diagnosis of
these diseases must always be at the onset a matter of doubt. For this
reason it is wise to keep any child with a fever isolated, even if the
trouble seems to be due to "a cold" or to digestive disturbance, to
avoid possible communication of the disorder to other children. While
colds and indigestion are among the most frequent ailments of
children, they must not be neglected, for measles begins as a bad
cold, smallpox like the grippe, and scarlet fever with a sore throat
or tonsilitis, and vomiting.
By isolation is meant that the sick child should stay in a room by
himself, and the doors should be kept[Pg 192] closed and no children should
enter, nor should any objects in the room be removed to other parts of
the house after the beginning of its occupation by the patient.
The services of a physician are particularly desirable in all these
diseases, in order that an early diagnosis be made and measures be
taken to protect the family, neighbors, and community from contagion.
The failure of parents or guardians to secure medical aid for children
is regarded by the law as criminal neglect, and is subject to
punishment. Boards of health require the reporting of all contagious
diseases as soon as their presence is known, and failure to comply
with their rules also renders the offender liable to fine or
imprisonment in most places.
SCARLET FEVER (Scarlatina).—There is no difference between scarlet
fever and scarlatina. It is a popular mistake that the latter is a
mild type of scarlet fever. Fever, sore throat, and a bright-red rash
are the characteristics of this disease. It occurs most frequently in
children between the ages of two and six years. It is practically
unknown under one year of age. Prof. H. M. Biggs, of the New York
Department of Health, has seen but two undoubted cases in infants
under twelve months. It is rare in adults, and one attack usually
protects the patient from another. Second attacks have occurred, but
many such are more apparent than real, since an error in diagnosis is
not uncommon. The disease is communi[Pg 193]cated chiefly by means of the
scales of skin which escape during the peeling process, but may also
be acquired at any time from the onset of the attack from the breath,
urine, and discharges from the body; or from substances which have
come in contact with these emanations. Scarlet fever is probably a
germ disease, and the germs may live for weeks in toys, books,
letters, clothing, wall paper, etc. Close contact with the patient, or
with objects which have come in close touch with the patient, is
apparently necessary for contagion.
Period of Development.—After exposure to the germs of scarlet fever,
usually from two to five days elapse before the disease shows itself.
Occasionally the outbreak of the disease occurs within twenty-four
hours of exposure, and rarely is delayed for a week or ten days.
Symptoms.—The onset is usually sudden. It begins with vomiting (in
very young children sometimes convulsions), sore throat, fever,
chilliness, and headache. The tongue is furred. The patient is often
stupid; or may be restless and delirious. Within twenty-four hours or
so the rash appears—first on the neck, chest, or lower part of
back—and rapidly spreads over the trunk, and by the end of
forty-eight hours covers the legs and entire body excepting the face,
which may be simply flushed. The rash appears as fine, scarlet pin
points scattered over a background of flushed skin. At its fullest
development, at the end of the second or third day, the whole body may
present[Pg 194] the color of a boiled lobster. After this time the rash
generally fades away and disappears within five to seven days. It is
likely to vary much in intensity while it lasts. As the rash fades,
scaling of the skin begins in large flakes and continues from ten days
to as many weeks, usually terminating by the end of the sixth to
eighth week. One of the notable features is the appearance of the
tongue, at first showing red points through a white coating, and after
this has cleared away, in presenting a raspberry-like aspect. The
throat is generally deep red, and the tonsils may be dotted over with
white spots (see Tonsilitis) or covered with a whitish or gray
membrane suggesting diphtheria, which occasionally complicates scarlet
fever. The fever usually is high (103° to 107° F), and the pulse
ranges from 120 to 150; both declining after the rash is fully
developed, generally by the fourth day. The urine is scanty and dark.
There is, however, great variation in the symptoms as to their
presence or absence, intensity, and time of occurrence and
disappearance.
Complications and Sequels.—These are frequent and make scarlet fever
the most dreaded of the eruptive diseases, except smallpox. Enlarged
glands under the jaw and at the sides of the neck are common, and
appear as lumps in these sites. Usually not serious, they may enlarge
and threaten life. Pain and swelling in the joints, especially of the
elbows and knees, are not rare, and may be the precursors of serious
inflam[Pg 195]mation of these parts. One of the most frequent and serious
complications of scarlet fever is inflammation of the kidneys,
occurring more often toward the end of the second week of the disease.
Examination of the urine by the attending physician at frequent
intervals throughout the course of the disorder is essential, although
puffiness of the eyelids and face, and of the feet, ankles, and hands,
together with lessened secretion of urine—which often becomes of a
dark and smoky hue—may denote the onset of this complication. The
disease of the kidneys usually results in recovery, but occasionally
in death or in chronic Bright's disease of these organs. Inflammation
of the middle ear with abscess, discharge of matter from the ear
externally, and—as the final outcome—deafness, is not uncommon. This
complication may be prevented to a considerable extent by spraying the
nose and throat frequently and by the patient's use of a nightcap with
earlaps, if the room is not sufficiently warm. Inflammation of the
eyelids is an occasional complication. The heart is sometimes attacked
by the toxins of the disease, and permanent damage to the organ, in
the form of valvular trouble, may result. Blindness and nervous
disorders are among the rarer sequels including paralyses and St.
Vitus's dance.
Determination of Scarlet Fever.—When beginning with vomiting,
headache, high fever, and sore throat, and followed in twenty-four
hours with a general scarlet rash, this is not difficult; but
occasionally[Pg 196] other diseases present rashes, as indigestion, grippe,
and German measles, which puzzle the most acute physicians. Measles
may be distinguished from scarlet fever in that measles appears first
on the face, the rash is patchy or blotchy, and does not show for
three to four days after the beginning of the sickness. The patient
seems to have a bad cold, with cough, running at the nose, and sore
eyes. German measles is mild, and while the rash may look something
like that of scarlet fever, the patient does not seem generally ill,
is hardly affected at all, though rarely troubled with slight catarrh
of the nose. In no sickness are the services of a physician more
necessary than in scarlet fever; first, to determine the existence of
the disease, and then to prevent or combat the complications which
often approach insidiously.
Outlook.—The average death rate of scarlet fever is about ten per
cent. It is very fatal in children about a year old, and most of the
deaths occur in those under the age of six. But the mortality varies
greatly at different times and in different epidemics. In 1904–5, in
many parts of the United States, the disease was very prevalent and
correspondingly mild, and deaths were rare.
Duration of Contagion.—The disease is commonly considered contagious
only so long as peeling of the skin lasts. But it seems probable that
any catarrhal secretion from the nose, throat, or ear is capable of
communicating the germs from a patient to another[Pg 197] person for many
days after other evidences of the disease are past. Scarlet fever
patients should always be isolated for as long a period as six
weeks—and better eight weeks—without regard to any shorter duration
of peeling, and if peeling continues longer, so should the isolation.
Treatment.—In case a physician is unobtainable the patient must be
put to bed in the most airy, sunshiny room, which should be heated to
70° F., and from which all the unnecessary movables should be taken
out before the entrance of the patient. A flannel nightgown and light
bed clothing are desirable. The fever is best overcome by cold
sponging, which at the same time diminishes the nervous symptoms, such
as restlessness and delirium. The body is sponged—part at a
time—with water at the temperature of about 70° F., after placing a
single thickness of old cotton or linen wet with ice or cold water
(better an ice cap) over the forehead. The part is thoroughly dried as
soon as sponged, and the process is repeated whenever the temperature
is over 103° F. There need be no fear that the patient may catch cold
if only a portion of the body is exposed at any one time. If there is
any chilliness following sponging, a bag or bottle containing hot
water may be placed at the feet. It is well that a rubber bag
containing ice, or failing this a cold cloth, be kept continually on
the head while fever lasts. The throat should be sprayed hourly with a
solution of hydrogen peroxide (full strength) and the nose with[Pg 198] the
same, diluted with an equal amount of water, three times a day. The
outside of the throat it is wise to surround with an ice bag, or
lacking this, a cold cloth frequently wet and covered with a piece of
oil silk (or rubber) and flannel.
The diet should consist of milk, broths, or thin gruels, and plenty of
water should be allowed. Sweet oil or carbolized vaseline should be
rubbed over the whole body night and morning during the entire
sickness and convalescence. The bowels must be kept regular by
injections or mild cathartics, and, after the fever subsides,
vegetables, fruit, cereals, and milk may be permitted, together with
meat or eggs once daily. It is imperative for the nurse and also the
mother to wear a gown and cap over the outside clothes, to be slipped
off in the hall at the door of the sick room when leaving the latter.
MEASLES.—Measles is a contagious disease, characterized by a
preliminary stage of fever and catarrh of the eyes, nose, and throat,
and followed by a general eruption on the skin. One attack practically
protects a person from another, yet, on the other hand, second attacks
occur with extreme rarity. It is more contagious than scarlet fever,
and isolation of a patient in a house is of less service in preventing
communication to other inmates, whereas in scarlet fever half the
number of susceptible children may escape the disease through this
precaution. The germs which cause measles perish rapidly, so that
infected clothes[Pg 199] or other objects merely require a thorough airing to
be rendered safe, whereas in scarlet fever the danger of transmission
of the contagion may lurk in infected clothing and other substances
for weeks, unless they are subjected to proper disinfection. A patient
with measles is capable of communicating the disorder from its onset,
before the appearance of the rash, through the breath, discharges from
the nose and eyes, tears and saliva and all the secretions. At the end
of the third week of the disease the patient is usually incapable of
giving the disease to others. Close contact with a patient is commonly
necessary for one to acquire the disease, but it is frequently claimed
that it is carried by a third person in the clothes, as by a nurse. It
is infrequent in infants under six months, and most frequent between
the second and sixth year. Adults are attacked by measles more often
than by scarlet fever.
Development.—A period of from seven to sixteen days after exposure to
measles elapses before the disease becomes apparent.
Symptoms.—The disease begins like a severe nasal catarrh with fever.
The eyes are red and watery, the nose runs, and the throat is
irritable, red, and sore, and there is some cough, with chilliness and
muscular soreness. The fever, higher at night, varies from 102° to
104° F., and the pulse ranges from 100 to 120. There is often marked
drowsiness for a day or two before the rash appears. Coated tongue,
loss of appe[Pg 200]tite, occasional vomiting, and thirst are present during
this period. The appearance of minute, whitish spots, surrounded by a
red zone, may often be seen in the inside of the mouth opposite the
back teeth for some days before the eruption occurs.
The preliminary period, when the patient seems to be suffering with a
bad cold, lasts for four days usually, and on the evening of the
fourth day the rash breaks out. It first appears on the face and then
spreads to the chest, trunk, and limbs. Two days are generally
required for the complete development of the rash; it remains thus in
full bloom for about two days more, then begins to subside, fading
completely in another two days—six days in all.
The rash appears as bright-red, slightly raised blotches on the face,
which is generally somewhat swollen. The same rash extends to the
abdomen, back, and limbs. Between the mottled, red rash may be seen
the natural color of the skin. At this time the cough may be hoarse
and incessant, and the eyes extremely sensitive to light. The fever
and other symptoms abate when the rash subsides, and well-marked
scaling of the skin occurs.
Complications and Sequels.—Severe bronchitis, pneumonia, croup,
laryngitis, sore eyes, ear abscess and deafness, violent diarrhea,
convulsions, and, as a late result, consumption sometimes accompany or
follow measles. For the consideration of these disorders, see special
articles in other parts of this work.
[Pg 201]Outlook.—The vast majority of healthy patients over two years old
recover from measles completely. Younger children, or those suffering
from other diseases, may die through some of the complications
affecting the lungs. The disease is peculiarly fatal in some epidemics
occurring among those living in unhygienic surroundings, and in
communities unaccustomed to the ravages of measles. Thus, in an
epidemic attacking the Fiji Islanders, over one-quarter of the whole
population (150,000) died of measles in 1875. Measles is more severe
in adults than in children.
Diagnosis.—For one not familiar with the characteristic rash a
written description of it will not suffice for the certain recognition
of the disease, but if the long preliminary period of catarrh and
fever, and the appearance of the eruption on the fourth day, be taken
into account—together with the existence of sore eyes and hoarse,
hard cough—the determination of the presence of measles will not be
difficult in most cases.
Treatment.—The patient should be put to bed in a darkened,
well-ventilated room at a temperature of 68° to 70° F. While by
isolation of the patient we may often fail to prevent the occurrence
of measles in other susceptible persons in the same house, because of
the very infectious character of the disease, and because it is
probable that they have already been exposed during the early stages
when measles was not suspected, yet all possible precautions should be
adopted promptly. For this reason other children in the house should
be[Pg 202] kept from school and away from their companions, and they ought
not to be sent away from home to spread the disease elsewhere. The
bowels should be kept regular by soapsuds injections or by mild
cathartics, as a Seidlitz powder. If the fever is over 103° F. and is
accompanied by much distress and restlessness, children may be sponged
with tepid water, and adults with water at 80° F., every two hours or
so as directed under scarlet fever. When cough is incessant or the
rash does not come out well, there is nothing better than the hot
pack.
The patient is stripped and wrapped from feet to neck in a blanket
wrung out of hot water containing two teaspoonfuls of mustard stirred
into a gallon of water. This is then covered with two dry blankets and
the patient allowed to remain in the blankets for two or three hours,
when the application may be repeated. It is well to keep a cold cloth
on the head during the process. Cough is also relieved by a mixture
containing syrup of ipecac, twenty drops; paregoric, one teaspoonful,
for an adult (or one-third the dose for a child of six), which should
be given in one-quarter glass of water and may be repeated every two
hours. If there is hoarseness, the neck should be rubbed with a
mixture of sweet oil, two parts; and oil of turpentine, one part, and
covered with a flannel bandage. The cough mixture will tend to relieve
this condition also. A solution of boric acid (ten grains of boric
acid to the ounce of[Pg 203] water) is to be dropped in both eyes every two
hours with a medicine dropper. Although usually mild, the eye symptoms
may be very severe and require special treatment, and considerably
impaired vision may be the ultimate result. Severe diarrhea is
combated with bismuth subnitrate, one-quarter teaspoonful, every three
hours. For adults, the diet consists of milk, broths, gruels, and raw
eggs. Young children living on milk mixtures should receive the
mixture to which they are accustomed, diluted one-half with barley
water. Nourishment must be given every two hours except during sleep.
The patient should be ten days in bed, and should remain three days in
his room after getting up (or three weeks in all, if there are others
who may contract measles in the house), and after leaving his room
should stay in the house a week longer. The principal danger after an
attack of measles is of lung trouble—pneumonia or tuberculosis
(consumption)—and the greatest care should be exercised to avoid
exposure to the wet or to cold draughts.
GERMAN MEASLES (Rötheln).—German measles is related neither to
measles nor scarlet fever, but resembles them both to a certain
extent—more closely the former in most cases. It is a distinct
disease, and persons who have had both measles and scarlet fever are
still susceptible to German measles. One attack of German measles
usually protects the patient from another. Adults, who have not been
previously attacked, are almost as liable to German measles as
children, but[Pg 204] it is rare that infants acquire the disease. It is a
very contagious disorder—but not so much so as true measles—and
often occurs in widespread epidemics. The breath and emanations from
the skin transmit the contagium from the appearance of the first
symptom to the disappearance of the eruption.
Development.—The period elapsing after exposure to German measles and
before the appearance of the symptoms varies greatly—usually about
two weeks; it may vary from five to eighteen days.
Symptoms.—The rash may be the first sign of the disease and more
frequently is so in children. In others, for a day or two preceding
the eruption, there may be headache, soreness, and redness of the
throat, the appearance of red spots on the upper surface of the back
of the mouth, chilliness, soreness in the muscles, loss of appetite,
watering of the eyes. Catarrhal symptoms are most generally absent, an
important point in diagnosis. When present, they are always mild.
These preliminary symptoms, if present, are much milder and of shorter
duration than in measles, where they last for four days before the
rash appears; and the hard, persistent cough of measles is absent in
German measles. Also, while there is sore throat in the latter, there
is not the severe form with swollen tonsils covered with white spots
so often seen in scarlet fever. Fever is sometimes absent in German
measles; usually it ranges about 100° F., rarely over 102° F. Thus,
German measles differs markedly from both scarlet[Pg 205] fever and measles
proper. The rash usually appears first on the face, then on the chest,
and finally covers the whole body, in the space of a few
hours—twenty-four hours at most. The eruption takes the form of
rose-red, round or oval, slightly raised spots—from the size of a pin
head to that of a pea—sometimes running together into uniform
redness, as in scarlet fever. The rash remains fully developed for
about two days, and often changes into a coppery hue as it gradually
fades away. There are often lumps—enlarged glands—to be felt under
the jaw, on the sides and back of the neck, which occur more commonly
in German than in true measles. The glands at the back of the neck are
the most characteristic. They are enlarged in about two-thirds of the
cases.
Determination.—The diagnosis or determination of the existence of
measles must be made, in the absence of a physician, on the general
symptoms rather than on the rash, which requires experience for its
recognition and is subject to great variations in appearance, at one
time simulating measles, at another scarlet fever.
German measles differs from true measles in the following points: the
preliminary period—before the rash—is mild, short, or absent; fever
is mild or absent; the cold in the nose and eyes and cough are slight
or may be absent, as contrasted with these symptoms in measles, while
the enlarged glands in the neck are more pronounced than in measles.
The onset of German[Pg 206] measles is not so sudden as in scarlet fever and
not accompanied with vomiting as in the latter, while the sore throat
and fever are much milder in German measles. The peeling, which is so
prominent in scarlet fever with the disappearance of the rash, is not
infrequently present. It may be absent. Its presence or absence seems
to depend upon the severity of the eruption. The desquamation when
present is finer than in either measles or scarlet fever.
Outlook.—Recovery from German measles is the invariable rule, and
without complications or delay.
Treatment.—Little or no treatment is required. The patient should
remain in bed in a darkened room on a liquid diet while fever lasts,
and be isolated from others indoors until all signs of the eruption
are passed. The eyes should be treated with boric acid as in measles;
the diet, during the fever, consisting of milk, broths, thin cereals,
beef juice, raw eggs or eggnog, for adults and older children; while
infants should have their milk mixture diluted one-half with barley
water. A bath and fresh clothing for the patient, and thorough
cleansing and airing of the sick room and clothing are usually
sufficient after the passing of the disease without chemical
disinfection.
SMALLPOX.—Smallpox is one of the most contagious diseases known. It
is extremely rare for anyone exposed to the disease to escape its
onslaught unless previously protected by vaccination or by a former
attack of the disease. One is absolutely safe from[Pg 207] acquiring smallpox
if recently and successfully vaccinated, and thus has one of the most
frightful and fatal scourges to which mankind has ever been subject
been robbed of its dangers. The contagium is probably derived
entirely from the scales and particles of skin escaping from smallpox
patients, and in the year 1905–6 the true germ of the disease was
discovered by Councilman, of Boston. It is not necessary to come in
direct contact with a patient to contract the disease, as the
contagium may be transmitted some little distance through the air,
possibly even outside of the sick room. One attack almost invariably
protects against another. All ages are liable to smallpox; it is
particularly fatal in young children, and during certain epidemics has
proved more so in colored than in white people.
Development.—A period of ten or twelve days usually elapses after
exposure to smallpox before the appearance of the first symptoms of
the disease. This period may vary, however, from nine to fifteen days.
Symptoms.—There is a preliminary period of from twenty-four to
forty-eight hours after the beginning of the disease before an
eruption occurs. The onset is ushered in by a set of symptoms
simulating those seen in severe grippe, for which smallpox is often
mistaken at this time. The patient is suddenly seized with a chill,
severe pains in the head, back, and limbs, loss of appetite and
vomiting, dizziness on sitting up, and fever—103° to 105° F. In young
children convul[Pg 208]sions often take the place of the chill seen in
adults. On the second day a rash often appears on the lower part of
the belly, thighs, and armpits, which may resemble that characteristic
of measles or scarlet fever, but does not last for over a day or two.
It is very evanescent and, consequently, rarely seen. Diarrhea often
occurs, as well as vomiting, particularly in children. On the evening
of the fourth day the true eruption usually appears; first on the
forehead or face, and then on the arms, hands, and legs, palms, and
soles. The eruption takes successively four forms: first, red, feeling
like hard pimples or like shot; then, on the second or third day of
the eruption, these pimples become tipped with little blisters with
depressed centers, and surrounded by a red blush. Two or three days
later the blisters are filled with "matter" or pus and present a
yellowish appearance and are rounded on top. Finally, on about the
tenth day of the eruption, the pustules dry up and the matter exudes,
forming large, yellowish or brownish crusts, which, after a while,
drop off and leave red marks and, in severe cases, pitting. The fever
preceding the eruption often disappears upon the appearance of the
latter and in mild cases does not reappear, but in severe forms the
temperature remains about 100° F., and when the eruption is at its
height again mounts to 103° to 105° F., and gradually falls with
convalescence. The eruption is most marked on the face, hands, and
forearms, and occurs less thickly on the body. It appears also in the
mouth and throat and[Pg 209] when fully developed on the face gives rise to
pain and considerable swelling and distortion of the features, so that
the eyes are closed and the patient becomes frightfully disfigured and
well-nigh unrecognizable. Delirium is common at this time, and
patients need constant watching to prevent their escape from bed. In
the severe forms the separate eruptive points run together so that the
face and hands present one distorted mass of soreness, swelling, and
crusting. In these, pitting invariably follows, while in those cases
where the eruption remains distinct, pitting is not certain to occur.
A still worse form is that styled "black smallpox," in which the skin
becomes of a dark-purplish hue, from the fact that each pustule is a
small blood blister, and bleeding occurs from the nose, mouth, etc.
These cases are almost, without exception, fatal in five to six days.
The patient may say that the eruption was the first symptom he
observed. This was particularly noticed in negroes, many of whom had
never been vaccinated. The eruption may exhibit but a dozen or so
points, especially about the forehead, wrists, palms, and soles. After
the first four days the fever and all the disagreeable symptoms may
subside, and the patient may feel absolutely well. The eruption,
however, passes through the stages mentioned, although but half the
time may be occupied by the changes; five or six days instead of ten
to twelve for crusts to form. In such cases the death rate has been
exceedingly low, al[Pg 210]though it is perfectly possible for a person to
contract the most severe smallpox from one of these mild (and often
unrecognized) cases, as has unfortunately happened. Smallpox occurring
after successful vaccination resembles, in its characteristics, the
cases just described, and unless vaccination had been done many years
previously, the results are almost always favorable as regards life
and absence of pitting.
Detection.—Smallpox is often mistaken for chickenpox, or some of the
skin diseases, in its mild forms. The reader is referred to the
article on chickenpox for a consideration of this matter. The mild
type should be treated just as rigidly as severe cases with regard to
isolation and quarantine, being more dangerous to the community
because lightly judged and not stimulating to the adoption of
necessary precautions. The preliminary fever and other symptoms
peculiar to smallpox will generally serve to determine the true nature
of the disease, since these do not occur in simple eruptions on the
skin. The general symptoms and course of smallpox must guide the
layman rather than the appearance of the eruption, which requires
educated skill and experience to recognize. Chickenpox in an adult is
less common than in children. Smallpox is very rare in one who has
suffered from a previous attack of the disease or in one who has been
successfully vaccinated within a few years.
Outlook.—The death rate of smallpox in those who have been previously
vaccinated at a compara[Pg 211]tively recent date, or in varioloid, as it is
called when thus modified by vaccination, is only 1.2 per cent. There
are, however, severe cases following vaccinations done many years
previous to the attack of smallpox. While these cannot be called
varioloid, yet the death rate is much lower than in smallpox occurring
in the unvaccinated. Thus, before the mild epidemic of 1894 the death
rate in the vaccinated was sixteen per cent; since 1894 it has been
only seven per cent; while in the unvaccinated before 1894 it was
fifty-eight per cent; and since that date it has been but seventeen
per cent, as reported by Welch from the statistics of 5,000 cases in
the Philadelphia Municipal Hospital.
Complications.—While a variety of disorders may follow in the course
of smallpox, complications are not very frequent in even severe cases.
Inflammation of the eyelids is very common, however, and also boils in
the later stages. Delirium and convulsions in children are also
frequent, as well as diarrhea; but these may almost be regarded as
natural accompaniments of the disease. Among the less common
complications are: laryngitis, pneumonia, diseases of the heart,
insanity, paralysis, various skin eruptions, inflammation of the
joints and of the eyes and ears, and baldness.
Treatment.—Prevention is of greatest importance. Vaccination stands
alone as the most effective preventive measure in smallpox, and as
such has no rival in the whole domain of medicine. The modern method
includes the inoculation of a human being with matter[Pg 212] taken from one
of the eruptive points on the body of a calf suffering with cowpox.
Whether cowpox is a modified form of smallpox or a distinct disease is
unknown.
The period of protection afforded by a successful vaccination is
uncertain, because it varies with different individuals. In a general
way immunity for about four or five years is thus secured; ten or
twelve years after vaccination the protection is certainly lost and
smallpox may be then acquired. Every individual should be vaccinated
between the second and third month after birth, and between the ages
of ten and twelve, and at other times whenever an epidemic threatens.
An unvaccinated person should be vaccinated and revaccinated, until
the result is successful, as immunity to vaccination in an
unvaccinated person is practically unknown. When unsuccessful, the
vaccine matter or the technique is faulty. A person continuously
exposed to smallpox should be vaccinated every few weeks—if
unsuccessful, no harm or suffering follow; if successful, it proves
liability to smallpox. A person previously vaccinated successfully may
"take" again at any time after four or five years, and, in event of
possible exposure to smallpox, should be revaccinated several times
within a few weeks—if the vaccination does not "take"—before the
attempt is given up. An unvaccinated person, who has been exposed to
smallpox, can often escape the disease if successfully vaccinated
within[Pg 213] three days from the date of the exposure, but is not sure to
do so.
Diseases are not introduced with vaccination now that the vaccine
matter is taken from calves and not from the human being, as formerly.
Most of the trouble and inflammation of the vaccinated part following
vaccination may be avoided by cleanliness and proper care in
vaccinating.
In the absence of a physician, vaccination may be properly done by any
intelligent person when the circumstances demand it. Vaccination is
usually performed upon the outside of the arm, a few inches below the
shoulder, in the depression situated in that region. If done on the
leg, the vaccination is apt to be much more troublesome and may
confine the patient to bed. The arm should be thoroughly washed in
soap and warm water, from shoulder to elbow, and then in alcohol
diluted one-third with water. When this has evaporated (without
rubbing), the dry arm is scratched lightly with a cold needle which
has previously been held in a flame and its point heated red hot. The
point must thereafter not be touched with anything until the skin is
scratched with it. The object is not to draw blood, but to remove the
outer layer of skin, over an area about one-fourth of an inch square,
so that it appears red and moist but not bleeding. This is
accomplished by very light scratching in various directions. Another
spot, about an inch or two below, may be similarly treated. Then
vaccine matter, if[Pg 214] liquid, is squirted on the raw spots, or, if dried
on points, the ivory point is dipped in water which has been boiled
and cooled, and rubbed thoroughly over the raw places. The arm must
remain bare and the vaccination mark untouched until the surface of
the raw spot is perfectly dry, which may take half an hour. A piece of
sterilized surgical gauze, reaching halfway about the arm and kept in
place with strips of adhesive plaster (or an absolutely clean
handkerchief bound about the arm, and held by sewing or safety pins),
ought to cover the vaccination for three days. After this time the
sore must only come in contact with soft and clean old cotton or
linen, which may be daily pinned in the sleeve of the under garment.
If the scab is knocked off and an open sore results it should be
treated like any wound.
If the vaccination "takes," it passes through several stages. On the
third day following vaccination a red pimple forms at the point of
introduction of the matter, which is surrounded by a circle of
redness. Some little fever may occur. On the fifth day a blister or
pimple containing clear fluid with a depressed center is seen, and a
certain amount of hard swelling, itchiness, and pain is present about
the vaccination. A sore lump (gland) is often felt under the arm. The
full development is reached by the eighth day, when the pimple is full
and rounded and contains "matter," and is surrounded by a large area
of redness. From the eleventh day the vaccination sore[Pg 215] dries, and a
brown scab forms over it about the end of the fourteenth day, and the
redness and swelling gradually depart. At the end of about three weeks
the scab drops off, leaving a pitted scar or mark. Not infrequently
the vaccination results in a very slight pimple and redness, which
passes through the various stages described, in a week or ten days, in
which case the vaccination should be repeated. Unless the vaccination
follows very closely the course described, it cannot be regarded as
successful, although after the first one or two vaccinations the
result is often not so severe, and the time of completion of the
various stages somewhat shortened.
Rarely an eruption, resembling that at the vaccination site, appears
on the vaccinated limb and even becomes general upon the body, due to
urticaria or to inoculation, through scratching.
The special treatment of an attack of smallpox is largely a matter of
careful nursing. A physician or nurse can scarcely lay claim to any
great degree of heroism in caring for smallpox patients, as there is
no danger of contracting the disease providing a successful
vaccination has been recently performed upon them. The patient should
be quarantined in an isolated building, and all unnecessary articles
should be removed from the sick room, in the way of carpets and other
furnishings. It is well that the room be darkened to save irritation
of the eyes. The diet should be liquid: milk, broths, and gruels.
Lauda[Pg 216]num, fifteen drops, or paregoric, one tablespoonful in water,
may be given to adults, once in three hours, to relieve pain during
the first few days. Sponging throughout the course of the disease is
essential; first, with cool water, as directed for scarlet fever, with
the use of cold on the head to relieve the itching, fever, and
delirium. The cold pack is still more efficient. To give this, the
patient is wrapped in a sheet wrung out in water at a temperature
between 68° and 75° F. The sheet surrounds the naked body from feet to
neck, and is tucked between the legs and between the body and arms;
the whole is then covered with a dry blanket, and a cold, wet cloth or
ice cap is placed upon the head. The patient may be permitted to
remain in the pack for an hour, when it may be renewed, if necessary,
to allay fever and restlessness; otherwise it may be discontinued. The
cold sponging or cold pack are indicated when the temperature is over
102.5° F., and when with fever there are restlessness and delirium.
Great cleanliness is important throughout the disease; the bedclothes
should be changed daily and the patient sponged two or three times
daily with warm water, unless fever is high. Cloths wet with cold
carbolic-acid solution (one-half teaspoonful to the pint of hot water)
should be kept continuously on the face and hands. Holes are cut in
the face mask for the eyes, nose, and mouth, and the whole covered
with a similar piece of oil silk to keep in the moisture. Such
applications give much[Pg 217] relief, and to some extent prevent pitting.
The hair must be cut short, and crusts on the scalp treated with
frequent sponging and applications of carbolized vaseline, to soften
them and hasten their falling. The boric-acid solution should be
dropped into the eyes as recommended for measles, and the throat
sprayed every few hours with Dobell's solution. Diarrhea in adults may
be checked with teaspoonful doses of paregoric given hourly in water.
Vaseline and cloths used on a patient must not be employed on another,
as boils are thus readily propagated. All clothing, dishes, etc.,
coming in contact with a patient must be boiled, or soaked in a
two-per cent carbolic-acid solution for twenty-four hours, or burned.
When the patient is entirely free from scabs, after bathing and
putting on disinfected or new clothes outside of the sick room, he is
fit to reënter the world.
CHICKENPOX.—Chickenpox is a contagious disease, chiefly attacking
children. While it resembles smallpox in some respects, at times
simulating the latter so closely as to puzzle physicians, it is a
distinct disease and is in no way related to smallpox. This is shown
by the fact that chickenpox sometimes attacks a patient suffering
with, or recovering from, smallpox. Neither do vaccination nor a
previous attack of smallpox protect an individual from chickenpox.
Chickenpox is not common in adults, and its apparent presence in a
grown person should awaken the liveliest suspicion lest the case be
one of smallpox,[Pg 218] since this mistake has been frequently made, and
with disastrous results, during an epidemic of mild smallpox. One
attack of chickenpox usually protects against another, but two or
three attacks in the same individual are not unknown. The disease may
be transmitted from the patient to another person from the time of the
first symptom until the disappearance of the eruption. The disease
ordinarily occurs in epidemics, but occasionally in isolated cases.
Development.—A period of two weeks commonly elapses after exposure to
the disease before the appearance of the first symptom of chickenpox,
but this period may vary from thirteen to twenty-one days.
Symptoms.—The characteristic eruption is often the first warning of
chickenpox, but in some cases there may be a preliminary period of
discomfort, lasting for a few hours, before the appearance of the
rash; particularly in adults, in whom the premonitory symptoms may be
quite severe. Thus, there may be chilliness, nausea, and even
vomiting, rarely convulsions in infants, pain in the head and limbs,
and slight fever (99° to 102° F.) at this time. The eruption shows
first on the body, in most cases, especially the back. It consists of
small red pimples, which rapidly develop into pearly looking blisters
about as large as a pea to that of the finger nail, and are sometimes
surrounded by a red blush on the skin. These blisters vary in number,
from a dozen or so to two hundred. They do not run together, and in
three to four days dry up, be[Pg 219]come shriveled and puckered, and covered
with a dark-brown or blackish crust, and drop off, leaving only
temporary red spots in most cases. The fever usually continues during
the eruption. During the first few days successive fresh crops of
fresh pimples and blisters appear, so that while the first crop is
drying the next may be in full development. This forms one of its
distinguishing features when chickenpox is compared with smallpox. In
chickenpox the eruption is seen on the unexposed skin chiefly, but may
occur on the scalp and forehead, and even on the palms, soles,
forearms, and face. In many cases the eruption is found in the mouth,
on its roof, and the inside of the cheeks. The blisters rarely contain
"matter" or pus, as in smallpox, unless they are scratched. Scratching
may lead to the formation of ugly scars and should be prevented,
especially when the eruption is on the face. Pitting rarely occurs.
Determination.—The discrimination between chickenpox and smallpox is
sometimes extremely puzzling and demands the skill of an experienced
physician. When one is unavailable, the following points may serve to
distinguish the two disorders: smallpox usually begins like a severe
attack of grippe, with pain in the back and head, general pains and
nausea or vomiting, with high fever (103° to 104° F.) These last two
or three days, and may completely subside when the rash appears. In
chickenpox preliminary discomfort is absent, or lasts but a few hours
before[Pg 220] the eruption. The eruption of smallpox usually occurs first on
the forehead, near the hair, or on the palms of the hands, soles of
the feet, the arms and legs, but is usually sparse on the body. The
eruption appears about the same time in smallpox and not in successive
crops, as in chickenpox. Chickenpox is more commonly a disease of
childhood; smallpox attacks all ages. The crusts in chickenpox are
thin, and appear in four or five days, while those of smallpox are
large and yellow, and occur after ten or twelve days.
Outlook.—Chickenpox almost invariably results in a rapid and speedy
recovery without complications or sequels. The young patients often
feel well throughout the attack, which lasts from eight to twelve
days.
Treatment.—Children should be kept in bed during the eruptive stage
until the blisters have dried. To prevent scratching, the calamine
lotion may be used (Vol. II, p. 145), or carbolized vaseline, or
bathing with a solution of baking soda, one teaspoonful to the pint of
tepid water. The diet should be that recommended for German measles.
Patients should be kept in the house and isolated until all signs of
the eruption are passed, and then receive a good bath and fresh
clothing before mingling with others. The sick room should be
thoroughly cleaned and aired; thorough chemical disinfection is not
essential.
The services of a physician are always desirable in order that it may
be positively determined that the disease is not a mild form of
smallpox.
[Pg 221]
CHAPTER II
Infectious Diseases
Typhoid Fever—How it is Contracted—Complications and Sequels—Rest,
Diet, and Bathing the Requisites—Mumps—Whooping Cough—Erysipelas.
TYPHOID FEVER (ENTERIC FEVER).—Through ignorance which prevailed
before the discovery of the germ of typhoid fever and exact methods
for determining the presence of the same, the term was loosely applied
and is to this day. Thus mild forms of typhoid are called gastric
fever, slow fever, malarial fever, nervous fever, etc., all true
typhoid in most cases; while typhoid fever, common to certain
localities and differing in some respects from the typical form, is
often named after the locality in which it occurs, as the "mountain
fever" common to the elevated regions of the western United States.
This want of information is apt to prevail in regions remote from
medical centers, and leads to neglect of the necessary strict measures
for the protection of neighboring communities, for the excretion of
one typhoid patient has led to thousands of cases and hundreds of
deaths.
Typhoid fever is a communicable disease caused by a germ which attacks
the intestines chiefly, but also invades the blood, and at times all
the other parts of[Pg 222] the body, and is characterized by continued fever,
an eruption, tenderness and distention of the bowels, and generally
diarrhea. It is common to all parts of the earth in the temperate
zones, and occurs more frequently from July to December in the north
temperate zone, from February to July in the south temperate zone. It
is most prevalent in the late summer and autumn months and after a
hot, dry summer. Individuals between the ages of fifteen and thirty
are more prone to typhoid fever, but no age is exempt. The sexes are
almost equally liable to the disease, although it is said that for
every four female cases there are five male cases. The robust succumb
as readily as the weak.
Cause and Modes of Communication.—While the typhoid germ is always
the immediate cause, yet it is brought in contact with the body in
various ways. Contamination of water supply through bad drainage is
the principal source of epidemics of typhoid. Before carefully
protected public water supplies were in vogue in Massachusetts, there
were ninety-two deaths from typhoid fever in 100,000 inhabitants,
while thirty-five years after town water supplies became the rule,
there were only nineteen deaths for the same population. Whenever
typhoid is prevalent, the water used for drinking and all other
household purposes should be boiled, and uncooked food should be
avoided. Flies are carriers of typhoid germs by lighting on the nose,
the mouth, and the discharges of typhoid patients, and then conveying
the germs to food, green vege[Pg 223]tables, and milk. Cooking the food,
preventing contact of flies with the patients, and keeping flies out
of human habitations becomes imperative. Milk is a source of contagion
through contaminated water used to wash cans, or to adulterate it, or
through handling of it by patients or those who have come in contact
with patients. Oysters growing in the mouths of rivers and near the
outlets of drains and sewers are carriers of typhoid germs, and, if
eaten raw, sometimes communicate typhoid fever. Dust is an occasional
medium of communication of the germ. It is probable, however, that the
germ always enters the body by being swallowed with food or drink, and
does not enter through the lungs. There is little doubt on this point.
Ice may harbor the germ for many months, for freezing does not kill
it, and epidemics have been traced to this source. Clothing, wood,
utensils, door handles, etc., which have been contaminated by contact
with discharges from patients, may also prove mediums of communication
of the typhoid germ to healthy individuals. Typhoid germs escape from
patients sick with the disease chiefly in the bowel discharges and
urine, sometimes in the sweat, saliva, and vomited matter.
Sewer gas and emanations from sewage and filth will not communicate
typhoid fever directly, but the latter afford nutriment for the growth
of the germ, and after becoming infected, may eventually come in
contact with drinking water or food, and so prove dan[Pg 224]gerous. Improper
care of discharges of excrement and urine—with the assistance of
flies—are responsible for the enormous typhoid epidemics in military
camps, so that in the late Spanish-American War one-fifth of all our
soldiers in camp contracted the disease. In the upper layers of the
soil typhoid germs may live for six months through frosts and thaws.
The disease is preventable, and will probably be stamped out in time.
In some of the most thickly populated cities in the world, as in
Vienna, its occurrence is most infrequent, owing to intelligent
sanitary control and pure water supply, while in the most salubrious
country districts its inroads are the most serious and fatal through
ignorance and carelessness.
Development.—From eight to twenty-three days elapse from the time of
entrance of typhoid germs into the body before the patient is taken
sick. One attack usually protects one against another, but two or
three attacks are not unheard of in the same person.
Symptoms.—Typhoid fever is subject to infinite variations, and it
will here be possible only to outline what may be called a typical
case. In a work of this kind the preliminary symptoms are of most
importance in warning one of the probability of an attack, so that the
prospective patient can govern himself accordingly, as in no other
disease is rest in bed of more value. Patients who persist in walking
about with typhoid fever for the first week or so are most likely to
die of the disease.
[Pg 225]The average duration of the disease is about one month. During the
first week the onset is gradual, the temperature mounting a little
higher each day—as 99.5° F. the first evening, 101° the second, 102°
the fourth, 104° the fifth, 105° the sixth, and 105.5° the seventh. In
the morning of each day the temperature is usually about a degree or
more lower than that of the previous night. From the end of the first
week to the beginning of the third the temperature remains at its
highest point, being about the same each evening and falling one or
two degrees in the morning. During the third week the temperature
gradually falls, the highest point each evening being a degree or so
lower than the previous day, while in the fourth week the temperature
may be below normal in the morning and a degree or so above normal at
night. So much for this symptom. After the entrance of typhoid germs
into the bowels and before the recognized onset of the disease, there
may be lassitude and disinclination for exertion. The disease begins
with headache, backache, loss of appetite, sometimes a chill in adults
or a convulsion in children, soreness in the muscles, pains in the
belly, nosebleed, occasional vomiting, diarrhea, coated tongue, often
some cough, flushed face, pulse 100, gradually increasing as
described.
These symptoms are, to a considerable extent, characteristic of the
beginning of many acute diseases, but the gradual onset with constant
fever, nosebleed, and looseness of the bowels are the most sugges[Pg 226]tive
features. Then, if at the end of the first week or ten days pink-red
spots, about as large as a pin head, appear on the chest and belly to
the number of two or three to a dozen, of very numerously, and
disappear on pressure (only to return immediately), the existence of
typhoid fever is pretty certain. Headache is now intense. These rose
spots—as they are called—often appear in crops during the second and
third weeks, lasting for a few days, then departing.
During the second week there is often delirium and wandering at night;
the headache goes, but the patient is stupid and has a dusky, flushed
face. The tongue becomes brownish in color, and its coat is cracked,
and the teeth are covered with a brownish matter. The skin is
generally red and the belly distended and tender. Diarrhea is often
present with three to ten discharges daily of a light-yellow, pea-soup
nature, with a very offensive odor. Constipation throughout the
disease is, however, not uncommon in the more serious cases. The pulse
ranges from 80 to 120 a minute.
During the third week, in cases of moderate severity, the general
condition begins to improve with lowering of the temperature, clearing
of the tongue, and less frequent bowel movements. But in severe cases
the patient becomes weaker, with rapid, feeble pulse, ranging from 120
to 140; stupor and muttering delirium; twitching of the wrists and
picking at the bedclothes, with general trembling of the muscles in
mov[Pg 227]ing; slow, hesitating speech, and emaciation; while the urine and
fæces may be passed unconsciously in bed. Occasionally the patient
with delirium may require watching to prevent him from getting out of
bed and injuring himself. He may appear insane.
During the fourth week, in favorable cases, the temperature falls to
normal in the morning, the pulse is reduced to 80 or 100, the diarrhea
ceases, and natural sleep returns.
Among the many and frequent variations from the type described, there
may be a fever prolonged for five or six weeks, with a good recovery.
Chills are not uncommon during the disease, sometimes owing to
complications. Relapse, or a return of the fever and other symptoms
all over again, occurs in about ten per cent of the cases. This may
happen more than once, and as many as five relapses have been recorded
in one patient. A slight return of the fever for a day or two is often
seen, owing to error in diet, excitement, or other imprudence after
apparent recovery. Death may occur at any time from the first week,
owing to complications or the action of the poison of the disease.
Pneumonia, perforation of and bleeding from the bowels are the most
frequent dangerous complications. Unfavorable symptoms are continued
high fever (105° to 106° F.), marked delirium, and trembling of the
muscles in early stages, and bleeding from the bowels; also intense
and sudden pain with vomiting, indicating perforation of the
intestines. The result is more apt to prove un[Pg 228]favorable in very fat
patients, and especially so in persons who have walked about until the
fever has become pronounced. Bleeding from the bowels occurs in four
to six per cent of all cases and is responsible for fifteen per cent
of the deaths; perforation of the bowels happens in one to two per
cent of all cases and occasions ten per cent of the deaths.
Detection.—It is impossible for the layman to determine the existence
of typhoid fever in any given patient absolutely, but when the
symptoms follow the general course indicated above, a probability
becomes established. Unusual types are among the most difficult and
puzzling cases which a physician has to diagnose, and he can rarely be
absolutely sure of the nature of any case before the end of the first
week or ten days, when examination of the blood offers an exact method
of determining the presence of typhoid fever. Typhoid
fever—especially where there are chills—is often thought to be
malaria, when occurring in malarial regions, and may be improperly
called "typhoid malaria." There is no such disease. Rarely typhoid
fever and malaria coexist in the same person, and while this was not
uncommon in the soldiers returning from Cuba and Porto Rico, it is an
extremely unusual occurrence in the United States. Examination of the
blood will determine the presence or absence of both of these
diseases.
Complications and Sequels.—These are very numerous. Among the former
are diarrhea, delirium,[Pg 229] mental and nervous diseases, bronchitis,
pleurisy, pneumonia, ear abscess, perforation of and hemorrhage from
the bowels, inflammation of the gall bladder, disease of heart,
kidney, and bladder, and many rarer conditions, depending upon the
organ which the germ invades. Among sequels are boils, baldness, bone
disease, painful spine, and, less commonly, insanity and consumption.
While convalescence requires weeks and months, the patient often gains
greatly in flesh and feels made over anew, as in fact he has been to a
great extent, through the destruction and repair of his organs.
Outlook.—The death rate varies greatly in different epidemics and
under different conditions. During the Spanish-American War in the
enormous number of cases—over 20,000—the death rate was only about
seven per cent, which represents that in the best hospitals of this
country and in private practice. Osler states that the mortality
ranges from five to twelve per cent in private practice, and from
seven to twenty per cent in hospital practice, because hospital cases
are usually advanced before admission. The chances of recovery are
much greater in patients under fifteen years, and are also more
favorable between the twenty-second and fortieth years.
Treatment.—There is perhaps no disease in which the services of a
physician are more desirable or useful than in typhoid fever, on
account of its prolonged course and the number of complications and
incidents[Pg 230] which may occur during its existence. It is the duty of the
physician to report cases of typhoid to the health authorities, and
thus act as a guardian of the public health. If, however, in any
circumstances one should have the misfortune to have the care of a
typhoid patient remote from medical aid, it is a consolation to know
that the outlook is not greatly altered by medicine or special
treatment of any sort. There have been epidemics in remote parts of
this country where numbers of persons have suffered with typhoid
without any professional care, and yet with surprisingly good results.
Thus, in an epidemic occurring in a small community in Canada,
twenty-four persons sickened with typhoid and received no medical care
or treatment whatever, and yet there was but one death. The essentials
of treatment are comprised in Rest, Diet, and Bathing. Rest to the
extent of absolute quiet in the horizontal position, at the first
suspicion of typhoid, is requisite in order to avoid the dangers of
bleeding and perforation of the bowels resulting from ulceration of
structures weakened by the disease. The patient should be assisted to
turn in bed, must make no effort to rise during the sickness, and
should pass urine and bowel discharges into a bedpan or urinal under
cover. In case of bleeding from the bowels, the bedpan should not be
used, but the discharges may be received for a time in cloths, without
stirring the patient.
Diet.—This should consist chiefly of liquids until[Pg 231] a week after the
fever's complete disappearance. A cup of liquid should be given every
two hours except during a portion of the sleeping hours. Milk, diluted
with an equal amount of water, forms the chief food in most cases
unless it disagrees, is refused, or is unobtainable.
In addition to milk, albumen water—white of raw egg, strained and
diluted with an equal amount of water, and flavored with a few drops
of lemon juice or with brandy—is valuable; also juice squeezed from
raw beef—in doses of four tablespoonfuls—coffee, cocoa, and strained
barley, rice, or oatmeal gruel, broths, unless diarrhea is marked and
increased by the same. Soft custard, jellies, ice cream,
milk-and-flour porridge, and eggnog may be used to increase the
variety. Finely scraped raw or rare beef, very soft toast, and
soft-boiled or poached eggs are allowable after the first week of
normal temperature, at the end of the third or fourth week of the
disease, and during the course of the disease under circumstances
where the fluids are not obtainable or not well borne. An abundance of
water should be supplied to the patient throughout the disease.
Bathing.—The importance of cold, through the medium of water, in
typhoid fever accomplishes much, both in reducing the temperature and
in stimulating the nervous system and relieving restlessness and
delirium. Bathing is usually applied when the temperature rises above
102.5° F., and may be repeated every[Pg 232] two or three hours if
restlessness, delirium, and high temperature require it.
The immersion of patients in tubs of cold water, as practiced with
benefit in hospitals, is out of the question for use by inexperienced
laymen. The patient should have a woven-wire spring bed and soft hair
mattress, over which is laid a folded blanket covered by a rubber
sheet. Sponging the naked body with ice water will suffice in some
cases; in others, when the temperature is over 1021/2° F., enveloping
the whole body in a sheet wet in water at 65°, and either rubbing the
surface with ice or cloths wet in ice-cold water, for ten or fifteen
minutes, is advisable. Rubbing of the skin of the chest and sides is
necessary during the application of cold to prevent shock. The use of
a cold cloth on the head and hot-water bottle at the feet, during the
sponging, will also prove beneficial. In children and others objecting
to these cold applications, the vapor bath is effective. For this a
piece of cheese cloth (single thickness) is wet with warm water—100°
to 105°—and is wrapped about the naked body from shoulders to feet,
and is continually wet by sprinkling with water at the temperature of
98°. The evaporation of the water will usually, in fifteen to twenty
minutes, cool the body sufficiently if the patient is fanned
continuously by two attendants. In warm weather the patient should
only be covered with a sheet for a while after the bath, which should
reduce the temperature to 3°. Hot water at the feet, and a little[Pg 233]
brandy or whisky given before the sponging if the pulse be feeble,
will generally prevent a chill. Patients should be gently dried after
the bath and covered with dry bedclothing. The utmost care should be
taken not to agitate a feeble patient during sponging.
The long period of lying in bed favors the occurrence of bedsores.
These are apt to appear about the lower part of the spine, and begin
with redness of the skin, underneath which a lump may be felt.
Constant cleanliness and bathing with alcohol, diluted with an equal
amount of water, will tend to prevent this trouble, while moving the
patient so as to take the pressure off this region and avoiding any
rumpling of the bedding under his body are also serviceable, as well
as the ring air cushion. Medicine is not required, except for special
symptoms, and has no influence either in lessening the severity of or
in shortening the disease. Brandy or whisky diluted with water are
valuable in severe cases, with muttering delirium, dry tongue, and
feeble pulse; it is not usually called for before the end of the
second week, and not in mild cases at any time. A tablespoonful of
either, once in two to four hours, is commonly sufficient. Pain and
distention of the belly are relieved by applying a pad over the whole
front of the belly—consisting of two layers of flannel wrung out of a
little very hot water containing a teaspoonful of turpentine—and
covered by a dry flannel bandage wrapped about the body. Also the use
of white of egg and water, and[Pg 234] beef juice, instead of milk, will
benefit this condition.
Diarrhea—if there are more than four discharges daily—may be checked
by one-quarter level teaspoonful doses of bismuth subnitrate, or
teaspoonful doses of paregoric, once in three hours. Constipation is
relieved by injections of warm soapsuds, once in two days. Bleeding
from the bowels must be treated by securing perfect quiet on the
patient's part, and by giving lumps of ice by the mouth, and cutting
down the nourishment for six hours. Fifteen drops of laudanum should
be given to adults, if there is restlessness, and some whisky, if the
pulse becomes feeble, but it is better to reserve this until the
bleeding has stopped. Patients may be permitted to sit up after a week
of normal temperature, but solid food must not be resumed until two or
three weeks after departure of fever, and then very gradually,
avoiding all coarse and uncooked vegetables and fruit.
The greatest care must be exercised by attendants to escape
contracting the disease and to prevent its communication to others.
The bowel discharges must be submerged in milk of lime (one part of
slaked lime to four parts of water), and remain in it one hour before
being emptied. The urine should be mixed with an equal amount of the
same, or solution of carbolic acid (one part in twenty parts of hot
water), and the mixture should stand an hour before being thrown into
privy or sewer. Clothing and linen in contact with[Pg 235] the patient must
be soaked in the carbolic solution for two hours. The patient's
expectoration is to be received on old muslin pieces, which must be
burned. The bedpan and eating utensils must be frequently scalded in
boiling water. The attendant should wash his hands always after
touching the patient, or objects which have come in contact with
patient or his discharges, and thus will avoid contagion. If farm or
dairy workers come in contact with the patient, the latter precaution
is especially important. If there is no water-closet in the house, the
disinfected discharges may be buried at least 100 feet from any well
or stream. Typhoid fever is only derived from the germs escaping in
the urine, and in the bowel, nose, or mouth discharges of typhoid
patients.
MUMPS.—Mumps is a contagious disease characterized by inflammation of
the parotid glands, situated below and in front of the ears, and
sometimes of the other salivary glands below the jaw, and rarely of
the testicles in males and the breasts in females.
Swelling and inflammation of the parotid gland also occur from injury;
and as a complication of other diseases, as scarlet fever, typhoid
fever, etc.; but such conditions are wholly distinct from the disease
under discussion. Mumps is more or less constantly prevalent in most
large cities, more often in the spring and fall, and is often
epidemic, attacking ninety per cent of young persons who have not
previously had the disease. It is more common in males, affecting
chil[Pg 236]dren and youths, but rarely infants or those past middle age. One
attack usually protects against another.
Development.—A period of from one to three weeks elapses, after
exposure to the disease, before the first signs develop. The germ has
not yet been discovered, and the means of communication are unknown.
The breath has been thought to spread the germs of the disease, and
mumps can be conveyed from the sick to the well, by nurses and others
who themselves escape.
Symptoms.—Sometimes there is some preliminary discomfort before the
apparent onset. Thus, in children, restlessness, peevishness, languor,
nausea, loss of appetite, chilliness, fever, and convulsions may usher
in an attack. Mumps begins with pain and swelling below the ear on one
side. Within forty-eight hours a large, firm, sensitive lump forms
under the ear and extends forward on the face, and downward and
backward in the neck. The swelling is not generally very painful, but
gives a feeling of tightness and disfigures the patient. It makes
speaking and swallowing difficult; the patient refuses food, and talks
in a husky voice; chewing causes severe pain. After a period of two to
four days the other gland usually becomes similarly inflamed, but
occasionally only one gland is attacked. There is always fever from
the beginning. At first the temperature is about 101° F., rarely much
higher than 103° or 104°. The fever continues four[Pg 237] or five days and
then gradually declines. The swelling reaches its height in from two
to five days, and then after forty-eight hours slowly subsides, and
disappears entirely within ten to fourteen days. The patient may
communicate the disease for ten days after the fever is past, and
needs to be isolated for that period. Earache and noises in the ear
frequently accompany mumps, and rarely abscess of the ear and deafness
result. The most common complication occurs in males past puberty,
when, during recovery or a week or ten days later, one or both
testicles become painful and swollen, and this continues for as long a
time as the original mumps. Less often the breasts and sexual organs
of females are similarly affected.
Complications and Sequels.—Recovery without mishap is the usual
result in mumps, with the exception of involvement of the testicles.
Rarely there are high fever, delirium, and great prostration.
Sometimes after inflammation of both testicles in the young the organs
cease to develop, and remain so, but sexual vigor is usually retained.
Sometimes abscess and gangrene of the inflamed parotid gland occur.
Recurring swelling and inflammation of the gland may occur, and
permanent swelling and hardness remain. Meningitis, nervous and joint
complications are among the rarer sequels.
Treatment.—The patient should remain in bed while the fever lasts. A
liquid diet is advisable during this time. Fever may be allayed by
frequent[Pg 238] sponging of the naked body with tepid water. High fever and
delirium demand the constant use, on the head, of the ice cap (a
rubber bag, made to fit the head, containing ice). The relief of pain
in the swollen gland is secured by the frequent application of a thick
layer of sheet cotton, large enough to cover the whole side of the
neck, wrung out of hot water and covered with oil-silk or rubber
sheeting, with a bandage to retain it in place.
Paregoric may be given for the same purpose—a tablespoonful for
adults; a teaspoonful for a child of eight to ten, well diluted with
water, and not repeated inside of two hours, and not then unless the
pain continues unabated. Inflammation of the testicles demands rest in
bed, elevation of the testicle on a pillow after wrapping it in a
thick layer of absorbent cotton, or applying hot compresses, as
recommended for the neck. After the first few days of this treatment,
adjust a suspensory bandage, which can be procured at any apothecary
shop, and apply daily the following ointment: guiacol, sixty grains;
lard, one-half ounce, over the swollen testicle.
WHOOPING COUGH.—A contagious disease characterized by fits of
coughing, during which a whooping or crowing sound is made following a
long-drawn breath. Whooping cough is generally taken through direct
contact with the sick, rarely through exposure to the sick room, or to
persons or clothing used by the sick. The germ which causes the
disease[Pg 239] is probably in the mucus of the nose and throat. Whooping
cough is usually more or less prevalent in all thickly settled
civilized communities, at times is epidemic, and often follows
epidemics of measles. It occurs chiefly in children from six months to
six years of age. Girls and all weak and delicate subjects are
slightly more susceptible to the disease. Some children are naturally
immune to whooping cough. One attack usually protects against another.
Development.—A variable period elapses between the time of exposure
to whooping cough and the appearance of the first symptoms. This may
be from two days to two weeks; usually seven to ten days.
Symptoms.—Whooping cough begins like an ordinary cold in the head,
with cough, worse at night, which persists. The coughing fits increase
and the child gets red in the face, has difficulty in getting its
breath during them, and sometimes vomits when the attack is over.
After a variable period, from a few days to two weeks from the
beginning of the cough, the peculiar feature of the disease appears.
The child gives fifteen or twenty short coughs without drawing breath,
the face swells and grows blue, the eyeballs protrude, the veins stand
out, and the patient appears to be suffocating, when at last he draws
in a long breath with a crowing or whooping sound, which gives rise to
the name of the disease. Several such fits of coughing may follow one
another and are often succeeded by vomiting and the expulsion of a
large[Pg 240] amount of phlegm or mucus, which is sometimes streaked with
blood. In mild cases there may be six to twelve attacks in twenty-four
hours; in severe cases from forty to eighty. The attacks last from a
few seconds to one or two minutes. Occasionally the whoop comes before
the coughing fit, and sometimes there may be no whooping at all, only
fits of coughing with vomiting. Between the attacks, puffiness of the
face and eyes and blueness of the tongue persist. The coughing fits
and whooping last usually from three to six weeks, but the duration of
the disease is very variable. Occasionally it lasts many months,
especially when it occurs in winter. The contagiousness of whooping
cough continues about two months, or ceases before that time with the
cessation of the cough. Oftentimes there may be occasional whooping
for months; or, after ceasing altogether for some days, it may begin
again. In neither of these conditions is the disease considered still
contagious after two months. When an attack of whooping is coming on,
the child often seems to have some warning, as he seems terrified and
suddenly sits up in bed, or, if playing, grasps hold of something, or
runs to his mother or nurse. Coughing fits are favored by emotion or
excitement, by crying, singing, eating, drinking, sudden change of
temperature, and by bad air.
Complications and Sequels.—These are many and make whooping cough a
critical disease for very young children. Bronchitis and pneumonia
often compli[Pg 241]cate whooping cough in winter, and diarrhea frequently
occurs with it in summer. Convulsions not infrequently follow the
coughing fits in infants, and, owing to the amount of blood forced to
the head during the attacks, nosebleed and dark spots on the forehead
and surface of the eyes appear from breaking of small blood vessels in
these places. Severe vomiting and diarrhea occasionally aggravate the
case, and pleurisy and consumption may occur. The violent coughing may
permanently damage the heart. Rupture of the lung tissue happens from
the same cause, and paralysis sometimes follows breaking of a blood
vessel in the brain. But in the vast majority of cases in children
over two years old no dangerous sequel need be feared.
Outlook.—Owing to the numerous complications, whooping cough must be
looked upon as a very serious disease, especially in infants under two
years, and in weak, delicate children. It causes one-fourth of all
deaths among children, the death rate varying from three to fifteen
per cent in different times and under different circumstances. For
this reason a physician's services should always be secured when
possible.
Treatment.—A host of remedies is used for whooping cough, but no
single one is always the best. It is often necessary to try different
medicines till we find one which excels. Fresh air is of greatest
importance. Patients should be strictly isolated in rooms by
themselves, and it is wise to send away children[Pg 242] who have not been
exposed. Morally, parents are criminally negligent who allow their
children with whooping cough to associate with healthy children. If
the coughing fits are severe or there is fever, children should be
kept in bed. Usually there is not much fever; perhaps an elevation of
a degree or two at first, and at times during the disease. Otherwise,
children may be outdoors in warm weather, and in winter on warm, quiet
days. Sea air is especially good for them. It is best that the sick
should have two rooms, going from one to the other, so that the
windows in the room last occupied may be opened and well ventilated.
Fresh air at night is especially needful, and the patient should sleep
in a room which has been freshly aired. The temperature should be kept
at an even 70° F., and the child should not be exposed to draughts.
Vaporizing antiseptics in the sick room has proved beneficial. A two
per cent solution of carbolic acid in water is useful for this
purpose, or a substance called vapo-cresoline, with which is sold a
vaporizing lamp and directions for use. A one per cent solution of
resorcin, or of hydrogen dioxide, diluted with four parts of water,
used in an atomizer for spraying the throat, every two hours, has
given good results. In the beginning of the disease, before the
whooping has begun, a mixture of paregoric and syrup of ipecac will
relieve the cough, ten drops of the former with five of the latter,
for a child of two years, given together in water every three hours.
The bromide of sodium, five[Pg 243] grains in water, every three hours during
the day, for a child of two, is serviceable in relieving the fits of
coughing in the day; while at night, two grains of chloral, not
repeated, may be given in water at bedtime to secure sleep, in a child
of two. The tincture of belladonna, in doses of two drops in water,
three times daily, for a child of two, is also often efficacious.
Quinine, given in the dose of one-sixth grain for each month of the
child's age under a year; or in one and one-half grain doses for each
year of age under five, is one of the older and more valuable
remedies. It should be given three times daily in pill with jelly, or
solution in water. Bromoform in doses of two drops for a child of two,
and increasing to five drops for a child of six, may be given in syrup
three times daily with benefit. Most of these drugs should be employed
only with a doctor's advice, when this is possible. To sum up, use the
vapo-cresoline every day. When no physician is available, begin with
belladonna during the day, using bromide of sodium at night. If this
fails to modify the whooping after five days' trial, use bromide and
chloral. In severe cases use bromoform. During a fit of coughing and
whooping, it is well to support the child's head, and if he ceases to
breathe, he should be slapped over the face and chest with a towel wet
with cold water. Interference with sleep caused by coughing, and loss
of proper nourishment through vomiting, lead to wasting and debility.
Teaspoonful doses of emulsion of cod-liver oil[Pg 244] three times daily,
after eating, are often useful in convalescence, and great care must
be taken at this time to prevent exposure and pneumonia. Change of air
and place will frequently hasten recovery remarkably in the later
stages of the disease.
ERYSIPELAS.—Erysipelas is a disease caused by germs which gain
entrance through some wound or abrasion in the skin or mucous
membranes. Even where no wound is evident it may be taken for granted
that there has been some slight abrasion of the surface, although
invisible. Erysipelas cannot be communicated any distance through the
air, but it is contagious in that the germs which cause it may be
carried from the sick to the well by nurses, furniture, bedding,
dressings, clothing, and other objects. Thus, patients with wounds,
women in childbirth, and the newborn may become affected, but modern
methods of surgical cleanliness have largely eliminated these forms of
erysipelas, especially in hospitals, where it used to be common.
Erysipelas attacks people of all ages, some persons being very
susceptible and suffering frequent recurrences. The form which arises
without any visible wound is seen usually on the face, and occurs most
frequently in the spring. The period of development, from the time the
germs enter the body until the appearance of the disease, lasts from
three to seven days.
Erysipelas begins with usually a severe chill (or convulsion in a
baby) and fever. Vomiting, head[Pg 245]ache, and general lassitude are often
present. A patch of red appears on the cheeks, bridge of nose, or
about the eye or nostril, and spreads over the face. The margins of
the eruption are sharply defined. Within twenty-four hours the disease
is fully developed; the skin is tense, smooth, and shiny, scarlet and
swollen, and feels hot, and is often covered with small blisters. The
pain is more or less intense, burning or itching occurs, and there is
a sensation of great tightness or tension. On the face the swelling
closes the eye and may interfere with breathing through the nose. The
lips, ears, and scalp are swollen, and the person may become
unrecognizable in a couple of days. Erysipelas tends to spread like a
drop of oil, and the borders of the inflammatory patch are well
marked. It rarely spreads from the face to the chest and body, and but
occasionally attacks the throat. During the height of the inflammation
the temperature reaches 104° F, or over. After four or five days, in
most cases, erysipelas begins to subside, together with the pain and
temperature, and recovery occurs with some scaling of the skin. The
death rate is said to average about ten per cent in hospitals, four
per cent in private practice. Headache, delirium, and stupor are
common when erysipelas attacks the scalp. The appearance of the
disease in other locations is similar to that described. Relapses are
not uncommon, but are not so severe as the original attack. Spreading
may extend over a large area, and the deeper parts may become
affected,[Pg 246] with the formation of deep abscesses and great destruction
of tissue. Certain internal organs, heart, lungs, spleen, and kidneys,
are occasionally involved with serious consequences. The old, the
diseased, and the alcoholic are more apt to succumb, also the newborn.
It is a curious fact that cure of malignant growths (sarcoma), chronic
skin diseases, and old ulcers sometimes follows attacks of erysipelas.
Treatment.—The duration of erysipelas is usually from a few days to
about two weeks, according to its extent. It tends to run a definite
course and to recovery in most cases without treatment. The patient
must be isolated in a room with good ventilation and sunlight.
Dressings and objects coming in contact with him must be burned or
boiled. The diet should be liquid, such as milk, beef tea, soups, and
gruels. The use of cloths wet constantly with cold water, or with a
cold solution of one-half teaspoonful of pure carbolic acid to the
pint of hot water, or with a poisonous solution of sugar of lead, four
grains to the pint, should be kept over small inflamed areas. Fever is
reduced by sponging the whole naked body with cold water at frequent
intervals. A tablespoonful of whisky or brandy in water may be given
every two hours to adults if the pulse is weak. Painting the borders
of the inflamed patch with contractile collodion may prevent its
spreading. The patient must be quarantined until all scaling ceases,
usually for two weeks.
[Pg 247]
CHAPTER III
Malaria and Yellow Fever
The Malarial Parasite—Mosquitoes the Means of Infection—Different
Forms of Malaria—Symptoms and Treatment—No Specific for Yellow
Fever.
MALARIA; CHILLS AND FEVER; AGUE; FEVER AND AGUE; SWAMP OR MARSH FEVER;
INTERMITTENT OR REMITTENT FEVER; BILIOUS FEVER.—Malaria is a
communicable disease characterized by attacks of fever occurring at
certain intervals, and due to a minute animal parasite which inhabits
the body of the mosquito, and is communicated to the blood of man by
the bites of this insect.
In accordance with this definition malaria is not a contagious disease
in the sense that it is acquired by contact with the sick, which is
not the case, but it is derived from contact with certain kinds of
mosquitoes, and can be contracted in no other way, despite the many
popular notions to the contrary. Mosquitoes, in their turn, acquire
the malarial parasite by biting human beings suffering from malaria.
It thus becomes possible for one malarial patient, coming to a region
hitherto free from the disease, to infect the whole[Pg 248] district with
malaria through the medium of mosquitoes.
Causes.—While the parasite infesting mosquitoes is the only direct
cause of malaria, yet certain circumstances are requisite for the life
and growth of the mosquitoes. These are moisture and proper
temperature, which should average not less than 60° F. Damp soil,
marshes, or bodies of water have always been recognized as favoring
malaria.
Malaria is common in temperate climates—in the summer and autumn
months particularly, less often in spring, and very rarely in winter,
while it is prevalent in the tropics and subtropics all the year
round, but more commonly in the spring and fall of these regions. The
older ideas, that malaria was caused by something arising in vapors
from wet grounds or water, or by contamination of the drinking water,
or by night air, or was due to sleeping outdoors or on the ground
floors of dwellings, are only true in so far as these favor the growth
of the peculiar kind of mosquitoes infected by the malarial parasites.
Two essentials are requisite for the existence of malaria in a region:
the presence of the particular mosquito, and the actual infection of
the mosquito with the malarial parasite. The kind of mosquito acting
as host to the malarial parasite is the genus Anopheles, of which
there are several species. The more common house mosquito of the
United States is the Culex. The Anopheles can usually be
distinguished from the latter[Pg 249] by its mottled wings, and, when on a
wall or ceiling, it sits with the body protruding at an angle of 45°
from the surface, with its hind legs hanging down or drawn against the
wall. In the case of the Culex, the body is held parallel with the
wall, the wings are usually not mottled, and the hind legs are carried
up over the back.
When a mosquito infected with the malarial parasite bites man, the
parasite enters his blood along with the saliva that anoints the
lancet of the mosquito. The parasite is one of the simplest forms of
animal life, consisting of a microscopical mass of living, motile
matter which enters the red-blood cell of man, and there grows,
undergoes changes, and, after a variable time, multiplies by dividing
into a number of still smaller bodies which represent a new generation
of young parasites. This completes the whole period of their
existence. It is at that stage in the development of the parasite in
the human body when it multiplies by dividing that the chills and
fever in malaria appear. What causes the malarial attack at this point
is unknown, unless it be that the parasites give rise to a poison at
the time of their division. Between the attacks of chills and fever in
malaria there is usually an interval of freedom of a few hours, which
corresponds to the period intervening in the life of the parasite in
the human body, between the birth of the young parasites and their
growth and final division, in turn, into new individuals. This
interval varies with the kind of parasite. The common form of malaria
is caused by a parasite re[Pg 250]quiring forty-eight hours for its
development. The malarial attacks caused by this parasite then occur
every other day, when the parasite undergoes reproduction by division.
However, an attack may occur every day when there are two separate
groups of these parasites in the blood, the time of birth of one set
of parasites, with an accompanying malarial attack, happening one day;
that of the other group coming on the next, so that between the two
there is a daily birth of parasites and a daily attack of malaria. In
cases of malaria caused by one group of parasites the attacks appear
at about the same time of day, but when the attacks are caused by
different groups of parasites the times of attack may vary on
different days. In the worst types of malaria the parasites do not all
go through the same stages of development at the same time, as is
commonly the case in the milder forms prevalent in temperate regions,
so that the fever—corresponding to the stage of reproduction of the
parasites—occurs at irregular intervals.
In a not uncommon type of malaria the attacks occur every third day,
with two days of intermission or freedom from fever. Different groups
of parasites causing this form of malaria, and having different times
of reproduction, may inhabit the same patient and give rise to
variation in the times of attack. Thus, an attack may occur on two
successive days with a day of intermission.
The reproduction of the parasite in the human[Pg 251] blood is not a sexual
reproduction; that takes place in the body of the mosquito.
When a healthy mosquito bites a malarial patient, the parasite enters
the body of the mosquito with the blood of the patient bitten. It
enters its stomach, where certain differing forms of the parasite,
taking the part of male and female individuals, unite and form a new
parasite, which, entering the stomach wall of the mosquito, gives
birth in the course of a week to innumerable small bodies as their
progeny. These find their way into the salivary glands which secrete
the poison of the mosquito bite, and escape, when the mosquito bites a
human being, into the blood of the latter and give him malaria.
Distribution.—Malaria is very widely distributed, and is much more
severe in tropical countries and the warmer parts of temperate
regions. In the United States malaria is prevalent in some parts of
New England, as in the Connecticut Valley, and in the course of the
Charles River, in the country near Boston. It is common in the
vicinity of the cities of Philadelphia, New York, and Baltimore, but
here is less frequent than formerly, and is of a comparatively mild
type. More severe forms prevail along the Gulf of Mexico and the
shores of the Mississippi and its branches, especially in Mississippi,
Texas, Louisiana, and Arkansas, but even here it is less fatal and
widespread than formerly. In Alaska, the Northwest, and on the Pacific
Coast of the United States malaria is almost unknown,[Pg 252] while it is but
slightly prevalent in the region of the Great Lakes, as about Lakes
Erie and St. Clair.
Development.—Usually a week or two elapses after the entrance of the
malarial parasite into the blood before symptoms occur; rarely this
period is as short as twenty-four hours, and occasionally may extend
to several months. It often happens that the parasite remains
quiescent in the system without being completely exterminated after
recovery from an attack, only to grow and occasion a fresh attack, a
month or two after the first, unless treatment has been thoroughly
prosecuted for a sufficient time.
Symptoms.—Certain symptoms give warning of an attack, as headache,
lassitude, yawning, restlessness, discomfort in the region of the
stomach, and nausea or vomiting. The attack begins with a chilliness
or creeping feeling, and there may be so severe a chill that the
patient is violently shaken from head to foot and the teeth chatter.
Chills are not generally seen in children under six, but an attack
begins with uneasiness, the face is pinched, the eyes sunken, the lips
and tips of the fingers and toes are blue, and there is dullness and
often nausea and vomiting. Then, instead of a chill, the eyelids and
limbs begin to twitch, and the child goes into a convulsion. While the
surface of the skin is cold and blue during a chill, yet the
temperature, taken with the thermometer in the mouth or bowel, reaches
102°, 105°, or 106° F., often. The chill lasts from a few minutes to
an hour, and[Pg 253] as it passes away the face becomes flushed and the skin
hot. There is often a throbbing headache, thirst, and sometimes mild
delirium. The temperature at this time, when the patient feels
intensely feverish, is very little higher than during the chill. The
fever lasts during three or four hours, in most cases, and gradually
declines, as well as the headache and general distressing symptoms
with the onset of sweating, to disappear in an hour or two, when the
patient often sinks into a refreshing sleep. Such attacks more
commonly occur every day, every other day, or after intermissions of
two days. Rarely do attacks come on with intervals of four, five, six,
or more days. The attacks are apt to recur at the same time of day as
in the first attack. In severe cases the intervals may grow shorter,
in mild cases, longer. In the interval between the attacks the patient
usually feels well unless the disease is of exceptional severity.
There is also entire freedom from fever in the intervals except in the
grave types common to hot climates. Frequently the chill is absent,
and after a preliminary stage of dullness there is fever followed by
sweating. This variety is known as "dumb ague."
Irregular and Severe Form—Chronic Malaria.—This occurs in those who
have lived long in malarial regions and have suffered repeated attacks
of fever, or in those who have not received proper treatment. It is
characterized by a generally enfeebled state, the patient having a
sallow complexion, cold[Pg 254] hands and feet, and temperature below normal,
except occasionally, when there may be slight fever. When the
condition is marked, there are breathlessness on slight exertion,
swelling of the feet and ankles, and "ague cake," that is, enlargement
of the spleen, shown by a lump felt in the abdomen extending downward
from beneath the ribs on the left side.
Among unusual forms of malaria are: periodic attacks of drowsiness
without chills, but accompanied by slight fever (100° to 101° F.);
periodic attacks of neuralgia, as of the face, chest, or in the form
of sciatica; periodic "sick headaches." These may take the place of
ordinary malarial attacks in malarial regions, and are cured by
ordinary malarial treatment.
Remittent Form (unfortunately termed "bilious").—This severe type of
malaria occurs sometimes in late summer and autumn, in temperate
climates, but is seen much more commonly in the Southern United States
and in the tropics. It begins often with lassitude, headache, loss of
appetite and pains in the limbs and back, a bad taste, and nausea for
a day or two, followed by a chill, and fever ranging from 101° to 103°
F., or more. The chill is not usually repeated, but the fever is
continuous, often suggesting typhoid fever. With the fever, there are
flushed face, occasional delirium, and vomiting of bile, but more
often a drowsy state. After twelve to forty-eight hours the fever
abates, but the temperature does not usually fall below 100° F., and
the patient feels better, but not[Pg 255] entirely well, as in the ordinary
form of malaria, where the fever disappears entirely between the
attacks. After an interval varying from three to thirty-six hours the
temperature rises again and the more severe symptoms reappear, and so
the disease continues, there never being complete freedom from fever,
the temperature sometimes rising as high as 105° or 106° F. In some
cases there are nosebleed, cracked tongue, and brownish deposit on the
teeth, and a delirious or stupid state, as in typhoid fever, but the
distention of the belly, diarrhea, and rose spots are absent. The skin
and whites of the eyes often take on the yellowish hue of jaundice.
This fever has been called typhomalarial fever, under the supposition
that it was a hybrid of the two. This is not the case, although it is
possible that the two diseases may occur in the same individual at the
same time. This, indeed, frequently happened as stated, in our
soldiers coming from the West Indies during the Spanish-American
War—but is an extremely uncommon event in the United States.
Pernicious Malaria.—This is a very grave form of the disease. It
rarely is seen in temperate regions, but often occurs in the tropics
and subtropics. It may follow an ordinary attack of chills and fever,
or come on very suddenly. After a chill the hot stage appears, and the
patient falls into a deep stupor or unconscious state, with flushed
face, noisy breathing, and high fever (104° to 105° F.). Wild delirium
or convul[Pg 256]sions afflict the patient in some cases. The attack may last
for six to twenty-four hours, from which the patient may recover, only
to suffer another like seizure, or he may die in the first. In another
form of this pernicious malaria the symptoms resemble true cholera,
and is peculiar to the tropics. In this there are violent vomiting,
watery diarrhea, cramps in the legs, cold hands and feet, and
collapse. Sometimes the attack begins with a chill, but fever, if any,
is slight, although the patient complains of great thirst and inward
heat. The pulse is feeble and the breathing shallow, but the intellect
remains clear.
Death often occurs in this, as in the former type of pernicious
malaria, yet vigorous treatment with quinine, iron, and nitre will
frequently prove curative in either form.
Black Water Fever.—Rarely in temperate climates, but frequently in
the Southern United States and in the tropics, especially Africa;
after a few days of fever, or after chilliness and slight fever, the
urine becomes very dark, owing to blood escaping in it. This sometimes
appears only periodically, and is often relieved by quinine. It is
apparently a malarial fever with an added infection from another
cause.
Chagres Fever.—A severe form of malarial fever acquired on the
Isthmus of Panama, apparently a hemorrhagic form of the pernicious
variety, and so treated.
Detection.—To the well-educated physician is now open an exact method
of determining the existence of[Pg 257] malaria, and of distinguishing it
from all similar diseases, by the examination of the patient's blood
for the malarial parasite—its presence or absence deciding the
presence or absence of the disease. For the layman the following
points are offered: intermittency of chills and fever, or of fever
alone, should suggest malaria, particularly in a patient living in or
coming from a malarial region, or in a previous sufferer from the
disease. In such a case treatment with quinine will solve the doubt in
most cases, and will do no harm even if the disease be not malaria.
Malaria is one of the few diseases which can be cured with certainty
by a drug; failure to stop the symptoms by proper amounts of quinine
means, in the vast majority of cases, that they are not due to
malaria. There are many other diseases in which chills, fever, and
sweating occur at intervals, as in poisoning from the presence of
suppuration or formation of pus anywhere in the body, but the layman's
ignorance will not permit him to recognize these in many instances.
The quinine test is the best for him.
Prevention.—Since the French surgeon, Laveran, discovered the
parasite of malaria in 1880, and Manson, in 1896, emphasized the fact
that the mosquito is the medium of its communication to man, the way
for the extermination of the disease has been plain. "Mosquito
engineering" has attained a recognized place. This consists in
destroying the abodes of mosquitoes (marshes, ponds, and pools) by
drainage and filling, also in the application of petroleum on their
sur[Pg 258]face to destroy the immature mosquitoes. Such work has already led
to wonderful results.[11] Open water barrels and water tanks prove a
fruitful breeding place for these insects, and should be abolished.
The protection of the person from mosquito bites is obtained by proper
screening of habitations and the avoidance of unscreened open air, at
or after nightfall, when the pests are most in evidence. Dwellings on
high grounds are less liable to mosquitoes. Persons entering a
malarial region should take from two to three grains of quinine three
times a day to kill any malarial parasites which may invade their
blood, and should screen doors and windows. Patients after recovery
from malaria must prolong the treatment as advised, and renew it each
spring and fall for several years thereafter. A malarial patient is a
direct menace to his entire neighborhood, if mosquitoes enter.
Treatment.—The treatment of malaria practically means the use of
quinine given in the proper way and in the proper form and dose.
Despite popular prejudices against it, quinine is capable of little
harm, unless used in large doses for months, and no other remedy has
yet succeeded in rivaling it in any way. Quinine is frequently useless
from adulteration; this may be avoided by getting it of a reliable
drug house and paying a fair price for the best to be had. Neither
pills nor tablets of quinine are suitable, as they sometimes pass
through the bowels undissolved. The drug should[Pg 259] be taken dissolved in
water, or, more pleasantly, in starch wafers or gelatin capsules. When
the drug is vomited it may be given (in double the dose) dissolved in
half a pint of water, as an injection into the bowels, three times
daily. Infants of a few months may be treated by rubbing an ointment
(containing thirty grains of quinine sulphate mixed with an ounce and
a half of lard) well into the skin of the armpits and groins, night
and morning. Children under the age of two can be best treated by
quinine made into suppositories—little conical bodies of cocoa butter
containing two grains each—one being introduced into the bowel, night
and morning.
During an attack of malaria the discomfort of the chill and fever may
be relieved to considerable extent by thirty grains of sodium bromide
(adult dose) in water. Hot drinks and hot-water bottles with warm
covering may be used during the chill, while cold sponging of the
whole naked body will afford comfort during the hot stage. In the
pernicious form, attended with unconsciousness, sponging with very
cold water, or the use of the cold bath with vigorous friction of the
whole body and cold to the head are valuable. The effect of quinine is
greatest during the time of birth of a new generation of young
parasites in the blood, which corresponds with the time of the
malarial attack. But in order that the quinine shall have time to
permeate the blood, it must be given two to four hours before the
expected chill, and then will probably prevent[Pg 260] the next attack but
one. A dose of ten grains of quinine sulphate taken three times daily
for the first three days of treatment; then a dose of three grains,
three times daily for two weeks; and finally two grains, three times
daily for the rest of the month of treatment will, in many cases,
complete a cure. If the quinine cause much ringing in the ears and
deafness, it will be found that sodium bromide taken with the quinine
(in twice the dose) dissolved in water, will correct this trouble. If
the patient is constipated and the bowel discharges are light colored,
a few one-quarter grain doses of calomel may be taken every two hours,
and followed in twelve hours by a dose of Epsom salts, on the first
day of treatment, with quinine. It is no use to take quinine by the
mouth later than two hours before an attack, and if the patient cannot
secure treatment before this time, he should take a single dose of
twenty grains of quinine.
To children may be given a daily amount of quinine equal to one grain
for each year of their age. In the severe forms of remittent and
pernicious types of malaria it may be necessary for the patient to
take as much as thirty grains of quinine every three days or so to cut
short the attack. But, unfortunately, the digestion may be so poor
that absorption of the drug does not occur, and in such an event the
use of quinine in the form of the bisulphate in thirty-grain doses,
with five grains of tartaric acid, will in some cases prove effective.
Chronic malaria is best treated[Pg 261] with small doses of quinine, together
with arsenic and iron. A capsule containing two grains of quinine
sulphate, one-thirtieth grain of arsenious acid, and two grains of
reduced iron should be taken three times daily for several weeks.
YELLOW FEVER.—This is a disease of tropical and subtropical countries
characterized by fever, jaundice, and vomiting (in severe cases
vomiting of blood), caused by a special germ or parasite which is
communicated to man solely through the agency of the bites of a
special mosquito, Stegomyia fasciata.
Distribution.—Yellow fever has always been present in Havana, Rio,
Vera Cruz, and other Spanish-American seaports; also on the west coast
of Africa. It is frequently epidemic in the tropical ports of the
Atlantic in America and Africa, and there have been numerous epidemics
in the southern and occasional ones in the northern seacoast cities of
the United States. The last epidemic occurred in the South in 1899.
Rarely has the disease been introduced into Europe, and it has never
spread there except in Spanish ports. The disease is one requiring
warm weather, for a temperature under 75° F. is unsuitable to the
growth of the special mosquito harboring the yellow-fever parasite. It
spreads in the crowded and unsanitary parts of seacoast cities, to
which it is brought on vessels by contaminated mosquitoes or
yellow-fever patients from the tropics. Havana has heretofore been the
source of infection for the United States, but[Pg 262] since the disease has
been eradicated by the American army of occupation, that danger has
been removed. Yellow fever is not at all contagious in the sense that
a healthy person can contract the disease by contact with a
yellow-fever patient, or with his discharges from the stomach, bowels,
or elsewhere, and is probably only communicated to man by the bite of
a particular kind of mosquito harboring the yellow-fever organism in
its body. Both these facts have been incontestably proved,[12] in part
by brave volunteers from the United States Army who submitted to sleep
for twenty-one days on clothes soiled with discharges from patients
dying of yellow fever, and escaped the disease; and by others living
in uncontaminated surroundings who permitted themselves to be bitten
by infected mosquitoes and promptly developed yellow fever.
Development.—After a person has been bitten by an infected mosquito,
from fourteen hours to five days and seventeen hours elapse before the
development of the first symptoms—usually this period lasts from
three to four days. With the appearance of a single case in a region,
a period of two weeks must elapse before the development of another
case arising from the first one. This follows because a mosquito,
after biting a patient, cannot communicate the germ to another person
for twelve days, and two days more must elapse before the disease
appears in the latter.
Symptoms.—During the night or morning the pa[Pg 263]tient has a chill (or
feels chilly) and experiences discomfort in the stomach, with
sometimes nausea and vomiting. There is pain through the forehead and
eyes, in the back and thighs, and often in the calves. The face is
flushed and slightly swollen—particularly the upper lip—and the eyes
are bloodshot, and gradually, in the course of thirty-six hours, the
whites become yellowish. This is one of the most distinguishing
features of the fever, but is often absent in children. The tongue is
coated, there are loss of appetite, lassitude, sore throat, and
constipation. In the beginning the temperature ranges from 101° to
103° F., or in severe cases as high as 105° or 106° F., and the pulse
from 110 to 120 beats a minute. The fever continues for several
days—except in mild cases—but the pulse usually falls before the
temperature does. For example, the temperature may rise a degree
during the third day to 103° F., while the pulse falls ten or more
beats at the same time and may not be over 70 or 80, while the
temperature is still elevated. This is another peculiar feature of the
disease. Vomiting often increases on the second or third day, and the
dreaded "black vomit" may then occur. This presents the appearance of
coffee grounds or tarry matter and, while a dangerous symptom, does
not by any means presage a fatal ending. The black color is due to
altered blood from the stomach, and bleeding sometimes takes place
from the nose, throat, gums, and bowels, with black discharges from
the latter. The[Pg 264] action of the kidneys is usually interfered with,
causing diminution in the amount of urine. It is extremely important
to pay regard to this feature, because failure of the patient to pass
a proper amount of urine calls for prompt action to avert fatal
poisoning from retained waste matters in the blood. The normal amount
of urine passed in twenty-four hours in health is over three pints,
and while not more than two-thirds of this amount could be expected to
be passed by a fever patient, yet in yellow fever the passage of urine
may be almost or wholly suppressed. The course of the disease varies
greatly. In children—especially of the Creoles—it is frequently so
mild as to pass unnoticed. In adults the fever may only last a few
hours, or two or three days, with gradual recovery from the various
symptoms, and yellowness of the skin lasting for some time. This is
not seen readily during the stage of fever when the surface is
reddened, but at that time may be detected by pressure on the skin for
a minute, when the skin will present a yellow hue on removing the
finger before the blood returns to the pressure spot. With fall of
fever, and abatement of symptoms after two or three days, the patient,
instead of going on to recovery may, after a few hours or a day or
two, again become very feverish and have vomiting—perhaps of blood or
black vomit—yellow skin, feeble pulse, failure of kidney action with
suppression of urine, delirium, convulsions, stupor, and death; or may
begin to again recover after a few days. Mild fever, slight[Pg 265] jaundice,
and absence of bleeding are favorable signs; black vomit, high fever,
and passage of little urine are unfavorable signs. The death rate is
very variable in different epidemics and among different classes;
anywhere from fifteen to eighty-five per cent. Among the better
classes it is often not greater than ten per cent in private practice.
Heavy drinkers and those living in unfavorable surroundings are apt to
succumb.
Prevention.—Yellow fever, like malaria, is a preventable disease, and
will one day be only a matter of historic interest. Dr. W. C. Gorgas,
U. S. A., during 1901, by ridding Havana of the mosquito carrying the
yellow-fever organism through screening barrels and receptacles
holding water, and by treating drains, cesspools, etc., with kerosene,
succeeded in also eradicating yellow fever from that city, so that in
the following year there was not one death from this disease; whereas,
before this time, the average yearly mortality had been 751 deaths in
Havana. Spread of the disease is controlled by preventing access of
mosquitoes to the bodies of living or dead yellow-fever patients;
while personal freedom from yellow fever may be secured by avoiding
mosquito bites, through protection by screens indoors, and covering
exposed parts of the face, hands, and ankles with oil of pennyroyal or
spirit of camphor, while outdoors.
Treatment.—There is unfortunately no special cure known for yellow
fever such as we possess in malaria. The patient should be well
covered and sur[Pg 266]rounded with hot-water bags during chill. It is
advisable to give a couple of compound cathartic pills or a
tablespoonful of castor oil at the start. Two, or at most three,
ten-grain doses of phenacetin at three hours intervals will relieve
the pain during the early stage. Cracked ice given frequently by the
mouth and the application of a mustard paper or paste (one part
mustard, three parts flour, mixed with warm water and applied between
two layers of thin cotton) over the stomach will serve to allay
vomiting. Cold sponging (see Typhoid Fever, p. 232) is the best
treatment for fever. The black vomit may be arrested by one-quarter
teaspoonful doses of tincture of the chloride of iron, given in four
tablespoonfuls of water, every hour after vomiting. The bowels should
be moved daily by injection of warm soapsuds. The patient should not
rise from his bed, but should use a bedpan or other receptacle. In
addition, a pint of warm water, containing one-half teaspoonful of
salt, should be injected into the bowel night and morning and, if
possible, retained by the patient. The object of the latter is by its
absorption to stimulate the action of the kidneys. The diet should
consist of milk, diluted with an equal amount of water, broths,
gruels, etc., and only soft food should be given for ten days after
recovery. Iced champagne in tablespoonful doses at frequent intervals,
or two teaspoonful doses of whisky in a little ice water, given every
half hour, relieves vomiting and supports the strength.
TRANSCRIBER'S NOTE.
The following change was made:
Part II, Chapter II, Typhoid Fever, Symptoms (p. 225)
Original text:
"... flushed face, pulse 100°, gradually increasing as described."
Changed to:
"... flushed face, pulse 100, gradually increasing as described."
"Pulse 100" was preferred over "temperature 100°".
End of the Project Gutenberg EBook of The Home Medical Library, Volume I (of
VI), by Various
*** END OF THIS PROJECT GUTENBERG EBOOK THE HOME MEDICAL LIBRARY ***
***** This file should be named 27943-h.htm or 27943-h.zip *****
This and all associated files of various formats will be found in:
http://www.gutenberg.org/2/7/9/4/27943/
Produced by Juliet Sutherland, Chris Logan and the Online
Distributed Proofreading Team at http://www.pgdp.net
Updated editions will replace the previous one--the old editions
will be renamed.
Creating the works from public domain print editions means that no
one owns a United States copyright in these works, so the Foundation
(and you!) can copy and distribute it in the United States without
permission and without paying copyright royalties. Special rules,
set forth in the General Terms of Use part of this license, apply to
copying and distributing Project Gutenberg-tm electronic works to
protect the PROJECT GUTENBERG-tm concept and trademark. Project
Gutenberg is a registered trademark, and may not be used if you
charge for the eBooks, unless you receive specific permission. If you
do not charge anything for copies of this eBook, complying with the
rules is very easy. You may use this eBook for nearly any purpose
such as creation of derivative works, reports, performances and
research. They may be modified and printed and given away--you may do
practically ANYTHING with public domain eBooks. Redistribution is
subject to the trademark license, especially commercial
redistribution.
*** START: FULL LICENSE ***
THE FULL PROJECT GUTENBERG LICENSE
PLEASE READ THIS BEFORE YOU DISTRIBUTE OR USE THIS WORK
To protect the Project Gutenberg-tm mission of promoting the free
distribution of electronic works, by using or distributing this work
(or any other work associated in any way with the phrase "Project
Gutenberg"), you agree to comply with all the terms of the Full Project
Gutenberg-tm License (available with this file or online at
http://gutenberg.org/license).
Section 1. General Terms of Use and Redistributing Project Gutenberg-tm
electronic works
1.A. By reading or using any part of this Project Gutenberg-tm
electronic work, you indicate that you have read, understand, agree to
and accept all the terms of this license and intellectual property
(trademark/copyright) agreement. If you do not agree to abide by all
the terms of this agreement, you must cease using and return or destroy
all copies of Project Gutenberg-tm electronic works in your possession.
If you paid a fee for obtaining a copy of or access to a Project
Gutenberg-tm electronic work and you do not agree to be bound by the
terms of this agreement, you may obtain a refund from the person or
entity to whom you paid the fee as set forth in paragraph 1.E.8.
1.B. "Project Gutenberg" is a registered trademark. It may only be
used on or associated in any way with an electronic work by people who
agree to be bound by the terms of this agreement. There are a few
things that you can do with most Project Gutenberg-tm electronic works
even without complying with the full terms of this agreement. See
paragraph 1.C below. There are a lot of things you can do with Project
Gutenberg-tm electronic works if you follow the terms of this agreement
and help preserve free future access to Project Gutenberg-tm electronic
works. See paragraph 1.E below.
1.C. The Project Gutenberg Literary Archive Foundation ("the Foundation"
or PGLAF), owns a compilation copyright in the collection of Project
Gutenberg-tm electronic works. Nearly all the individual works in the
collection are in the public domain in the United States. If an
individual work is in the public domain in the United States and you are
located in the United States, we do not claim a right to prevent you from
copying, distributing, performing, displaying or creating derivative
works based on the work as long as all references to Project Gutenberg
are removed. Of course, we hope that you will support the Project
Gutenberg-tm mission of promoting free access to electronic works by
freely sharing Project Gutenberg-tm works in compliance with the terms of
this agreement for keeping the Project Gutenberg-tm name associated with
the work. You can easily comply with the terms of this agreement by
keeping this work in the same format with its attached full Project
Gutenberg-tm License when you share it without charge with others.
1.D. The copyright laws of the place where you are located also govern
what you can do with this work. Copyright laws in most countries are in
a constant state of change. If you are outside the United States, check
the laws of your country in addition to the terms of this agreement
before downloading, copying, displaying, performing, distributing or
creating derivative works based on this work or any other Project
Gutenberg-tm work. The Foundation makes no representations concerning
the copyright status of any work in any country outside the United
States.
1.E. Unless you have removed all references to Project Gutenberg:
1.E.1. The following sentence, with active links to, or other immediate
access to, the full Project Gutenberg-tm License must appear prominently
whenever any copy of a Project Gutenberg-tm work (any work on which the
phrase "Project Gutenberg" appears, or with which the phrase "Project
Gutenberg" is associated) is accessed, displayed, performed, viewed,
copied or distributed:
This eBook is for the use of anyone anywhere at no cost and with
almost no restrictions whatsoever. You may copy it, give it away or
re-use it under the terms of the Project Gutenberg License included
with this eBook or online at www.gutenberg.org
1.E.2. If an individual Project Gutenberg-tm electronic work is derived
from the public domain (does not contain a notice indicating that it is
posted with permission of the copyright holder), the work can be copied
and distributed to anyone in the United States without paying any fees
or charges. If you are redistributing or providing access to a work
with the phrase "Project Gutenberg" associated with or appearing on the
work, you must comply either with the requirements of paragraphs 1.E.1
through 1.E.7 or obtain permission for the use of the work and the
Project Gutenberg-tm trademark as set forth in paragraphs 1.E.8 or
1.E.9.
1.E.3. If an individual Project Gutenberg-tm electronic work is posted
with the permission of the copyright holder, your use and distribution
must comply with both paragraphs 1.E.1 through 1.E.7 and any additional
terms imposed by the copyright holder. Additional terms will be linked
to the Project Gutenberg-tm License for all works posted with the
permission of the copyright holder found at the beginning of this work.
1.E.4. Do not unlink or detach or remove the full Project Gutenberg-tm
License terms from this work, or any files containing a part of this
work or any other work associated with Project Gutenberg-tm.
1.E.5. Do not copy, display, perform, distribute or redistribute this
electronic work, or any part of this electronic work, without
prominently displaying the sentence set forth in paragraph 1.E.1 with
active links or immediate access to the full terms of the Project
Gutenberg-tm License.
1.E.6. You may convert to and distribute this work in any binary,
compressed, marked up, nonproprietary or proprietary form, including any
word processing or hypertext form. However, if you provide access to or
distribute copies of a Project Gutenberg-tm work in a format other than
"Plain Vanilla ASCII" or other format used in the official version
posted on the official Project Gutenberg-tm web site (www.gutenberg.org),
you must, at no additional cost, fee or expense to the user, provide a
copy, a means of exporting a copy, or a means of obtaining a copy upon
request, of the work in its original "Plain Vanilla ASCII" or other
form. Any alternate format must include the full Project Gutenberg-tm
License as specified in paragraph 1.E.1.
1.E.7. Do not charge a fee for access to, viewing, displaying,
performing, copying or distributing any Project Gutenberg-tm works
unless you comply with paragraph 1.E.8 or 1.E.9.
1.E.8. You may charge a reasonable fee for copies of or providing
access to or distributing Project Gutenberg-tm electronic works provided
that
- You pay a royalty fee of 20% of the gross profits you derive from
the use of Project Gutenberg-tm works calculated using the method
you already use to calculate your applicable taxes. The fee is
owed to the owner of the Project Gutenberg-tm trademark, but he
has agreed to donate royalties under this paragraph to the
Project Gutenberg Literary Archive Foundation. Royalty payments
must be paid within 60 days following each date on which you
prepare (or are legally required to prepare) your periodic tax
returns. Royalty payments should be clearly marked as such and
sent to the Project Gutenberg Literary Archive Foundation at the
address specified in Section 4, "Information about donations to
the Project Gutenberg Literary Archive Foundation."
- You provide a full refund of any money paid by a user who notifies
you in writing (or by e-mail) within 30 days of receipt that s/he
does not agree to the terms of the full Project Gutenberg-tm
License. You must require such a user to return or
destroy all copies of the works possessed in a physical medium
and discontinue all use of and all access to other copies of
Project Gutenberg-tm works.
- You provide, in accordance with paragraph 1.F.3, a full refund of any
money paid for a work or a replacement copy, if a defect in the
electronic work is discovered and reported to you within 90 days
of receipt of the work.
- You comply with all other terms of this agreement for free
distribution of Project Gutenberg-tm works.
1.E.9. If you wish to charge a fee or distribute a Project Gutenberg-tm
electronic work or group of works on different terms than are set
forth in this agreement, you must obtain permission in writing from
both the Project Gutenberg Literary Archive Foundation and Michael
Hart, the owner of the Project Gutenberg-tm trademark. Contact the
Foundation as set forth in Section 3 below.
1.F.
1.F.1. Project Gutenberg volunteers and employees expend considerable
effort to identify, do copyright research on, transcribe and proofread
public domain works in creating the Project Gutenberg-tm
collection. Despite these efforts, Project Gutenberg-tm electronic
works, and the medium on which they may be stored, may contain
"Defects," such as, but not limited to, incomplete, inaccurate or
corrupt data, transcription errors, a copyright or other intellectual
property infringement, a defective or damaged disk or other medium, a
computer virus, or computer codes that damage or cannot be read by
your equipment.
1.F.2. LIMITED WARRANTY, DISCLAIMER OF DAMAGES - Except for the "Right
of Replacement or Refund" described in paragraph 1.F.3, the Project
Gutenberg Literary Archive Foundation, the owner of the Project
Gutenberg-tm trademark, and any other party distributing a Project
Gutenberg-tm electronic work under this agreement, disclaim all
liability to you for damages, costs and expenses, including legal
fees. YOU AGREE THAT YOU HAVE NO REMEDIES FOR NEGLIGENCE, STRICT
LIABILITY, BREACH OF WARRANTY OR BREACH OF CONTRACT EXCEPT THOSE
PROVIDED IN PARAGRAPH F3. YOU AGREE THAT THE FOUNDATION, THE
TRADEMARK OWNER, AND ANY DISTRIBUTOR UNDER THIS AGREEMENT WILL NOT BE
LIABLE TO YOU FOR ACTUAL, DIRECT, INDIRECT, CONSEQUENTIAL, PUNITIVE OR
INCIDENTAL DAMAGES EVEN IF YOU GIVE NOTICE OF THE POSSIBILITY OF SUCH
DAMAGE.
1.F.3. LIMITED RIGHT OF REPLACEMENT OR REFUND - If you discover a
defect in this electronic work within 90 days of receiving it, you can
receive a refund of the money (if any) you paid for it by sending a
written explanation to the person you received the work from. If you
received the work on a physical medium, you must return the medium with
your written explanation. The person or entity that provided you with
the defective work may elect to provide a replacement copy in lieu of a
refund. If you received the work electronically, the person or entity
providing it to you may choose to give you a second opportunity to
receive the work electronically in lieu of a refund. If the second copy
is also defective, you may demand a refund in writing without further
opportunities to fix the problem.
1.F.4. Except for the limited right of replacement or refund set forth
in paragraph 1.F.3, this work is provided to you 'AS-IS' WITH NO OTHER
WARRANTIES OF ANY KIND, EXPRESS OR IMPLIED, INCLUDING BUT NOT LIMITED TO
WARRANTIES OF MERCHANTIBILITY OR FITNESS FOR ANY PURPOSE.
1.F.5. Some states do not allow disclaimers of certain implied
warranties or the exclusion or limitation of certain types of damages.
If any disclaimer or limitation set forth in this agreement violates the
law of the state applicable to this agreement, the agreement shall be
interpreted to make the maximum disclaimer or limitation permitted by
the applicable state law. The invalidity or unenforceability of any
provision of this agreement shall not void the remaining provisions.
1.F.6. INDEMNITY - You agree to indemnify and hold the Foundation, the
trademark owner, any agent or employee of the Foundation, anyone
providing copies of Project Gutenberg-tm electronic works in accordance
with this agreement, and any volunteers associated with the production,
promotion and distribution of Project Gutenberg-tm electronic works,
harmless from all liability, costs and expenses, including legal fees,
that arise directly or indirectly from any of the following which you do
or cause to occur: (a) distribution of this or any Project Gutenberg-tm
work, (b) alteration, modification, or additions or deletions to any
Project Gutenberg-tm work, and (c) any Defect you cause.
Section 2. Information about the Mission of Project Gutenberg-tm
Project Gutenberg-tm is synonymous with the free distribution of
electronic works in formats readable by the widest variety of computers
including obsolete, old, middle-aged and new computers. It exists
because of the efforts of hundreds of volunteers and donations from
people in all walks of life.
Volunteers and financial support to provide volunteers with the
assistance they need, are critical to reaching Project Gutenberg-tm's
goals and ensuring that the Project Gutenberg-tm collection will
remain freely available for generations to come. In 2001, the Project
Gutenberg Literary Archive Foundation was created to provide a secure
and permanent future for Project Gutenberg-tm and future generations.
To learn more about the Project Gutenberg Literary Archive Foundation
and how your efforts and donations can help, see Sections 3 and 4
and the Foundation web page at http://www.pglaf.org.
Section 3. Information about the Project Gutenberg Literary Archive
Foundation
The Project Gutenberg Literary Archive Foundation is a non profit
501(c)(3) educational corporation organized under the laws of the
state of Mississippi and granted tax exempt status by the Internal
Revenue Service. The Foundation's EIN or federal tax identification
number is 64-6221541. Its 501(c)(3) letter is posted at
http://pglaf.org/fundraising. Contributions to the Project Gutenberg
Literary Archive Foundation are tax deductible to the full extent
permitted by U.S. federal laws and your state's laws.
The Foundation's principal office is located at 4557 Melan Dr. S.
Fairbanks, AK, 99712., but its volunteers and employees are scattered
throughout numerous locations. Its business office is located at
809 North 1500 West, Salt Lake City, UT 84116, (801) 596-1887, email
[email protected]. Email contact links and up to date contact
information can be found at the Foundation's web site and official
page at http://pglaf.org
For additional contact information:
Dr. Gregory B. Newby
Chief Executive and Director
[email protected]
Section 4. Information about Donations to the Project Gutenberg
Literary Archive Foundation
Project Gutenberg-tm depends upon and cannot survive without wide
spread public support and donations to carry out its mission of
increasing the number of public domain and licensed works that can be
freely distributed in machine readable form accessible by the widest
array of equipment including outdated equipment. Many small donations
($1 to $5,000) are particularly important to maintaining tax exempt
status with the IRS.
The Foundation is committed to complying with the laws regulating
charities and charitable donations in all 50 states of the United
States. Compliance requirements are not uniform and it takes a
considerable effort, much paperwork and many fees to meet and keep up
with these requirements. We do not solicit donations in locations
where we have not received written confirmation of compliance. To
SEND DONATIONS or determine the status of compliance for any
particular state visit http://pglaf.org
While we cannot and do not solicit contributions from states where we
have not met the solicitation requirements, we know of no prohibition
against accepting unsolicited donations from donors in such states who
approach us with offers to donate.
International donations are gratefully accepted, but we cannot make
any statements concerning tax treatment of donations received from
outside the United States. U.S. laws alone swamp our small staff.
Please check the Project Gutenberg Web pages for current donation
methods and addresses. Donations are accepted in a number of other
ways including checks, online payments and credit card donations.
To donate, please visit: http://pglaf.org/donate
Section 5. General Information About Project Gutenberg-tm electronic
works.
Professor Michael S. Hart is the originator of the Project Gutenberg-tm
concept of a library of electronic works that could be freely shared
with anyone. For thirty years, he produced and distributed Project
Gutenberg-tm eBooks with only a loose network of volunteer support.
Project Gutenberg-tm eBooks are often created from several printed
editions, all of which are confirmed as Public Domain in the U.S.
unless a copyright notice is included. Thus, we do not necessarily
keep eBooks in compliance with any particular paper edition.
Most people start at our Web site which has the main PG search facility:
http://www.gutenberg.org
This Web site includes information about Project Gutenberg-tm,
including how to make donations to the Project Gutenberg Literary
Archive Foundation, how to help produce our new eBooks, and how to
subscribe to our email newsletter to hear about new eBooks.
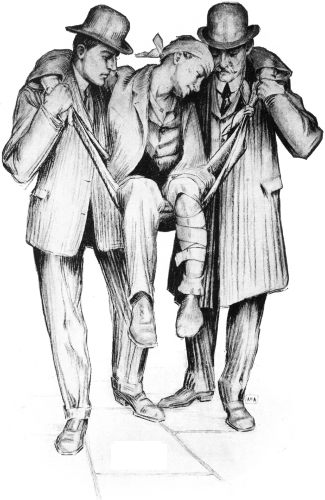 A DESIRABLE METHOD OF CARRYING THE INJURED.
A DESIRABLE METHOD OF CARRYING THE INJURED.